2014 年 79 巻 1 号 p. 180-184
2014 年 79 巻 1 号 p. 180-184
Background: There is currently a well-established network for the allocation of donor organs for transplantation in Japan, and emergency patients are often transported by the “Doctor Helicopter”. However, interhospital transfer of patients, which can require aircraft with specialized equipment, depends on arrangement by each responsible hospital.
Methods and Results: Since 2009 there were 41 interhospital aviation transfers of pediatric patients with intractable cardiac or airway diseases seeking surgical treatment at Sakakibara Heart Institute. Of these, 22 were newborns, 21 were on continuous drip infusion and 14 on mechanical ventilator support. In 15 cases (36.6%), a commercial airliner was used, with the remaining using chartered emergency aircraft (eg, local fire department helicopter, Self-Defense-Forces of Japan and the Doctor Helicopter). The median transfer time was 239 min for commercial airliners, 51 min for chartered aircraft departing directly from the referring hospital and 120.5 min for chartered aircraft departing from a nearby location. The efficiency of the transfer exemplified by the percentage of the time on board the aircraft was significantly lower for commercial airliners compared with chartered emergency aircraft.
Conclusions: Further efforts and cooperation with government are required to obtain geographically uniform availability of carriers with optimal medical equipment to improve pediatric patient outcomes. (Circ J 2015; 79: 180–184)
In Japan, the allocation of transplant donor organs by aircraft is well established under the supervision of organ sharing networks. Also, emergency cases in areas distant from medical services are often transferred by a “Doctor Helicopter” of the prefecture.
Pediatric patients with severe cardiac or respiratory problems may require interhospital transfer to receive a higher standard of surgical care. These patients are often small infants, critically ill, and on mechanical ventilator support, carrying certain risks even with the attendance of a specialized medical team. Presently, however, this type of transfer is arranged by each responsible hospital and often relies on commercial airliners, which can involve extra time spent waiting for the arrival of the carrier.
Another option in this context is to charter other emergency aircraft, such as firefighting or rescue helicopter (local fire departments or governments) or military aircraft (the Self-Defense-Forces of Japan). Recent legislation towards creating organizations providing airborne ambulances (such as the “Doctor Helicopter”) was introduced by a Diet member in 2007. In Hokkaido fixed-wing ambulance aircraft are also available and run by “Medical Wings”, a local research institute. However, the availability of these emergency aircraft is limited.
We describe the incidence, demographics and duration of interhospital patient transfers and also the clinical course of pediatric patients having cardiac or airway disease and using various airborne carriers.
The Sakakibara Heart Institute is in the city of Fuchu, Tokyo. Tokyo is approximately 1,100 km from the northern point of Hokkaido and 2,000 km from the southern point of Okinawa. The linear distance of the hospital from Tokyo international airport and Chofu airport is 27.1 km and 1.2 km, respectively. From Iruma and Fuchu airbases, owned by the Self-Defense-Force, the distance is 22.0 km and 2.5 km, respectively. The main activity of the Chofu airport, administered by the Tokyo Metropolitan Government, is to provide a runway for commercial as well as private aircraft. It also accepts airborne ambulances upon request.
From March 2009 to January 2014, 41 pediatric cases with cardiac or airway diseases requiring surgical care underwent interhospital transfer using airborne carriers. During the same time period, there were 1,828 admissions to Sakakibara Heart Institute seeking surgical care. Therefore, airborne interhospital transfer represents 2.2% of all admissions for pediatric cardiac or airway surgery. Parametric comparisons were performed between the main cohort of 41 admissions vs. other types of admissions (1,828−41=1,787 admissions).
In 15 cases (36.6%), a commercial airliner was used and of the remaining, chartered aircraft were used, including local fire department helicopters (19), “Doctor Helicopter” (4) and aircraft of the Self-Defense-Forces of Japan (3).
