Vulnerable or high-risk atherosclerotic plaque is prone to rupture and to thus cause acute coronary syndrome, but detecting this plaque on coronary plaque imaging has been challenging.1
In previous studies we described the characteristics of coronary high-intensity plaque (HIP) on non-contrast T1-weighted magnetic resonance imaging (T1WI),2,3
and showed that this plaque was associated with the slow- or no-reflow phenomenon and with periprocedural myocardial injuries during elective percutaneous coronary intervention (PCI), as well as with future coronary events.2,4,5
High-spatial-resolution 3.0-T magnetic resonance imaging (MRI) of carotid plaques had substantial improvement in imaging quality and signal-to-noise and contrast-to-noise ratios compared with 1.5-T MRI.6
Few studies, however, have involved coronary plaque imaging using non-contrast T1WI with 3.0-T clinical MRI.
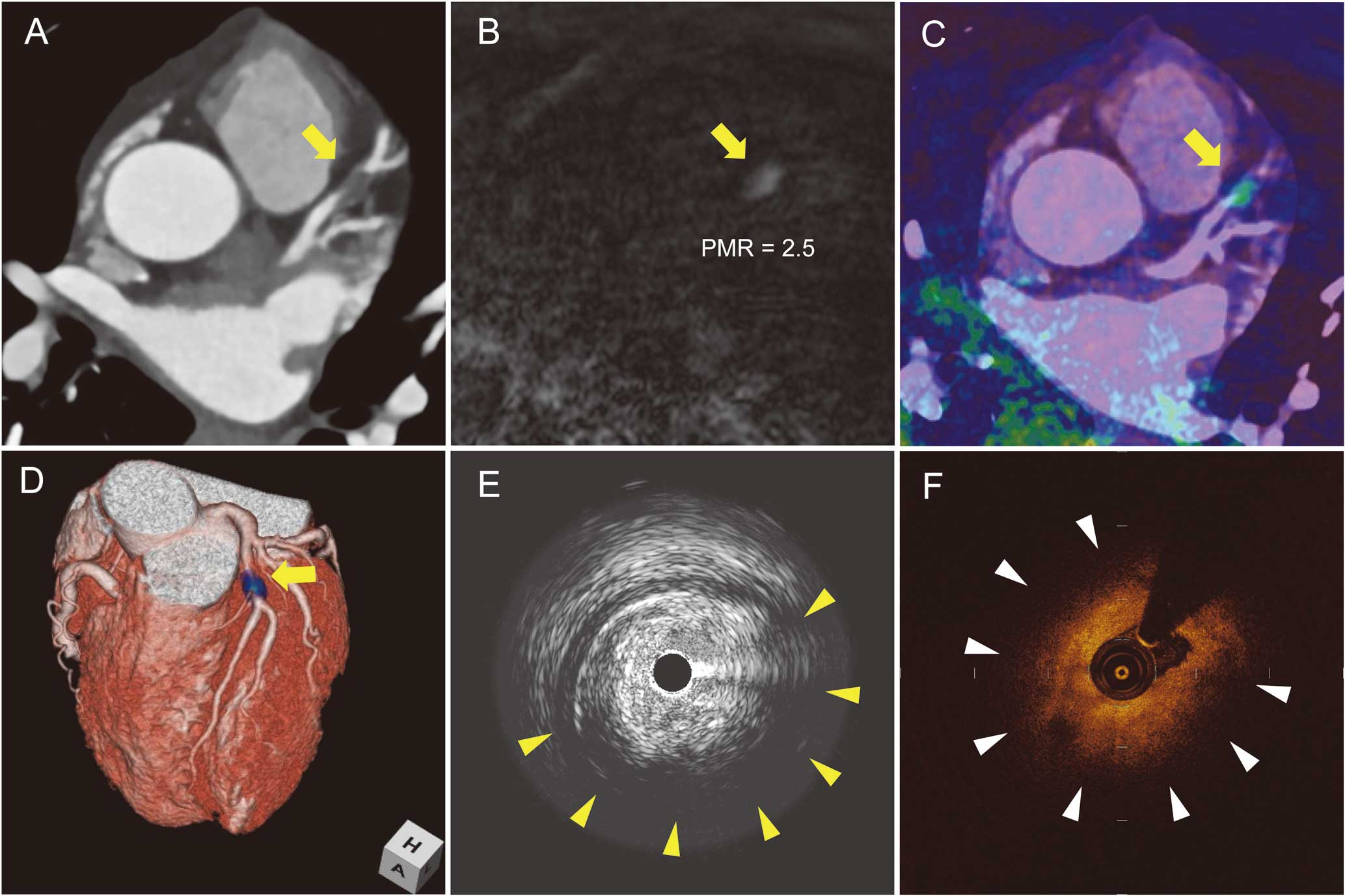
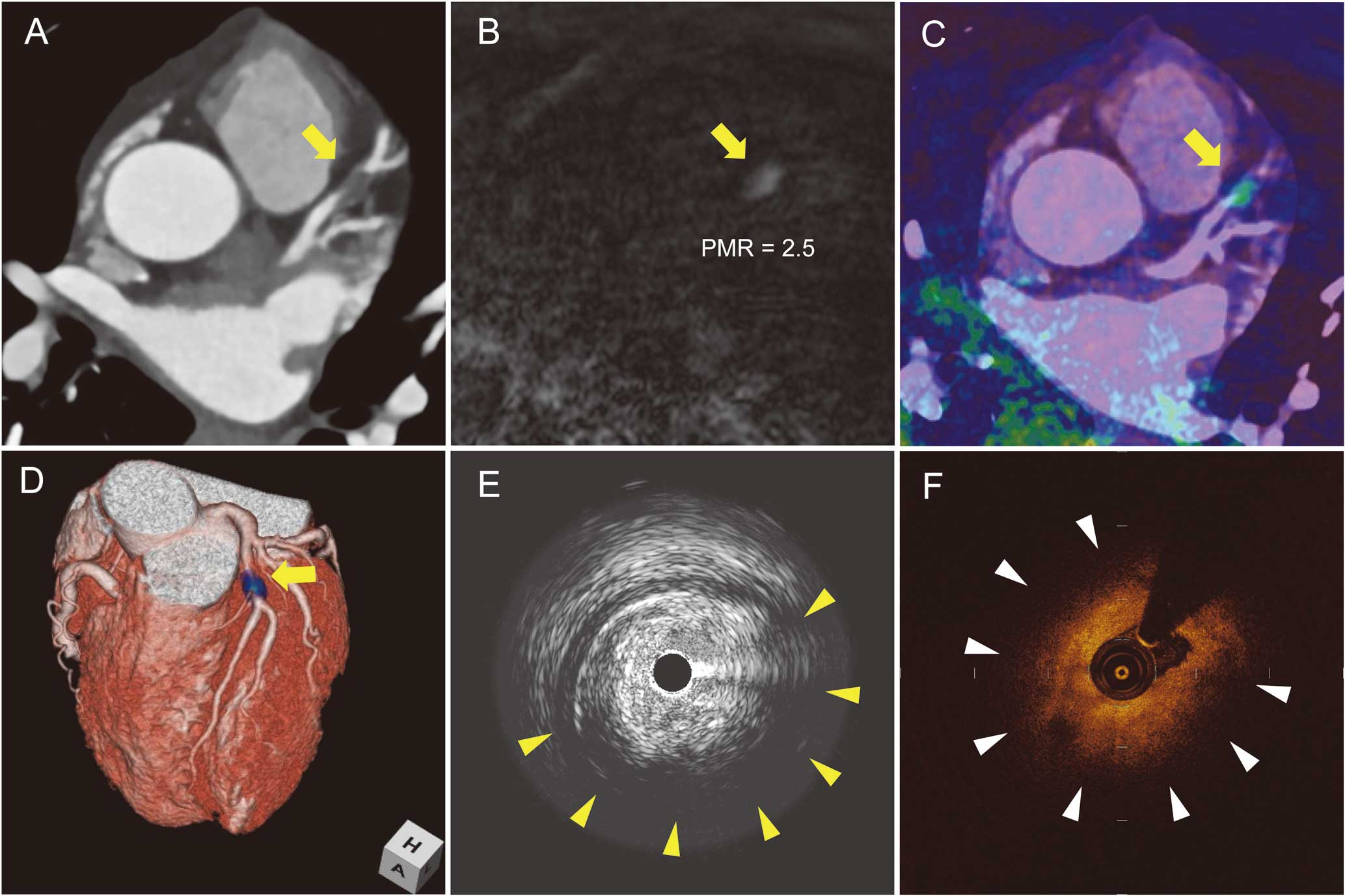
In a 46-year-old man with stable effort angina pectoris, coronary computed tomography angiography showed significant stenosis with a low-density coronary plaque and positive vessel remodeling in the proximal portion of the left anterior descending artery (LAD;
Figure 1A;
Movie S1). Non-contrast T1WI was done on 3.0-T MRI with a 32-channel cardiac coil (MAGNETOM Verio; Siemens AG Healthcare Sector, Erlangen, Germany). Coronary plaque imaging was performed using an inversion recovery-prepared 3-D T1W turbo fast low-angle shot sequence with an electrocardiographic trigger, navigator-gated free-breathing, and fat suppression, with transaxial sections covering the whole heart (inversion