Abstract
Background:
The association of morning and evening home blood pressures (HBPs) with carotid atherosclerosis has been uncertain in general populations, so we aimed to investigate it in a general Japanese population.
Methods and Results:
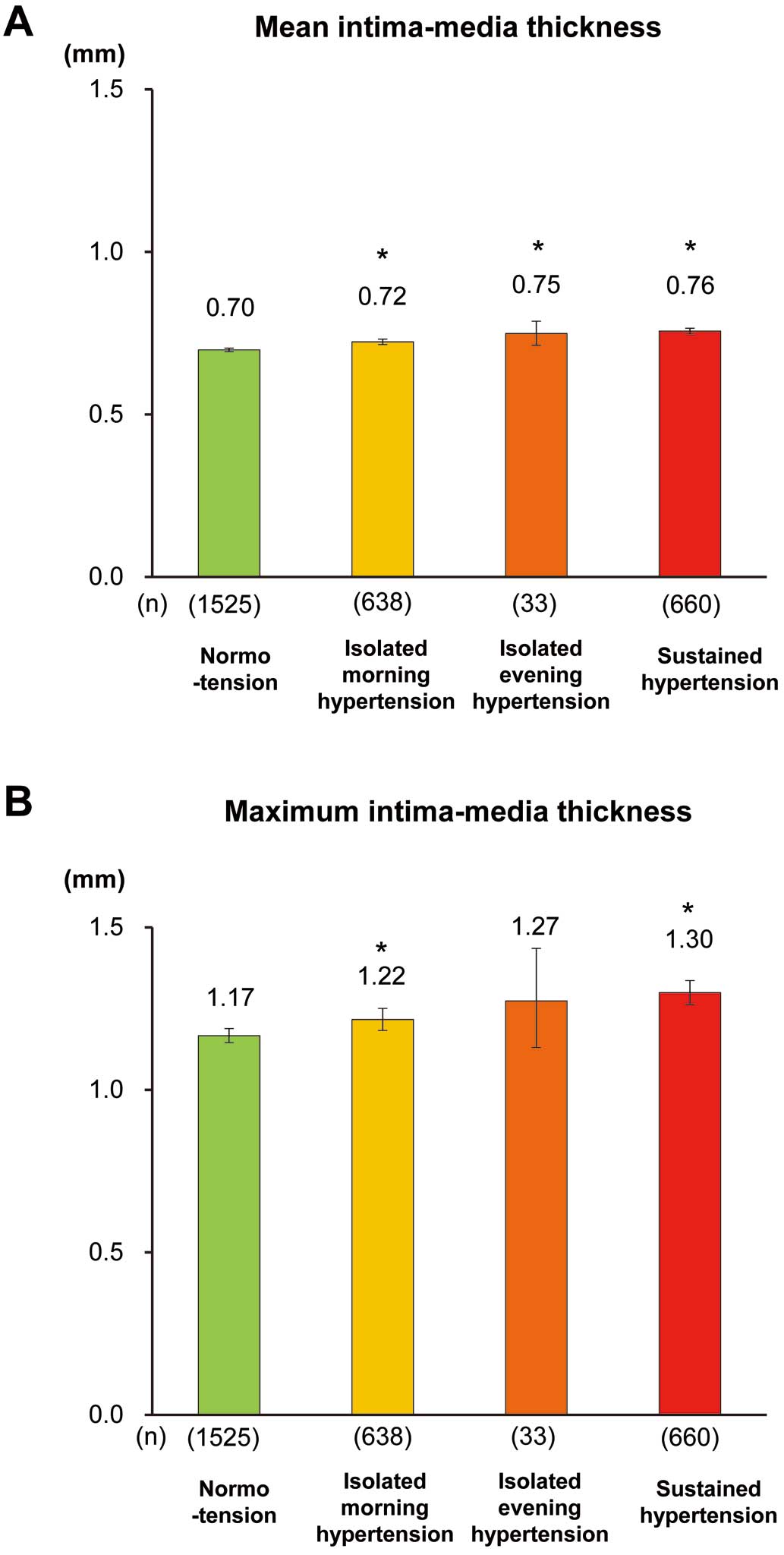
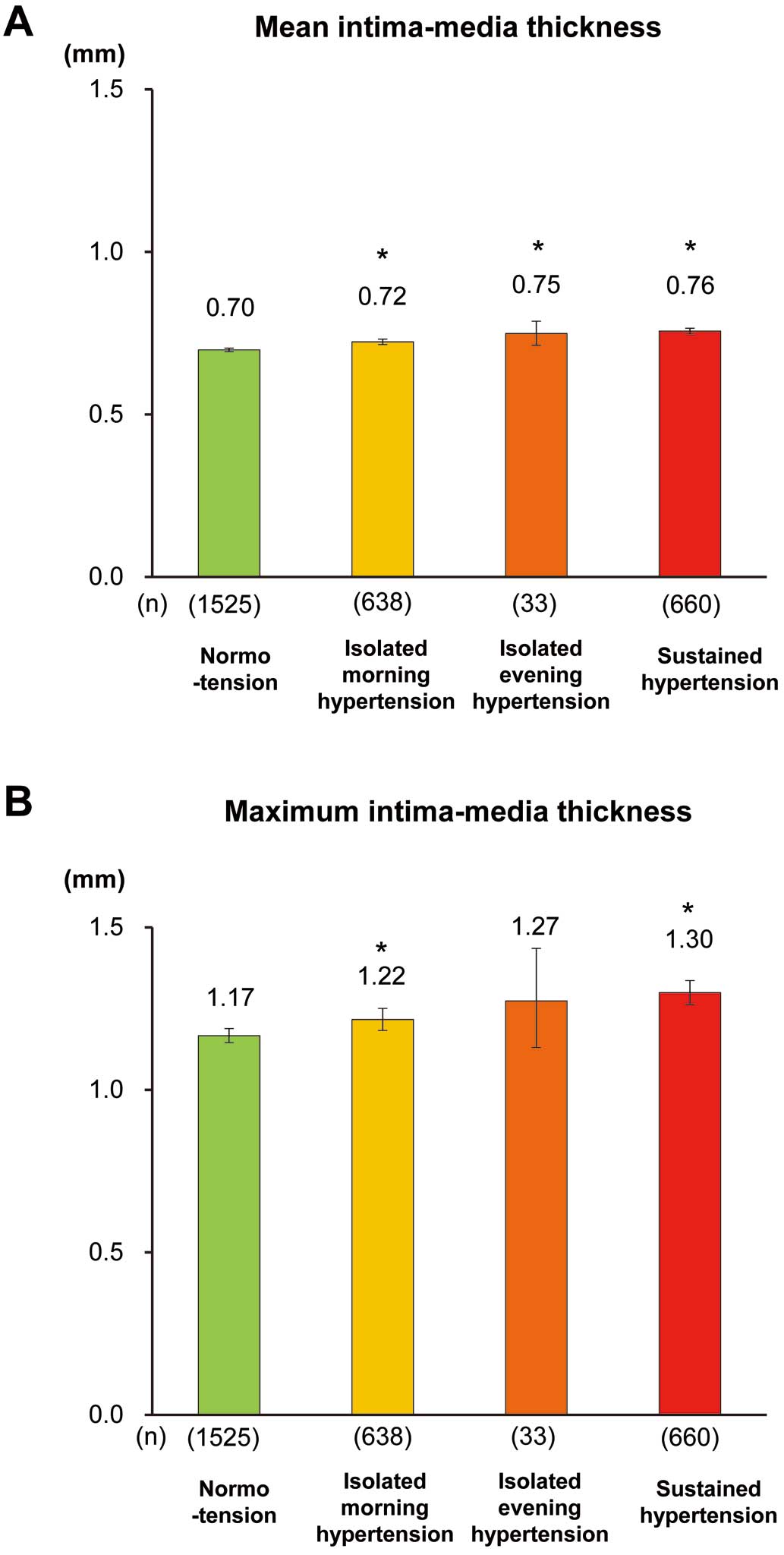
We performed a cross-sectional survey of 2,856 community-dwelling individuals aged ≥40 years to examine the association of morning and evening HBPs with carotid mean intima-media thickness (IMT). The age- and sex-adjusted geometric averages of carotid mean IMT increased significantly with increasing morning HBP (optimal: 0.67 mm; normal: 0.69 mm; high normal: 0.72 mm; grade 1 hypertension: 0.74 mm; and grade 2+3 hypertension: 0.76 mm) and with increasing evening HBP (0.68 mm, 0.71 mm, 0.73 mm, 0.76 mm, and 0.78 mm, respectively) (both P for trend <0.001). These associations remained significant even after adjusting for potential confounding factors. Likewise, both isolated morning hypertension (morning HBP ≥135/85 mmHg and evening HBP <135/85 mmHg) and isolated evening hypertension (evening HBP ≥135/85 mmHg and morning HBP <135/85 mmHg) as well as sustained hypertension (both morning and evening HBP ≥135/85 mmHg) were significantly associated with thicker mean IMT.