The patient’s status in the referring hospitals was: newborn awaiting surgical intervention (23), in-hospital care required for heart failure (12), and in-hospital care required for airway obstruction (6). Age and body weight at admission were 0.5 (0–65.4) months and 3.1 (2.3–17.3) kg, respectively. The chief clinical problem in the cohort was cardiac in 35 admissions and a combination of cardiac and airway in 6; 28 had cyanotic heart disease (Table 1). Noncardiac abnormalities included 2 each of 22q11 deletion, chromosomal abnormalities other than 22q11 deletion and unspecified multiple surface abnormalities; and 1 each of asplenia, Down syndrome, diaphragmatic hernia and persistent cloaca; 14 patients (34.2%) were on a ventilator at the time of admission and 4 of them had undergone tracheostomy. Patients were receiving continuous infusions of lipo-prostaglandin (19), phosphodiesterase inhibitor (2) and prostaglandin-E1 (1).
| Diagnosis | n |
|---|---|
| Hypoplastic left heart syndrome and variants | 12 |
| Ventricular septal defect (with CoA/interrupted aortic arch) | 5 (3) |
| Pulmonary atresia/stenosis with ventricular septal defect | 5 |
| Transposition of the great arteries/Taussig-Bing anomaly (with CoA) | 4 (1) |
| Functionally single ventricle (with TAPVC) | 3 (1) |
| Truncus arteriosus | 3 |
| Mitral valve regurgitation | 3 |
| Pulmonary arterial sling | 2 |
| Atrial septal defect with partial anomalous pulmonary venous connection | 2 |
| Tetralogy of Fallot | 1 |
| Isolated TAPVC | 1 |
CoA, coarctation of the aorta; TAPVC, total anomalous pulmonary venous connection.
This study was a retrospective chart review from March 2009 through February 2014. A questionnaire was sent to all 19 referring hospitals to retrieve information including departure time, means of transfer, departure place, and arrival time at the airport in Tokyo. A reply was sent from 15 hospitals (78.9%). Data are presented as median with range. Student’s t-test or one-way analysis of variance was used to analyze intergroup difference of continuous variables. Categorical variables were compared using the χ2 test. Statistical analysis was performed with JMP® software for Macintosh, 10.0.2 (SAS Institute Inc, Cary, NC, USA).
On admission to the Institute, the patients’ laboratory study values often deviated from the normal range (Table 2). Of note, the patient transferred from the farthest hospital (946.3 km distance) by commercial airliner exhibited deteriorated dehydration during the transfer, with serum sodium and blood urea nitrogen levels upon arrival of 172 mmol/L and 117.8 mg/dl, respectively. Operations were performed on an emergency basis in 6 (14.6%). For those requiring cardiopulmonary bypass, the perfusion and ischemic times were 100 (47–192) and 59 (0–116) min, respectively. The lengths of stay in the intensive care unit and hospital were 6 (1–63) and 30.5 (7–132) days. The principal operation during the admission was cardiac in 35 cases, cardiac plus airway (external stenting) in 3, airway in 2, and diaphragmatic plication in 1 (Table 3). The site of the airway obstruction was trachea in 3 and left bronchus in 2. Besides these principal operations, a total of 31 additional procedures were performed for 19 admissions (once for 11 admissions, twice for 6, three times for 1 and five times for 1). Details of these operations are listed in Table 4. The rate of requiring delayed sternal closure was 29.3% (12 of 41 admissions) compared with 4.3% (77 of 1,787 admissions) of the other admissions (P<0.05). In addition, 2 patients required extracorporeal membrane oxygenation (4.9%).
