2015 年 79 巻 2 号 p. 419-424
2015 年 79 巻 2 号 p. 419-424
Background: The relationship between outcome of radiofrequency catheter ablation (RFCA) for atrial fibrillation (AF) and the severity of left ventricular (LV) diastolic dysfunction in patients with hypertrophic cardiomyopathy (HCM) remains unknown.
Methods and Results: Twenty-two HCM patients (12 female, aged 65±11 years) with paroxysmal (n=5; 23%) or persistent (n=17; 77%) AF were enrolled. LV diastolic function was evaluated according to the ratio of the mitral inflow early filling velocity to the velocity of the early medial mitral annular ascent (E/e’) measured on pulsed wave and tissue Doppler assessments in all patients. Pulmonary vein isolation was performed in all patients. A second procedure was performed in 3 patients. During a follow-up of 21±12 months, sinus rhythm was maintained in 13 of 22 patients (59%). E/e’ was significantly higher in the patients with AF recurrence than in those without (18±7 vs. 11±3; P<0.01). On Kaplan-Meier analysis the prevalence of AF recurrence was significantly higher in patients with E/e’ ≥15 (n=6) than in those with E/e’ <15 (n=16; P<0.01). On multivariate Cox regression analysis the only significant and independent predictor for AF recurrence was E/e’ (hazard ratio, 1.16; 95% confidence interval: 1.01–1.37, P=0.03).
Conclusions: LV diastolic dysfunction evaluated using E/e’ was associated with difficulty of rhythm control after RFCA in patients with HCM and AF. (Circ J 2015; 79: 419–424)
Atrial fibrillation (AF) is the most common tachyarrhythmia in patients with hypertrophic cardiomyopathy (HCM). AF is often poorly tolerated and is associated with significant clinical deterioration in these patients.1–3 Maintenance of sinus rhythm (SR) is desirable in patients with HCM. Several studies have shown that radiofrequency catheter ablation (RFCA) of severely symptomatic AF is both a feasible and safe approach in patients with HCM.4–7 The presence and severity of left ventricular (LV) diastolic dysfunction increase the risk of AF recurrence after RFCA in patients without structural heart disease.8 In patients with HCM, severe LV diastolic dysfunction is common due to the thickened and non-compliant ventricular chambers. The relationship between the outcome of RFCA for AF in patients with HCM and the severity of LV diastolic dysfunction, however, has not been fully investigated. The purpose of this study was to evaluate the impact of LV diastolic dysfunction, as measured on ultrasonography, on the outcome of RFCA for AF in patients with HCM.
Editorial p 305
Twenty-four consecutive Japanese patients with HCM undergoing RFCA of paroxysmal or persistent AF at the National Cerebral and Cardiovascular Center from 2009 to 2012 were reviewed. The diagnosis of HCM was based on the presence of myocardial hypertrophy in the absence of local or systemic etiology. Paroxysmal and persistent AF were defined according to the 2012 HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation.9 Two patients in whom LV diastolic dysfunction was not evaluated on ultrasonography were excluded. Consequently, 22 HCM patients were enrolled in this study. All patients provided informed consent. All patients were on oral anticoagulant therapy maintaining a target international normalized ratio of 2–3. Transesophageal echocardiography was performed to exclude any left atrial thrombi prior to the procedure in all patients.