Conclusions:
Our findings suggested that both morning and evening HBPs were significantly associated with carotid atherosclerosis in this general Japanese population.
Measuring home blood pressure (HBP) is becoming common for hypertensive patients in clinical practice. HBP measurement can reduce observer biases and white-coat effects, and is useful to assess the duration of the effectiveness of antihypertensive medication and to improve adherence to antihypertensive treatment.1–5
In addition, HBP has been reported to be more sensitive for risk assessment of target organ damage than casual blood pressure (BP) measured at the clinic or health examination.6–9
BP has a circadian rhythm caused by neuroendocrine factors.10,11
Circadian rhythm is also affected by antihypertensive medication, and lifestyle factors.12–14
Therefore, it is important to measure HBP on different occasions. Several recent guidelines or scientific statements for hypertension management have recommended measuring HBP at least twice daily, namely, in the morning and in the evening.3–5,15
Most clinical studies have evaluated the association of HBP with target organ damage using average values of either morning and evening HBPs16–18
or only morning HBP.19,20
Meanwhile, there are limited numbers of studies addressing the influence of morning HBP and evening HBP separately on atherosclerotic disease in general populations, as the clinical significance of morning HBP and evening HBP may be different.
The purpose of the present study was to investigate the association of HBP levels in the morning and evening with carotid atherosclerosis in a general Japanese population.
Methods
Study Population
The Hisayama Study is a population-based observational study for cardiovascular disease, which was established in 1961 in the town of Hisayama, a suburb of the Fukuoka metropolitan area on Kyushu Island, Japan.21–23
In 2007 and 2008, a total of 3,384 residents of Hisayama aged 40 years or older participated in health examinations (participation rate among the total population of this age group: 78.2%). After the exclusion of 8 participants who refused to participate in the epidemiological study, 453 subjects without HBP measurements for more than 3 days, and 67 without information on carotid ultrasonography, a total of 2,856 subjects (1,234 men and 1,622 women) were enrolled in the present study.
Home and Clinical BP Measurements
The procedure for the measurement of HBP was described in detail in our previous report24
and followed the Japanese guidelines for self-monitoring of BP at home.3
HBP was measured using an automatic device (HEM-7080IC; Omron Healthcare Co., Ltd.) based on the validated cuff oscillometric method. This device uses the identical components and BP-determining algorithm as another device, HEM-705IT, which was previously validated and satisfied the criteria of the British Hypertension Society protocol.25
The subjects were instructed to measure their HBP 3 times every morning before breakfast within 1 h of waking and 3 times every evening before going to bed after more than 5 min of rest while seated, for 4 weeks. Subjects on antihypertensive medication were instructed to measure their HBP before taking their medication. Morning and evening HBPs were defined as the mean value of daily averages of HBP in the morning and in the evening, respectively. In addition, clinical BP was measured 3 times at the health examination using an automated sphygmomanometer (BP-203 RVIIIB; Omron Healthcare Co., Ltd.), and the mean of 3 measurements was used for the analysis.
Classification of Groups Based on HBP
HBP was categorized by the measured values, regardless antihypertensive medication. In the present analysis, we defined HBP from the European Society of Hypertension and European Society of Cardiology (ESH-ESC) criteria4
minus 5 mmHg, because HBP of 135/85 mmHg is considered to be equivalent to clinical BP of 140/90 mmHg. For each morning and evening HBP, values were classified into 5 categories as follows: optimal (HBP <115/75 mmHg); normal (HBP 115–124/75–79 mmHg); high normal (HBP 125–134/80–84 mmHg); grade 1 hypertension (HBP 135–154/85–94 mmHg); grade 2+3 hypertension (HBP ≥155/95 mmHg). The subjects were also divided into 4 groups according to the combination of morning and evening HBP: normotension (morning HBP <135/85 mmHg and evening HBP <135/85 mmHg), isolated morning hypertension (morning HBP ≥135/85 mmHg and evening HBP <135/85 mmHg), isolated evening hypertension (morning HBP <135/85 mmHg and evening HBP ≥135/85 mmHg), and sustained hypertension (morning HBP ≥135/85 mmHg and evening HBP ≥135/85 mmHg). Furthermore, for the sensitivity analysis, the subjects were re-categorized into 4 groups using a different cutoff value of 126/76 mmHg for evening HBP, which corresponded to morning HBP of 135/85 mmHg in a linear regression analysis between morning and evening HBP (Figure S1), in order to correct for the imbalance in the number of subjects with isolated evening hypertension.