| Laboratory data | n | Median | Range | Deviation from normal |
Percentage (%) |
|---|---|---|---|---|---|
| Blood oxygen saturation (%) | 41 | 87 | 55~100 | <60 | 3 (7.3) |
| pH | 40 | 7.40 | 7.16~7.63 | <7.3 | 3 (7.5) |
| Partial oxygen pressure (mmHg) | 40 | 38.0 | 17.4~314 | <30 | 8 (20.0) |
| Partial carbon dioxide pressure (mmHg) | 40 | 43.0 | 23.2~104 | >50 | 10 (25.0) |
| Base excess (mEq/L) | 40 | 1.0 | −8.0~11.4 | <−3 | 5 (12.5) |
| Lactate (mmol/L) | 40 | 1.6 | 0.3~8.5 | >4 | 6 (15.0) |
| Hemoglobin (g/dl) | 41 | 14.3 | 9.5~18.0 | <11 | 4 (9.8) |
| Hematocrit (%) | 41 | 42.6 | 27.7~54.2 | <32 | 2 (4.9) |
| White blood cell count (×103/μl) | 41 | 9.9 | 5.3~32.0 | >20 | 6 (14.6) |
| Platelet count (/μl) | 41 | 289 | 56~549 | <120 | 3 (7.3) |
| Total protein (g/dl) | 41 | 5.6 | 4.3~8.2 | <5 | 6 (14.6) |
| Albumin (g/dl) | 41 | 3.8 | 2.8~5.5 | <3.5 | 8 (19.5) |
| Aspartate aminotransferase (IU/L) | 41 | 29 | 17~774 | >120 | 3 (7.3) |
| Alanine aminotransferase (IU/L) | 41 | 12 | 3~355 | >60 | 3 (7.3) |
| Lactate dehydrogenase (IU/L) | 41 | 352 | 201~3,220 | >800 | 4 (9.8) |
| Blood urea nitrogen (mg/dl) | 41 | 10.2 | 2.3~117.8 | >20 | 6 (14.6) |
| Creatinine (mg/dl) | 41 | 0.41 | 0.15~1.74 | >1.2 | 4 (9.8) |
| Sodium (mmol/L) | 41 | 138 | 125~172 | >150 | 1 (2.4) |
| Chloride (mmol/L) | 41 | 102 | 84~134 | <90, >120 | 2 (4.9) |
| Total bilirubin (mg/dl) | 41 | 2.0 | 0.2~16.6 | >12.5 | 4 (9.8) |
| C-reactive protein (mg/dl) | 41 | 0.1 | 0~5.0 | >5 | 1 (2.4) |
| Norwood operation | 7 |
| Systemic-to-pulmonary shunt±PA plasty | 6 |
| Pulmonary arterial banding | 5 |
| Arterial switch operation | 4 |
| Coarctation or interruption of the aorta with VSD repair | 3 |
| Mitral valve repair or replacement | 3 |
| Total APVC repair±PA banding/systemic-to-pulmonary shunt | 2 |
| Bidirectional cavopulmonary anastomosis | 2 |
| VSD closure | 2 |
| PA sling repair | 2 |
| Tetralogy of Fallot repair | 1 |
| Atrial septal defect with partial APVC repair | 1 |
APVC, anomalous pulmonary venous connection; PA, pulmonary arterial; S-P, systemic-to-pulmonary; VSD, ventricular septal defect.
| Delayed sternal closure | 12 |
| Pulmonary arterial banding | 4 |
| Systemic-to-pulmonary arterial shunt | 3 |
| Atrioventricular valve repair or replacement | 3 |
| Diaphragmatic plication | 2 |
| Institution of extracorporeal membrane oxygenation | 2 |
| Supra aortic stenosis repair | 1 |
| Jejunostomy creation | 1 |
| Pacemaker insertion | 1 |
| Emergency mediastinal exploration | 1 |
| Occlusion of major atriopulmonary collateral | 1 |
The postoperative events included 2 cases of atrial tachyarrhythmia and 1 each of phrenic nerve injury, cerebral infarction and complete atrioventricular block. There was 1 in-hospital (2.4%) and 1 late death; 13 (31.7%) patients were repatriated to the referring hospitals.
From the questionnaires returned from the referring hospitals, complete datasets including total time of transfer and the time on the aircraft were harvested for 29 admissions (Figures 1–3).