EchocardiographyComprehensive 2-D and Doppler echocardiography were performed in each patient using commercially available instruments before RFCA.10,11 SR was maintained at the time of echocardiography in 15 of 22 patients. When echocardiography was performed during AF, all echocardiographic parameters were measured with an average of 3 consecutive beats. LV outflow tract (LVOT) gradient was measured with continuous-wave Doppler in the apical 3-chamber view. LVOT obstruction (LVOTO) was defined as a gradient >30 mmHg.12 LV diastolic function was evaluated as the ratio of the mitral inflow early filling velocity to the velocity of the early medial mitral annular ascent (E/e’), measured on pulsed wave and tissue Doppler.13
RFCAThe RFCA was performed under sedation with i.v. propofol. All anti-arrhythmia medication, except for amiodarone, was discontinued for at least 5 half-lives before the procedure in all patients. Two standard catheters were positioned: a 6-F catheter (St. Jude Medical, Minnetonka, MN, USA) at the His bundle region via a femoral vein, and another 6-F catheter (Japan Lifeline, Tokyo, Japan) in the coronary sinus via the right cervical vein. The transseptal procedure was performed using fluoroscopic landmarks, and 2 SL0 sheaths (St. Jude Medical) and an 8.0-F Preface sheath (Biosense Webster, Irwindale, CA, USA) were advanced into the left atrium (LA). After the transseptal procedure, a single bolus of 4,000 U heparin was given. A continuous infusion with heparinized saline was performed to maintain an activated clotting time of 300–350 s. Two 7-F decapolar circular catheters (Lasso, Biosense-Webster, Diamond Bar, CA, USA) and a 3.5-mm open irrigated tip ablation catheter (Navistar Thermocool, Biosense Webster) were inserted into the LA. We performed 3-D electroanatomical mapping (CARTO system, Biosense Webster) of the LA. Mapping was complete when all regions of the LA had been systematically sampled and when a sufficient density of points had been acquired to determine the LA chamber. After reconstruction of the LA, the volume of the LA chamber was automatically analyzed with the CARTO system. Each pulmonary vein (PV) ostium was identified on PV venography and tagged on the 3-D electroanatomical map. Two decapolar circular mapping catheters were placed inside the ipsilateral superior and inferior PV. The circumferential ablation lines, using a 3.5-mm tip irrigated catheter targeting a maximum temperature of 43℃, maximum power of 25–30 W, and infusion rate of 17 ml/min, were created at a distance from the PV ostia. The endpoint of the PV isolation was defined as the establishment of bidirectional conduction block between the LA and PV at least 30 min after successful PV isolation. Cavo-tricuspid isthmus ablation was performed at the operator’s discretion.
Post-Procedure Care and Follow-upAfter the first procedure, all patients received a follow-up every 1–3 months in the outpatient clinic. Follow-up included 12-lead electrocardiogram, 24-h Holter monitoring and assessment of the current condition. Anti-arrhythmic agents were resumed when there was evidence that AF recurred during the early unstable period after the procedure. AF recurrence was defined as sustained AF lasting >1 min. AF recurrence within a 2-month period after the procedure was considered transient, and a 2-month period was applied as a blanking period. Following the blanking period, repeat RFCA was carried out in the event of a recurrence of AF or atrial tachycardia. PV isolation was assessed and further ablation delivered as necessary.
Statistical AnalysisData were analyzed using JMP 9.0e (SAS Institute, Cary, NC, USA). Numeric data are expressed as the mean±SD. Chi-squared test or Student’s t-test was used when appropriate to test for statistical difference. P<0.05 was considered statistically significant. Receiver operating characteristic (ROC) curve analysis was used to identify the value of E/e’ predictive of AF recurrence. Event rate curves were plotted according to the Kaplan-Meier method and were analyzed with the log-rank test. Univariate Cox regression analysis was performed to identify predictors of subsequent AF recurrence. The hazard ratio (HR) and 95% confidence interval (95% CI) were defined. To confirm their independent predictive value, variables with P<0.05 were tested in a multivariate model.