Carotid Ultrasonography
Carotid ultrasonography was performed using a real-time, B-mode ultrasound imaging unit (Toshiba Sonolayer SSA-250A; Toshiba, Tokyo, Japan) with a 7.5-MHz annular array probe as described previously.24
Mean intima-media thickness (IMT) was measured using the long-axis views of the right and left common carotid arteries. We examined the far wall of each common carotid artery in the region that was 20 mm proximal to the origin of the bulb, and automatically calculated the average IMT as the mean value of IMT measurements on each side using a computer-assisted measurement system (Intimascope; Media Cross Co., Ltd, Tokyo, Japan).26
Mean IMT was defined as the mean of the average IMT of the left and right sides. Maximum IMT in the observation-possible areas of the left and right common carotid arteries, bulbs, and internal carotid arteries was measured manually. Carotid wall thickening was defined as a maximum IMT >1.0 mm. Moreover, advanced carotid wall thickening was determined as a maximum IMT >1.5 mm.
Other Risk Factors
At the health examination, each participant completed a self-administered questionnaire covering medical history, antihypertensive medication, lipid-lowering medication, smoking habit, alcohol intake, and regular exercise. Smoking habit and alcohol intake were classified as either current use or not. Subjects engaging in sports or other forms of exertion ≥3 times a week during their leisure time made up the regular exercise group. Body height and weight were measured in light clothing without shoes, and the body mass index (BMI: kg/m2) was calculated. Serum total and high-density lipoprotein (HDL) cholesterol levels were determined enzymatically. Blood glucose levels were measured by the hexokinase method. Diabetes mellitus was determined as fasting glucose level ≥7.0 mmol/L, postprandial or 2-h postload glucose level ≥11.1 mmol/L, or use of antidiabetic medication.
Statistical Analysis
The correlation between morning or evening HBP and clinical BP was evaluated using Pearson’s correlation coefficient. The differences in the mean values of continuous variables or frequencies of categorical variables across the morning or evening HBP categories were examined using an analysis of variance or a logistic regression model. Mean and maximum IMT were transformed into logarithm to improve skewness, and geometrical means were reported by back transformation. The adjusted geometric averages of the mean and maximum IMT across the morning or evening HBP categories were assessed using an analysis of covariance. The age- and sex-adjusted prevalence of carotid wall thickening was calculated using the direct method, using the distributions of age and sex in the study population as a reference population. The age- and sex-adjusted or multivariable-adjusted odds ratio and its 95% confidence interval (CI) for the presence of carotid wall thickening were estimated using a multivariable logistic regression model. The subgroup analyses by antihypertensive medication status and by drinking status were conducted, and the heterogeneity in the effects of BP levels on outcomes between the subgroups was estimated by adding interaction terms to the relevant statistical model. The heterogeneity in the association with carotid atherosclerosis between morning and evening HBPs was tested by adding an interaction term in the relevant statistical model with generalized estimating equations in order to account for repeated measurements of morning and evening HBP for each individual. All statistical analyses were performed using the SAS program package version 9.3 (SAS Institute Inc., Cary, NC, USA). P values <0.05 were considered statistically significant.
Ethical Considerations
The study protocol was approved by Kyushu University Institutional Review Board for Clinical Research, and the procedures followed were in accordance with national guidelines. Written informed consent was given by all the subjects.
Results
For the total subjects, the mean value±standard deviation of morning HBP, evening HBP, and clinical BP at the health examination was 132±18/77±10 mmHg, 124±16/70±9 mmHg, and 131±19/79±11 mmHg, respectively. The mean values of morning HBP were significantly higher than those of evening HBP (both P<0.001). Both morning and evening HBPs were significantly correlated with clinical BP (Pearson’s correlation coefficient: 0.64 between morning systolic HBP and clinical systolic BP; 0.62 for evening systolic HBP and clinical systolic BP; both P<0.001).