time, 650 ms; field of view, 280×228 mm; acquisition matrix, 256×187; reconstruction matrix, 512×374; acquisition slice thickness, 1.0 mm; reconstruction spatial resolution, 0.6×0.5×0.6 mm; repetition time/echo, 4.7 ms/2.13 ms; flip angle, 12°; GRAPP factor, 2; navigator gating window, ±1.5–2.5 mm; and data acquisition window, 84–120 ms). The trigger delay and acquisition window were set based on the period of minimal right coronary artery motion as determined on cine-MRI.5
Acquisition time and navigation efficiency in this case were 15 min and 35%, respectively. The plaque-to-myocardium signal intensity ratio, defined as the signal intensity of the coronary plaque divided by that of the nearby left ventricular myocardium, was calculated to be 2.5 (Figure 1B;
Movie S2). Intravascular ultrasound showed a large intimal plaque and a region of low echogenicity that had remarkable attenuation (Figure 1E). Optical CT showed an extensive signal-poor region with low backscattering and a lipid arc of 286° (Figure 1F). The patient underwent elective PCI for proximal LAD lesion. Following the first balloon dilatation, a filling defect was observed in the distal segment of the LAD and the slow-flow phenomenon developed (Figure 2A); this defect disappeared following intra-coronary aspiration (Figure 2B). Microscopy of the aspirated specimen showed a large amount of the necrotic core with overlying platelet- and fibrin-rich thrombus (Figures 2C,D). Immunohistology confirmed numerous CD68+
macrophages within the aspirated specimen (Figures 2E,F), suggesting that the coronary embolus may have involved the large necrotic core with extensive inflammation.