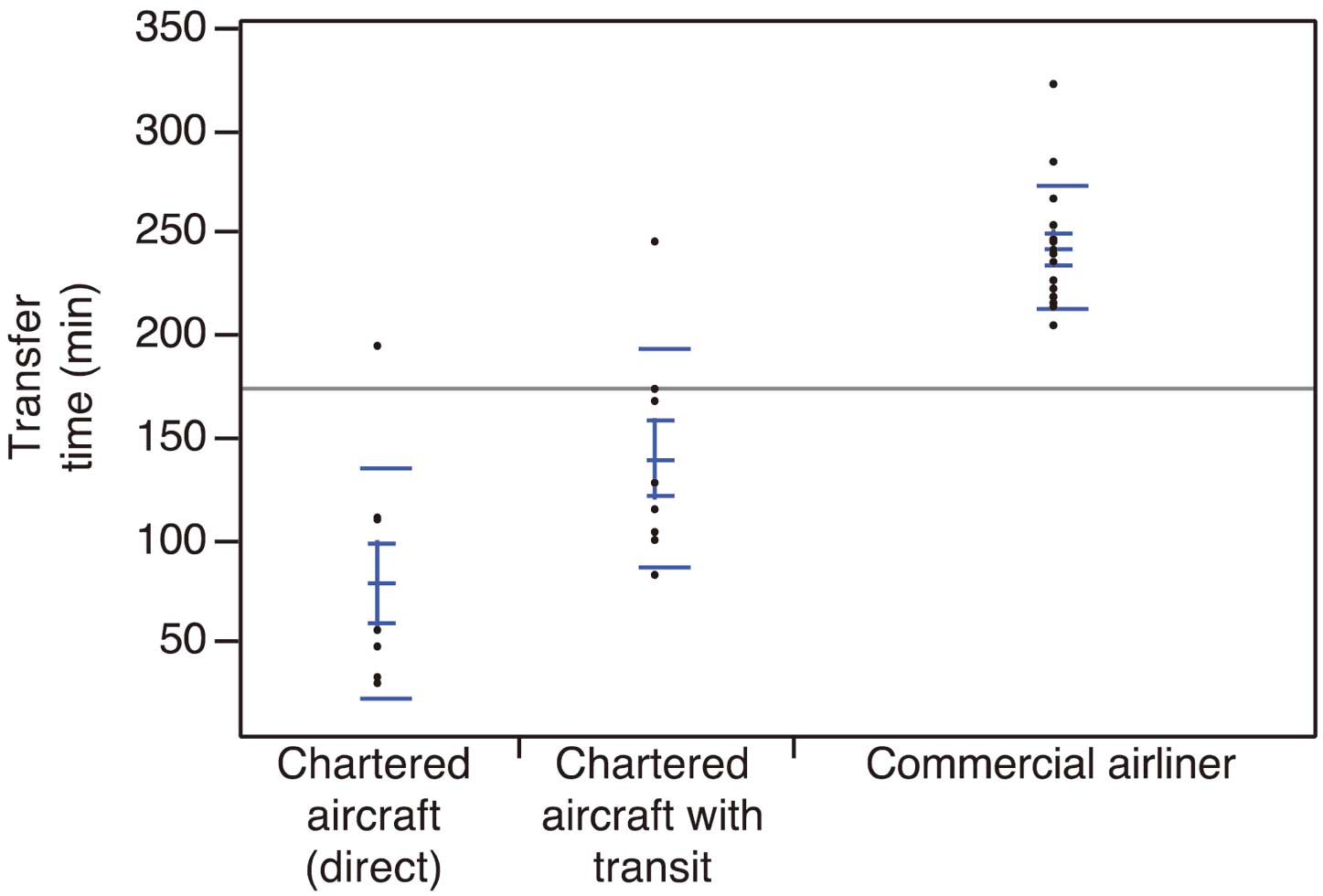
Scattergram of the total time of transfer with: chartered aircraft departing from the referring hospital (direct, n=8), chartered aircraft departing from a nearby location (n=8) and a commercial airliner (n=13). Bars indicate the mean, standard deviation, and 95% confidence interval. The median time was 51 (29–194), 120.5 (82–245) and 239 (204–322) min, respectively. All parameters were considered significantly different between the groups with a P-value <0.05.