Patient clinical characteristics are listed in Table 1. Persistent AF was found in 17 patients (77.3%). Longstanding persistent AF was not included in this study. The mean duration of AF was 80±53 months. The mean of the LA diameter was 48±6 mm and the mean LA volume measured on 3-D mapping was 98±38 ml.
| Variable | Total (n=22) |
AF recurrence (n=9) |
Without AF recurrence (n=13) |
P-value |
|---|---|---|---|---|
| Age (years) | 65±11 | 67±8 | 64±12 | 0.52 |
| Female | 12 (54.5) | 6 (66.7) | 6 (46.2) | 0.90 |
| Paroxysmal AF | 5 (22.7) | 2 (22.2) | 3 (23.1) | 0.96 |
| Persistent AF | 17 (77.3) | 7 (77.8) | 10 (76.9) | 0.96 |
| Duration of AF (months) | 80±53 | 107±56 | 62±45 | 0.052 |
| Family history of HCM | 4 (18.2) | 2 (22.2) | 2 (15.4) | 0.68 |
| Use of AAD | 15 (68.2) | 5 (55.6) | 10 (76.9) | 0.29 |
| Echocardiography | ||||
| Middle LV thickness (mm) | 13±4 | 12±4 | 14±5 | 0.28 |
| LVDd (mm) | 45±6 | 47±2 | 44±2 | 0.30 |
| LVDs (mm) | 30±7 | 32±2 | 28±2 | 0.26 |
| LVEF (%) | 57±14 | 54±13 | 59±14 | 0.48 |
| E | 65±18 | 60±14 | 68±20 | 0.31 |
| e’ | 5±2 | 4±1 | 7±2 | 0.0009 |
| E/e’ | 14±6 | 18±7 | 11±3 | 0.002 |
| MR (>moderate) | 5 (22.7) | 2 (22.2) | 3 (23.1) | 0.96 |
| LVOTO (>30 mmHg) | 3 (13.6) | 3 (33.3) | 0 (0.0) | 0.03 |
| LA diameter (mm) | 48±6 | 49±5 | 46±6 | 0.20 |
| LA volume (ml)† | 98±38 | 115±41 | 86±33 | 0.08 |
| RFCA | ||||
| Pulmonary vein isolation | 22 (100) | 9 (100) | 13 (100) | NS |
| CTIA | 10 (45.5) | 2 (22.2) | 8 (61.5) | 0.12 |
| Second procedure | 3 (13.6) | 1 (11.1) | 2 (15.4) | 0.22 |
| Follow-up period (months) | 21±12 | 22±14 | 20±11 | 0.72 |
Data given as mean±SD or n (%). †Measured on 3-D electrophysiologic mapping. AAD, anti-arrhythmic drug; AF, atrial fibrillation; CTIA, cavo-tricuspid isthmus ablation; E, mitral inflow early filling velocity; e’, velocity of early medial mitral annular ascent; HCM, hypertrophic cardiomyopathy; LA, left atrium; LV, left ventricle; LVDd, left ventricular dimension at end-diastole; LVDs, left ventricular dimension at end-systole; LVEF, left ventricular ejection fraction; LVOTO, left ventricular outflow tract obstruction; MR, mitral regurgitation; RFCA, radiofrequency catheter ablation.
All PV were successfully isolated in all patients. The mean procedure time was 244±60 min and the total duration of the RF applications was 39±12 min. Cavo-tricuspid isthmus ablation was performed in 10 patients (45.5%). No patients received linear lesions in the LA or a complex fractionated atrial electrogram ablation. In 3 patients, a second procedure was performed for recurrence of AF. Recovered PV conduction was found and successfully eliminated with RFCA.
Effect of RecurrenceFrom 21±12 months after the last procedure, maintenance of SR was observed in 13 of 22 patients (59%; Table 1). There were no significant differences between patients with and without AF recurrence with respect to age, gender, type of AF, family history of HCM, use of anti-arrhythmic drugs, or follow-up period (Table 1). The duration of AF tended to be longer in the patients with AF recurrence than in those without (P=0.052). There were also no significant differences on echocardiography between patients with and without AF recurrence except for E/e’, e’ and number of patients with LVOTO (>30 mmHg). Compared with the patients without AF recurrence, E/e’ and number of patients with LVOTO (>30 mmHg) were significantly higher in those with an AF recurrence (18±7 vs. 11±3; P=0.002 and 3 vs. 0; P=0.03, respectively). E’ was significantly lower in those with AF recurrence (3.6±1.2 vs. 6.5±2.0; P=0.0009).
There was no significant difference in the number of cavo-tricuspid isthmus ablations during the initial RFCA and the second procedure between the patients with and without AF recurrence. LA volume measured on 3-D electroanatomical mapping tended to be larger in the patients with AF recurrence than in those without (115±41 vs. 86±33; P=0.08).
LV Diastolic Dysfunction and Outcome of RFCAComparison of E/e’ between the patients with and without AF recurrence is shown in Figure 1. E/e’ was significantly higher in the patients with AF recurrence than in those without. In all 13 patients without AF recurrence, E/e’ was <15. In contrast, in 6 of 9 patents (67%) with AF recurrence, E/e’ was >15. On ROC curve analysis, the optimal threshold of E/e’ for predicting AF recurrence was 15 (sensitivity, 67%; specificity, 100%). The area under the ROC curve was 0.88. Figure 2 shows the results of Kaplan-Meier analysis of the maintenance of SR following RFCA. Patients with E/e’ ≥15 had a significantly higher risk of AF recurrence than those with E/e’ <15 (log-rank, P<0.001).