The clinical characteristics of the subjects according to the levels of morning HBP and evening HBP are summarized in
Table 1
and
Table S1, respectively. Subjects with higher morning HBP levels were older and more likely to be male. The mean values of BMI increased significantly with increasing morning HBP levels, whereas the mean values of HDL-cholesterol decreased significantly. The frequencies of subjects with antihypertensive medication, diabetes, lipid-lowering medication, current drinking, and regular exercise increased significantly with increasing morning HBP levels. Similar associations were observed for evening HBP levels except for current smoking and regular exercise: subjects with higher evening HBP levels were more likely to be smokers and had no significant association with the frequency of regular exercise.
Table 1.
Clinical Characteristics of Participants According to Morning HBP Levels
| |
Morning HBP level |
P for
trend |
Optimal
(n=513) |
Normal
(n=458) |
High normal
(n=587) |
Grade 1
hypertension
(n=891) |
Grade 2+3
hypertension
(n=407) |
| Age, years |
55±10 |
61±11 |
63±11 |
66±11 |
69±12 |
<0.001 |
| Men, % |
25.0 |
39.5 |
45.8 |
49.8 |
52.1 |
<0.001 |
| Morning home systolic BP, mmHg |
107±6 |
119±3 |
129±4 |
142±7 |
162±11 |
<0.001 |
| Morning home diastolic BP, mmHg |
66±5 |
72±5 |
77±6 |
82±7 |
89±11 |
<0.001 |
| Evening home systolic BP, mmHg |
105±7 |
115±8 |
123±8 |
131±11 |
147±15 |
<0.001 |
| Evening home diastolic BP, mmHg |
62±6 |
67±6 |
70±7 |
73±8 |
78±11 |
<0.001 |
| Antihypertensive medication, % |
4.1 |
12.7 |
29.5 |
45.1 |
57.3 |
<0.001 |
| Diabetes mellitus, % |
4.5 |
12.0 |
16.9 |
22.6 |
25.3 |
<0.001 |
| Total cholesterol, mmol/L |
5.4±0.9 |
5.5±1.0 |
5.5±0.9 |
5.4±0.9 |
5.4±0.9 |
0.34 |
| HDL-cholesterol, mmol/L |
1.9±0.5 |
1.8±0.4 |
1.7±0.4 |
1.7±0.4 |
1.7±0.5 |
<0.001 |
| Lipid-lowering medication, % |
7.6 |
9.8 |
17.4 |
20.9 |
18.9 |
<0.001 |
| Body mass index, kg/m2 |
21.3±2.7 |
22.5±3.2 |
23.3±3.4 |
23.8±3.5 |
24.1±3.6 |
<0.001 |
| Current smoking, % |
18.5 |
16.6 |
18.6 |
18.9 |
22.6 |
0.11 |
| Current drinking, % |
44.1 |
46.3 |
48.4 |
51.2 |
54.1 |
<0.001 |
| Regular exercise, % |
9.2 |
13.3 |
11.6 |
14.9 |
12.0 |
0.04 |
All values are given as the mean±SD or as a percentage. HBP, home blood pressure; HDL, high-density lipoprotein.
Table 2
demonstrates geometric averages of mean and maximum IMT according to the levels of morning or evening HBP. The age- and sex-adjusted geometric average of mean IMT increased significantly and progressively with increasing morning HBP levels (optimal: 0.67 mm; normal: 0.69 mm; high normal: 0.72 mm; grade 1 hypertension: 0.74 mm; grade 2+3 hypertension: 0.76 mm; P<0.001 for trend) or evening HBP levels (optimal: 0.68 mm; normal: 0.71 mm; high normal: 0.73 mm; grade 1 hypertension: 0.76 mm; grade 2+3 hypertension: 0.78 mm; P<0.001 for trend). These associations were substantially unchanged even after adjustment for other cardiovascular risk factors, namely, antihypertensive medication, diabetes, total and HDL cholesterols, lipid-lowering medication, BMI, current smoking, current drinking, and regular exercise. When we examined the association of each morning and evening HBP with the geometric average of maximum IMT, a significant linear relation was observed between morning or evening HBP and maximum IMT. The associations of evening HBP with mean and maximum IMT were stronger than those of morning HBP (both P for heterogeneity <0.05).
Table 2.