In the present case, we successfully imaged coronary plaque defined as HIP on non-contrast T1WI using 3.0-T MRI. MRI was originally developed for carotid artery examinations but has emerged as a novel modality for atherosclerotic plaque characterization.7
In particular, high-intensity signals observed in carotid plaque using inversion recovery-based 3-D T1WI have been found to be associated with recent ischemic cerebrovascular events and are related to the American Heart Association classification type VI complex plaque, which is characterized by luminal surface defects, intraplaque hemorrhage, thrombus, or calcified nodules.7,8
Plaque imaging at 3.0 T is expected to provide improved imaging quality and better signal-to-noise and contrast-to-noise ratios compared with 1.5-T MRI. There have been few reports, however, of coronary artery imaging using 3.0-T MRI. Future studies comparing 1.5-T and 3.0-T MRI are warranted to assess coronary plaque.
Importantly, in this particular case, the coronary plaque defined as HIP on non-contrast T1WI at 3.0 T was associated with coronary embolus and slow flow following PCI. Specimens collected from the coronary artery contained atheroma with lipid-rich necrotic cores (Figure 2), consistent with MRI findings of hyperintense carotid plaque. Further studies are also needed to identify the plaque components of coronary HIP visualized on T1WI, and thus elucidate the mechanisms underlying acute coronary syndrome and the development of atherosclerosis.
Supplementary Files
Supplementary File 1
Movie S1. Serial imaging of the heart with enhanced computed tomography angiography showing coronary plaque with severe stenosis, positive vessel remodeling, and low plaque density at the proximal portion of the left anterior descending artery (orange arrow).
Supplementary File 2
Movie S2. Serial imaging of the heart on non-contrast T1-weighted magnetic resonance imaging at 3.0 T showing a high-intensity plaque at the proximal left anterior descending artery (orange arrow), corresponding with the lesion detected on computed tomography angiography.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-14-0897
References
- 1.
Noguchi T, Yamada N, Kawasaki T, Tanaka A, Yasuda S. Detection of high-risk atherosclerotic plaques by magnetic resonance imaging. Circ J 2013; 77: 1975–1983.
- 2.
Kawasaki T, Koga S, Koga N, Noguchi T, Tanaka H, Koga H, et al. Characterization of hyperintense plaque with noncontrast T1-weighted cardiac magnetic resonance coronary plaque imaging: Comparison with multislice computed tomography and intravascular ultrasound. JACC Cardiovasc Imaging 2009; 2: 720–728.
- 3.
Nakashima T, Noguchi T, Morita Y, Sakamoto H, Goto Y, Ishihara M, et al. Detection of intramural hematoma and serial non-contrast T1-weighted magnetic resonance imaging findings in a female patient with spontaneous coronary artery dissection. Circ J 2013; 77: 2844–2845.
- 4.
Noguchi T, Kawasaki T, Tanaka A, Yasuda S, Goto Y, Ishihara M, et al. High-intensity signals in coronary plaques on noncontrast T1-weighted magnetic resonance imaging as a novel determinant of coronary events. J Am Coll Cardiol 2014; 63: 989–999.
- 5.
Asaumi Y, Noguchi T, Morita Y, Fijiwara R, Kanaya T, Matsuyama T, et al. High-intensity plaques on noncontrast T1-weighted imaging as a predictor of periprocedural myocardial injury. JACC Cardiovasc Imaging 2014 November 26, doi:10.1016/j.jcmg.2014.07.020.
- 6.
Underhill HR, Yarnykh VL, Hatsukami TS, Wang J, Balu N, Hayes CE, et al. Carotid plaque morphology and composition: Initial comparison between 1.5- and 3.0-T magnetic field strengths. Radiology 2008; 248: 550–560.
- 7.
Moody AR, Murphy RE, Morgan PS, Martel AL, Delay GS, Allder S, et al. Characterization of complicated carotid plaque with magnetic resonance direct thrombus imaging in patients with cerebral ischemia. Circulation 2003; 107: 3047–3052.
- 8.
Murphy RE, Moody AR, Morgan PS, Martel AL, Delay GS, Allder S, et al. Prevalence of complicated carotid atheroma as detected by magnetic resonance direct thrombus imaging in patients with suspected carotid artery stenosis and previous acute cerebral ischemia. Circulation 2003; 107: 3053–3058.