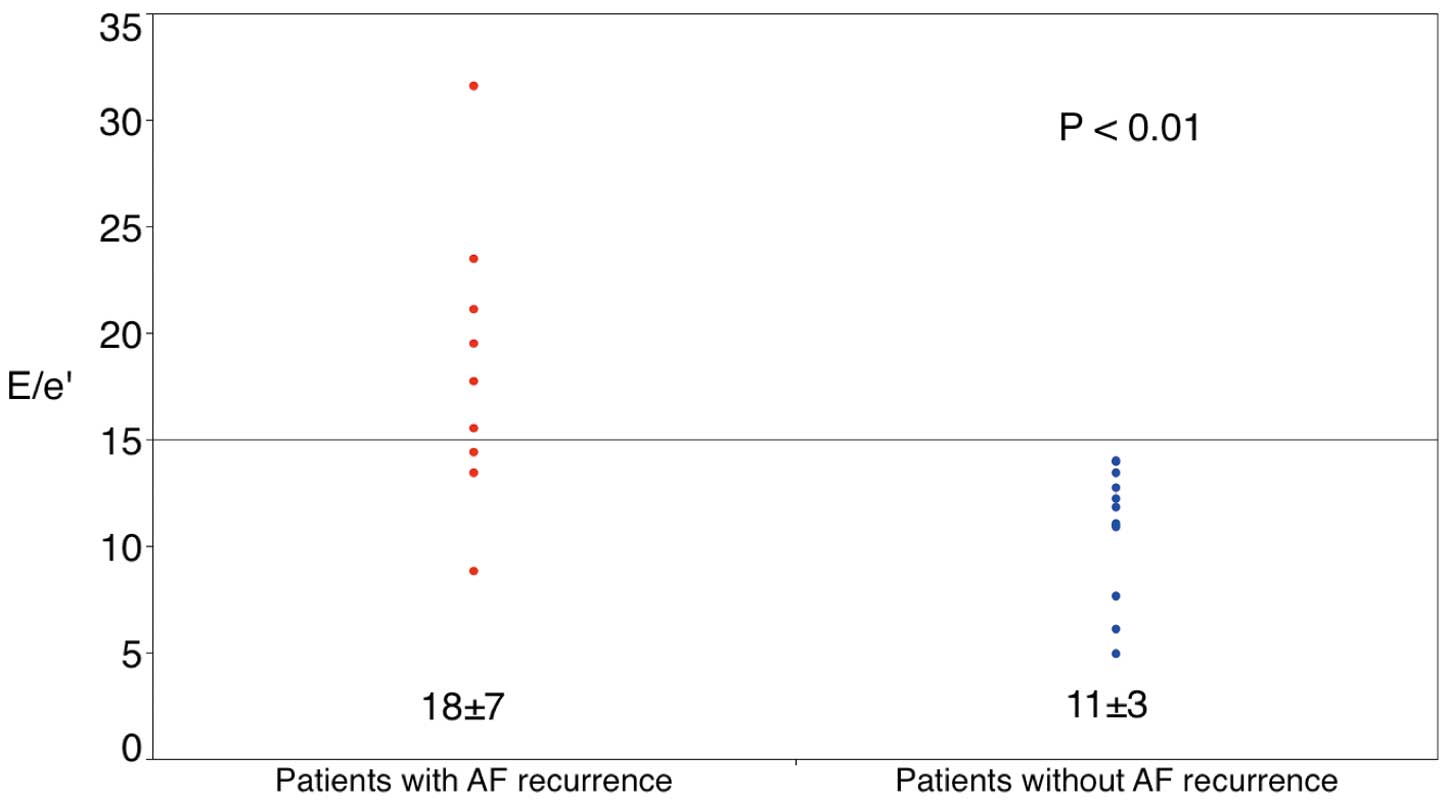
E/e’ vs. presence of atrial fibrillation (AF) recurrence. E/e’ was significantly higher in the patients with AF recurrence than in those without (P<0.01). E, mitral inflow early filling velocity; e’, velocity of early medial mitral annular ascent.