Geometric Averages of Mean and Maximum IMT According to Morning or Evening HBP Levels
| |
HBP level |
P for
trend |
P for
heterogeneity‡ |
| Optimal |
Normal |
High normal |
Grade 1
hypertension |
Grade 2+3
hypertension |
| Mean IMT |
| Morning HBP |
| No. of participants |
518 |
458 |
587 |
891 |
407 |
|
|
Age- and sex-adjusted
geometric average (95% CI) |
0.67
(0.66–0.68) |
0.69
(0.69–0.70)* |
0.72
(0.71–0.73)* |
0.74
(0.73–0.74)* |
0.76
(0.75–0.77)* |
<0.001 |
|
Multivariable-adjusted
geometric average (95% CI)† |
0.68
(0.67–0.69) |
0.70
(0.69–0.71)* |
0.72
(0.71–0.73)* |
0.74
(0.73–0.74)* |
0.76
(0.75–0.77)* |
<0.001 |
0.005 |
| Evening HBP |
| No. of participants |
845 |
725 |
593 |
565 |
128 |
|
|
Age- and sex-adjusted
geometric average (95% CI) |
0.68
(0.67–0.69) |
0.71
(0.70–0.72)* |
0.73
(0.72–0.74)* |
0.76
(0.75–0.77)* |
0.78
(0.76–0.80)* |
<0.001 |
|
Multivariable-adjusted
geometric average (95% CI)† |
0.69
(0.68–0.69) |
0.71
(0.70–0.72)* |
0.73
(0.72–0.74)* |
0.75
(0.74–0.76)* |
0.78
(0.76–0.80)* |
<0.001 |
|
| Maximum IMT |
| Morning HBP |
| No. of participants |
518 |
458 |
587 |
891 |
407 |
|
|
Age- and sex-adjusted
geometric average (95% CI) |
1.14
(1.11–1.18) |
1.13
(1.09–1.16) |
1.20
(1.17–1.24)* |
1.25
(1.22–1.28)* |
1.31
(1.26–1.35)* |
<0.001 |
|
Multivariable-adjusted
geometric average (95% CI)† |
1.15
(1.11–1.19) |
1.14
(1.10–1.18) |
1.20
(1.17–1.23) |
1.25
(1.22–1.28)* |
1.29
(1.25–1.34)* |
<0.001 |
0.04 |
| Evening HBP |
| No. of participants |
845 |
725 |
593 |
565 |
128 |
|
|
Age- and sex-adjusted
geometric average (95% CI) |
1.14
(1.11–1.17) |
1.18
(1.15–1.21)* |
1.22
(1.18–1.25)* |
1.30
(1.26–1.34)* |
1.40
(1.32–1.49)* |
<0.001 |
|
Multivariable-adjusted
geometric average (95% CI)† |
1.15
(1.12–1.18) |
1.19
(1.16–1.22) |
1.22
(1.19–1.26)* |
1.28
(1.25–1.32)* |
1.38
(1.30–1.47)* |
<0.001 |
|
*P<0.05 vs optimal level. †Adjusted for age, sex, antihypertensive medication, diabetes, total cholesterol, HDL cholesterol, lipid-lowering medication, body mass index, current smoking, current drinking, and regular exercise. ‡Heterogeneity for multivariable-adjusted geometric averages. CI, confidence interval; IMT, intima-media thickness. Other abbreviations as in Table 1.
We also estimated the prevalence and odds ratios for carotid wall thickening (defined as maximum IMT >1.0 mm) according to each HBP level (Table 3). The age- and sex-adjusted prevalence of carotid wall thickening was significantly increased in subjects with higher HBP levels compared with those with optimal HBP levels in the morning. The multivariable-adjusted odds ratios (95% CIs) for carotid wall thickening were 0.92 (0.69–1.23) for normal, 1.33 (1.00–1.76) for high normal, 1.46 (1.11–1.92) for grade 1 hypertension, and 1.67 (1.19–2.35) for grade 2+3 hypertension, compared with the optimal level as a reference (P for trend <0.001). A significant association was also observed for evening HBP levels (multivariable-adjusted odds ratio [95% CI]: 1.37 [1.09–1.72], 1.46 [1.13–1.87], 1.79 [1.37–2.35], and 3.14 [1.92–5.33], respectively; P<0.001 for trend), indicating that both morning and evening HBP levels were significantly associated with carotid wall thickening independent of other cardiovascular risk factors. Evening HBP was more strongly associated with carotid wall thickening than was morning HBP (P for heterogeneity=0.02). Increased morning and evening HBP levels were also significantly associated with advanced carotid wall thickening defined as maximum IMT >1.5 mm (both P for trend <0.001), but no evidence of heterogeneity between morning and evening HBPs was observed (P for heterogeneity=0.55) (Table S2).