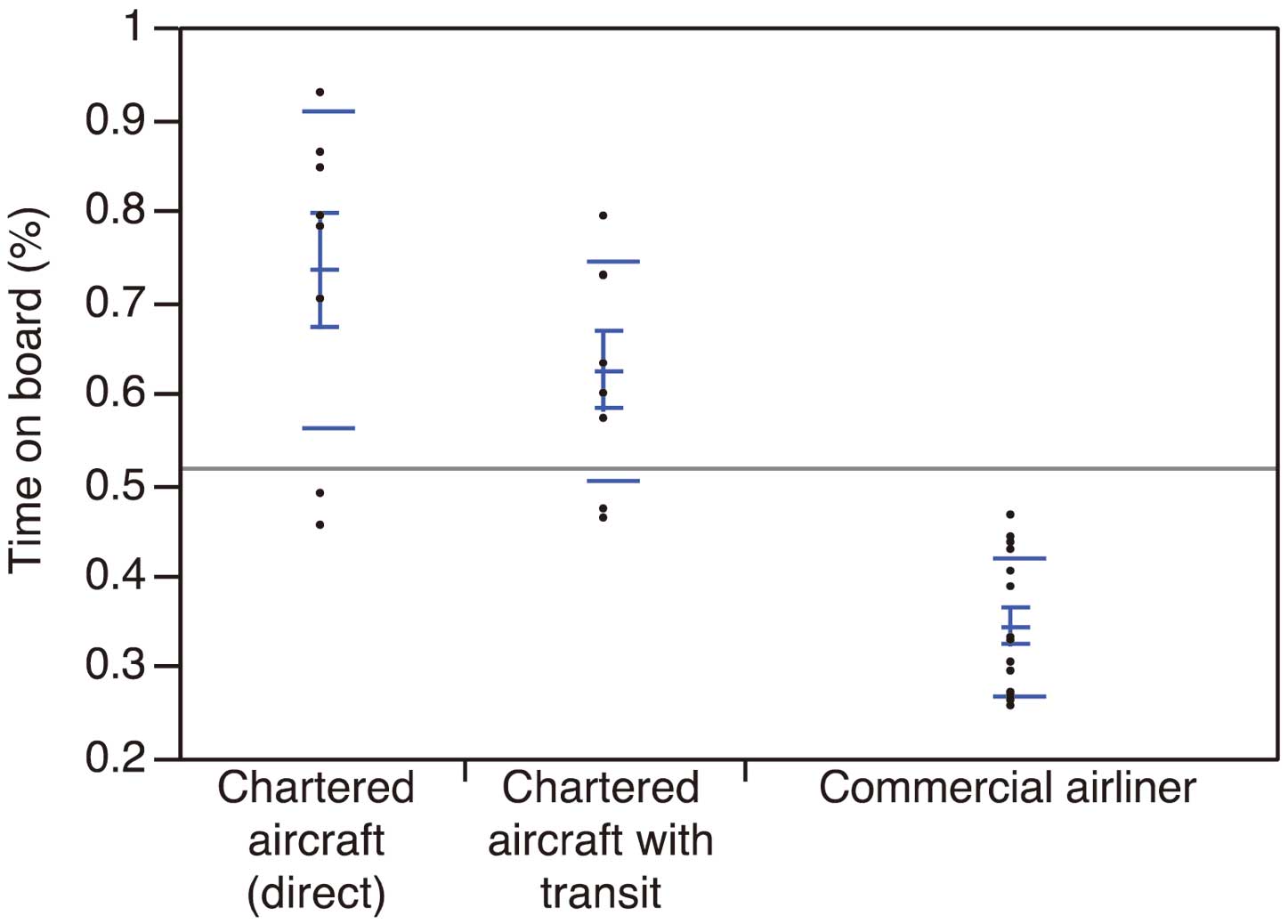
Scattergram of the percentage of time on board the aircraft or train per total transfer time for the 3 groups. The percentage of time on board is (time on board aircraft)/(total transfer time). The median percentage was 79 (45–93), 62 (46–79) and 33 (26–47), respectively. The former 2 parameters were considered significantly different from the last 1 with a P-value <0.05.