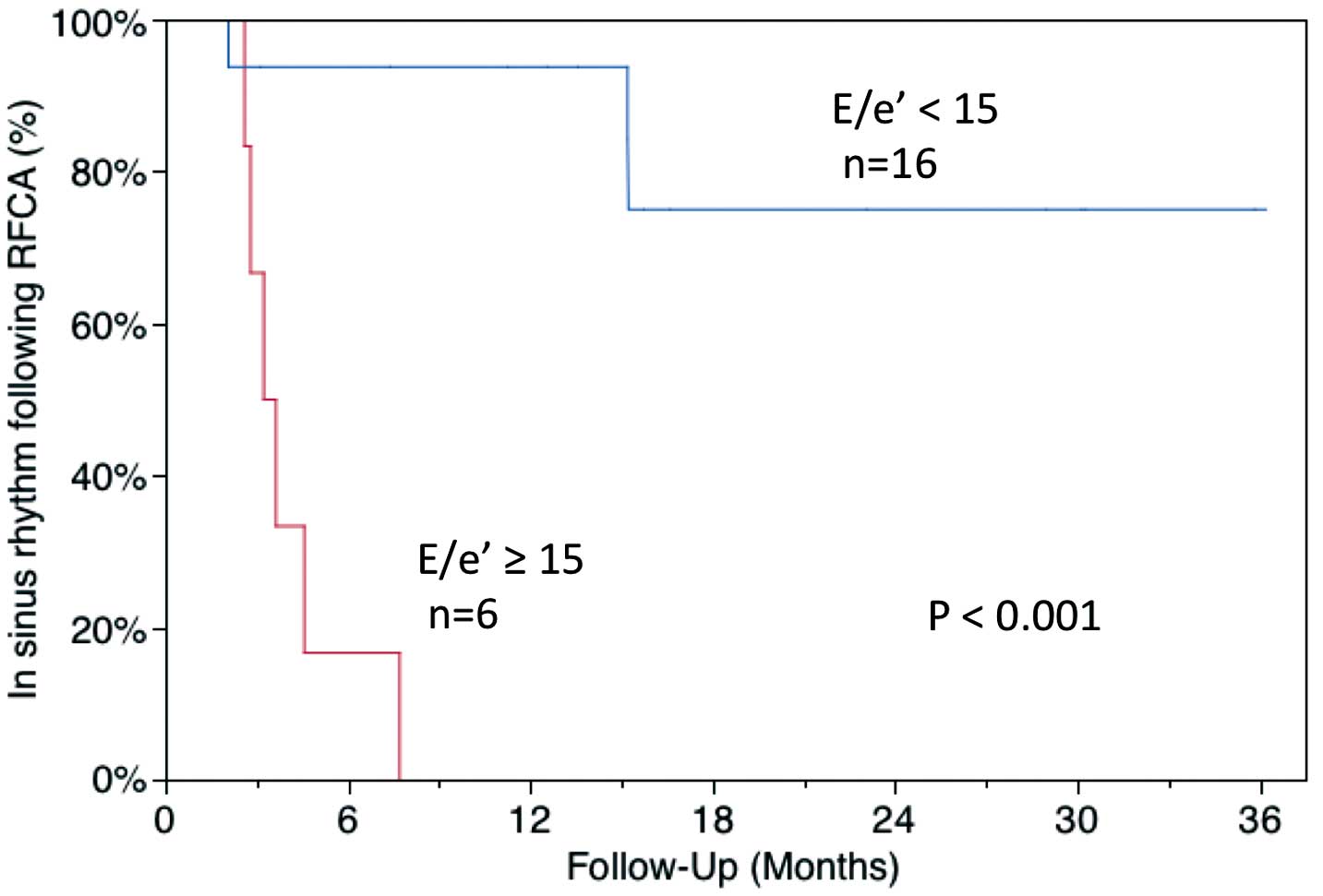
Kaplan-Meier curve of the maintenance of sinus rhythm following radiofrequency catheter ablation (RFCA). Patients with E/e’ ≥15 had a significantly higher risk of atrial fibrillation recurrence than those with E/e’ <15 (log-rank, P<0.001). E, mitral inflow early filling velocity; e’, velocity of early medial mitral annular ascent.
The results of Cox regression analysis are shown in Table 2. On univariate Cox regression analysis, E/e’, duration of AF and LA volume measured on 3-D electroanatomical mapping were significant predictors of AF recurrence. On multivariate Cox regression analysis E/e’ was the only predictor of AF recurrence following RFCA (HR, 1.16; 95% CI: 1.01–1.37, P=0.03).
| Univariate | Multivariate | |||
|---|---|---|---|---|
| HR (95% CI) | P-value | HR (95% CI) | P-value | |
| E/e’ | 1.19 (1.07–1.33) | 0.002 | 1.16 (1.01–1.37) | 0.03 |
| Duration of AF (months) | 1.02 (1.00–1.03) | 0.02 | 1.01 (0.99–1.03) | 0.40 |
| LA volume (ml)† | 1.02 (1.00–1.03) | 0.04 | 1.00 (0.98–1.02) | 0.28 |
| LA diameter (mm) | 1.14 (1.00–1.33) | 0.05 | ||
| LVOTO (>30 mmHg) | 3.99 (0.83–15.1) | 0.08 | ||
| CTIA | 0.50 (0.11–1.92) | 0.32 | ||
| Second procedure | 0.77 (0.04–4.28) | 0.80 | ||
†Measured on 3-D electrophysiologic mapping. Abbreviations as in Table 1.