Table 3.
Odds Ratios for Carotid Wall Thickening According to Morning or Evening HBP Level
| |
HBP level |
P for
trend |
P for
heterogeneity‡ |
| Optimal |
Normal |
High normal |
Grade 1
hypertension |
Grade 2+3
hypertension |
| Morning HBP |
| No. of cases/participants |
86/513 |
149/458 |
264/587 |
489/891 |
270/407 |
|
|
Age- and sex-adjusted
prevalence, % |
46.4 |
49.1 |
58.2* |
60.0* |
65.2* |
<0.001 |
|
Age- and sex-adjusted
OR (95% CI) |
1 (Ref.) |
0.95
(0.72–1.26) |
1.45
(1.10–1.89) |
1.62
(1.25–2.09) |
1.88
(1.37–2.59) |
<0.001 |
|
Multivariable-adjusted
OR (95% CI)† |
1 (Ref.) |
0.92
(0.69–1.23) |
1.33
(1.00–1.76) |
1.46
(1.11–1.92) |
1.67
(1.19–2.35) |
<0.001 |
0.02 |
| Evening HBP |
| No. of cases/participants |
220/845 |
289/725 |
302/593 |
354/565 |
93/128 |
|
|
Age- and sex-adjusted
prevalence, % |
47.5 |
57.0* |
57.7* |
63.4* |
79.8* |
<0.001 |
|
Age- and sex-adjusted
OR (95% CI) |
1 (Ref.) |
1.44
(1.15–1.79) |
1.58
(1.24–2.00) |
2.05
(1.60–2.62) |
3.47
(2.11–5.69) |
<0.001 |
|
Multivariable-adjusted
OR (95% CI)† |
1 (Ref.) |
1.37
(1.09–1.72) |
1.46
(1.13–1.87) |
1.79
(1.37–2.35) |
3.14
(1.92–5.33) |
<0.001 |
|
Carotid wall thickening was defined as maximum IMT >1.0 mm. *P<0.05 vs. optimal level. †Adjusted for age, sex, antihypertensive medication, diabetes, total cholesterol, HDL cholesterol, lipid-lowering medication, body mass index, current smoking, current drinking, and regular exercise. ‡Heterogeneity for multivariable-adjusted ORs. OR, odds ratio. Other abbreviations as in Tables 1,2.
We conducted subgroup analyses stratified by the status of antihypertensive medication (Tables S3,S4). The multivariable-adjusted geometric averages of the mean and maximum IMT were higher in subjects with antihypertensive medication than in those without, but increased significantly and linearly with increasing morning or evening HBP levels both in the subgroups of subjects with and without antihypertensive medication (all P for heterogeneity >0.10). We also performed subgroup analyses stratified by drinking status (Tables S5,S6). Regardless of drinking status, there were significant associations of morning and evening HBP levels with the geometric averages of mean and maximum IMT, without any evidence of heterogeneity between subgroups (all P for heterogeneity >0.05).
Next, we examined geometric averages of mean and maximum IMT according to 4 BP groups: normotension, isolated morning hypertension, isolated evening hypertension, and sustained hypertension (Figure;
Table S7). The multivariable-adjusted geometric average of the mean IMT increased significantly in subjects with isolated morning hypertension, isolated evening hypertension, and sustained hypertension compared with normotensive subjects. For maximum IMT, similar associations were observed; however, there was no significant increase in isolated evening hypertension, probably because of the relative small number of subjects with isolated evening hypertension. In the subgroup analyses stratified by antihypertensive medication status, there was no evidence of heterogeneity in the association of the 4 BP groups with the mean and maximum IMT between the groups of antihypertensive medication status (both P for heterogeneity >0.4), although some P values in the groups of isolated morning hypertension and isolated evening hypertension did not reach the level of statistical significance (Table S8). When we combined the subjects with isolated morning hypertension and isolated evening hypertension, subjects with either isolated morning or evening hypertension had a significantly higher mean and maximum IMT than those with normotension (Table S9).
In addition, we performed a sensitivity analysis after changing the cutoff value of evening HBP from 135/75 to 126/76 mmHg to correct for the imbalance in the number of subjects with isolated evening hypertension. As a consequence, the average mean IMT and maximum IMT in subjects with isolated evening hypertension became lower, but the findings were not altered substantially (Table S10). There was also no significant heterogeneity in the association between antihypertensive medication status after changing the cutoff value for evening HBP (both P for heterogeneity >0.05) (Table S11)
Discussion
The present study demonstrated that increased morning and evening HBP was significantly associated with the presence of carotid atherosclerosis in a general Japanese population. It is noteworthy that these associations were unchanged by the use of antihypertensive medication or drinking status. The findings from this study are expected to show the importance of BP control in both the morning and the evening.