Scattergram of the linear distance between the referring hospital and the Sakakibara Heart Institute for the 3 groups. The median value was 80 (30–456), 241 (60–946) and 561 (456–929) km, respectively. The former 2 parameters were considered significantly different from the last 1 with a P-value <0.05.
Interhospital transfer of critically ill patients poses difficulties for medical staff, especially so for pediatric cardiac and airway diseases, which are highly specialized fields. It is known that the geographical disparity in the pediatric healthcare system is greater than that of adults.1 These patients, consequently, may require long-distance interhospital transfer to obtain a sufficiently high standard of care: the patient group described here included a high percentage of newborns, patients with continuous drip infusion and on mechanical ventilator support. Underscoring the severity of this patient cohort, the requirements for delayed sternal closure and extracorporeal membrane oxygenation were higher compared with other surgical patients at the same hospital. Data from North America reveal that the final surgical outcome of transported small children is significantly affected by the distance traveled.2,3 Transfer can be more problematic when the patient is on a mechanical ventilator, with a serious consequence being the occlusion or unintended extubation of the endotracheal tube.4,5 It is, therefore, especially important that the patient be attended by a specialized pediatric team.6
For safe transfer, appropriate equipment is also required, including a vital signs monitor, defibrillator, ventilator, oxygen source, suction unit, resuscitation chart and a communication system.7 Clearly, an airborne ambulance is the ideal for the storage and use of this equipment, and should be the first option. Data from the USA of interhospital extracorporeal membrane oxygenation transport revealed that transport was carried out by airborne ambulance in 87.5% of cases.8 In Japan, the Fire Defense Act amended in 1963 assigned ambulance service responsibilities to Fire Defense organizations, providing a well-established ground ambulance system covering the entire nation.9,10 On the other hand, the airborne ambulance system has only recently started operating, being also known as “Doctor Helicopters”. In order to promote deployment of the Doctor Helicopter, the Act on Special Measures Concerning Securing of Helicopter Emergency Medical Services (Doctor Helicopter Special Act) was enacted in 2007. In 2008, the Parliamentary Group for the Promotion of Doctor Helicopters was formed as a bipartisan group of 140 Parliament members. Doctor Helicopters have been distributed to each prefecture nationwide, which has shortened the time interval for transfer of emergency patients in comparison to ground ambulance.11–15 Also, in Hokkaido, there is an organization (Medical Wings) doing research on and administrating fixed-wing aircraft carrying medical equipment, with patient transfer being the first priority. According to their operational experience report, the organization is funded by donations and subsidies from the local government and administered by local medical institutions. However, these airborne ambulances are presently not commonly used for regular interhospital transfers.
The use of a firefighting or rescue helicopter is another option for interhospital transfer and is a well-established practice in some countries. For example, the Swiss helicopter rescue service transported 656 children in a 1-year period, including 241 interhospital transfers.16 Although not designed for medical transfer and lacking sufficient medical equipment, these helicopters may offer the fastest access from hospital to hospital. Also, the aero-medical squadron of the Japan Self-Defense Forces provides aircraft for long-distance transfer of patients per request by the governor of the municipal government, stipulated in the Article 83 of the Japanese Self-Defense Forces Act. In the year 2013, 341 patient transfers were conducted (http://www.mod.go.jp/j/press/news/2011/01/12b.html).
However, these transport resources are limited and not uniformly available, differing greatly among the geographical regions of Japan. Therefore, 36.6% of patients in this study used a commercial airliner for transfer, which can be a choice for a stable patient, but for critically ill children, it can be problematic because of the need to wait for the carrier’s arrival. Indeed, the time efficiency of the transfer exemplified by the percentage of the time on board aircraft was significantly lower for commercial airliners compared with chartered emergency aircrafts. This fact sheds light on the underdeveloped standards of interhospital transfer of critically ill patients in Japan. It is therefore vital to obtain geographically uniform availability of carriers with optimal medical equipment providing the fastest access. For this purpose, further efforts and cooperation with government are required to optimize transport systems and processes.
We thank all medical staff of the referring hospitals who kindly responded to the questionnaires.