The major findings of the present study are as follows: (1) E/e’ was significantly higher in patients with AF recurrence than in those without; (2) patients with E/e’ ≥15 had a significantly higher risk of AF recurrence than those with E/e’ <15; and (3) E/e’ was the only predictor of AF recurrence following RFCA in the patients with HCM. To the best of our knowledge, this is the first report to describe the relationship between LV diastolic dysfunction and outcome of RFCA for AF in patients with HCM.
LV Diastolic Dysfunction and AF RecurrenceIn the present study, we examined the correlation between LV diastolic dysfunction, estimated as E/e’, and outcome for AF in HCM patients. In patients with HCM, the mitral variables of E/A ratio and deceleration time of early filling velocity have weak to no correlations with LV filling pressures.14,15 But E/e’ correlated reasonably well with LV pre-A pressure during SR,15 which mean that E/e’ is a good parameter of LV diastolic function even in patients with HCM. E/e’ was significantly higher and e’ was significantly lower in patients with AF recurrence. The lower e’ reflects impaired myocardial relaxation. Severely impaired myocardial relaxation should elevate LA pressure, manifested as higher E/e’.16,17 Elevated LA pressure might result in continuous atrial remodeling after RFCA, which might explain why a higher recurrence was noted. Patients with LV diastolic dysfunction and AF have a lower LA voltage and higher recurrence rate of AF after RFCA.8,18,19 In contrast, SR was maintained in 13 of 16 patients (82%) with mild or moderate LV diastolic dysfunction (E/e’ <15). In those patients, the LA pressure might not be so high and the LA remodeling might not progress very much after RFCA for AF. The present results are in accordance with the previous reports showing that the presence and severity of LV diastolic dysfunction increased the risk of AF in patients with preserved LV systolic function.20–22
Several studies have demonstrated that RFCA of severely symptomatic AF is both a feasible and safe approach in patients with HCM.4–7 Di Donna et al found that the most important independent predictors of AF recurrence following RFCA consisted of age, functional status and LA volume.4 In that study, however, the relationship between the outcome of RFCA for AF and the severity of the LV diastolic dysfunction was not examined. Bunch et al showed that AF control following RFCA was less likely in patients with more advanced LV diastolic dysfunction.7 In the present study, LV diastolic dysfunction was graded as normal (grade 0), abnormal relaxation (grade I), pseudonormalization (grade II), restrictive (grade III), or irreversible advanced restrictive (grade IV). Although the grade of diastolic dysfunction was inversely related to the rate of AF control, this relationship did not reach statistical significance. Also, echocardiographic variables utilized to assess LV diastolic function were not associated with a reduced likelihood of AF control. The severity of LV diastolic dysfunction was not assessed in some patients due to AF during echocardiography, which might result in exclusion of the patients with severe LV diastolic dysfunction and weakening of the inverse relationship between the severity of LV diastolic dysfunction and the rate of AF control.
Clinical ImplicationAccording to the ESC guidelines for the management of AF, RFCA for symptomatic AF refractory to pharmacological control in patients with HCM is a class IIa indication.23 At the same time, the ESC guidelines note that severe LV diastolic dysfunction is at high risk for recurrence. The appropriate candidates for RFCA in patients with HCM and AF have not been defined. We showed that outcome after RFCA was favorable in patients with mild or moderate LV diastolic dysfunction (E/e’ <15). This suggests that HCM patients with mild or moderate LV diastolic dysfunction (E/e’ <15) and AF might be good candidates for RFCA.
Study LimitationsThis study had several limitations. First, this study was a retrospective study. Second, we could have underestimated the recurrence rate after RFCA for AF because asymptomatic AF recurrence could have been missed. Third, echocardiography was performed during AF in 7 of 22 patients. Although echocardiography during AF can be inaccurate, E/e’ is useful in the estimation of LV filling pressure even in patients with AF.24,25 There were no changes in LV diastolic parameters on tissue Doppler imaging following electrical cardioversion in patients with persistent AF,26 which means that these parameters were used equally in the patients with SR and AF. Fourth, this was an analysis of a small number of patients and a small number of events. Further examination is required with a larger number of patients to confirm the present results.
LV diastolic dysfunction evaluated on E/e’ was linked to the possibility of rhythm control after RFCA in the patients with HCM and AF. Patients with mild or moderate LV diastolic dysfunction (E/e’ <15) might be good candidates for RFCA in those with HCM and AF.
We thank Mr John Martin for the linguistic revision.
Funding: Nothing to disclose.