A few epidemiological studies in Japan19,24
and Finland16
have provided consistent findings that higher HBP is significantly associated with greater IMT despite differences in study populations. This suggests that mean HBP is closely related to carotid atherosclerosis. However, there are limited studies addressing the association of morning and evening HBP separately with clinical or subclinical cardiovascular disease, especially in general populations. The J-HOP Study,27
which evaluated outpatients with at least 1 cardiovascular risk factor, showed that higher morning and evening HBP levels were significantly linked with greater IMT, but the significant association remained only for morning HBP after adjusting for confounding factors. In the present study, evening HBP as well as morning HBP was clearly associated with carotid wall thickening. The discrepancy in the findings between the studies may be attributable to the difference in study populations. Patients with cardiovascular risk factors are more likely to have increased variability in evening BP, which tends towards a non-significant association, caused by insufficient duration of the action of antihypertensive medications28
and impairment of baroreflex or autonomic dysfunction29–31
than general populations. With regard to clinical cardiovascular events, 2 population-based prospective cohort studies32,33
have shown that both morning HBP and evening HBP have significant and equal predictive abilities for future stroke or cardiovascular events. All this evidence indicates the importance of assessing both morning and evening BP to prevent future risks of cardiovascular disease.
The present study demonstrated that morning hypertension, which was hypertension observed in the morning only, was significantly linked with greater IMT in this general population. Several studies conducted in hypertensive patients have reported that morning hypertension has a strong association with target organ damage8,9,34
and cardiovascular events.35,36
However, there are few previous studies that have examined this issue in general populations.32
Morning hypertension is considered to reflect inadequate BP control during night (e.g., via insufficient duration of action of antihypertensive drugs) and increased activities of neurohumoral factors, such as the sympathetic nervous system and the renin-angiotensin system in the morning, which promotes progression of arterial damage.10,11,28
Therefore, controlling morning BP is important for the prevention of atherosclerotic disease.
Evening BP has greater variability, affected more by antihypertensive mediations, daily customs (e.g., bathing and evening drink) and activities than morning BP.12
Therefore, morning BP may be considered as a more useful indicator of target organ disease than evening BP in clinical practice. In the current analysis, however, evening hypertension, defined as hypertension in the evening only, was clearly associated with mean IMT, just as with morning hypertension. No prior population-based investigation has evaluated this issue for carotid atherosclerosis to date. A prospective study of a general Japanese population32
supportively demonstrated that subjects with evening hypertension tended towards having a higher risk of stroke compared with normotensive subjects, though this association was not statistically significant. This finding, together with ours, suggests that higher evening BP itself contributes to the atherosclerotic process. Moreover, in the present study, evening HBP showed a significantly greater association with carotid atherosclerosis than morning HBP, a finding that was probably attributable to the fact that the morning and evening HBP levels were higher in each of the high normal and hypertension categories determined on evening HBP than in the corresponding categories defined on morning HBP (Table 1,S1). This may suggest that evening HBP is a better predictor of atherosclerosis than morning HBP, but the clinical significance of evening hypertension remains to be investigated.
Study Limitations
First, we were not able to determine a causal association of morning and evening HBP with IMT because of the cross-sectional study design. Second, several laboratory technicians measured maximum IMT manually, therefore there is the possibility that the association between HBP and maximum IMT observed in the present study was weaker than the true association. However, this limitation is unlikely to alter the conclusions of the present analysis, because similar results were obtained for mean IMT, which was estimated automatically using a computer-assisted measurement system. Finally, we could not exclude the possibility that residual confoundings still exist in the association.
Conclusions
To the best of our knowledge, this is the first report to demonstrate the association of both morning and evening HBP with IMT in a general population. Both morning and evening HBP provided equally valuable information for target organ damage, therefore physicians should use both HBP measurements as indicators in the management of hypertension. Further longitudinal study addressing the influence of morning and evening HBPs on cardiovascular risk is warranted to elucidate this issue.
Acknowledgments
We thank the staff of Division of Health and Welfare of Hisayama for their cooperation in this study.
Sources of Funding
This study was supported in part by Grants-in-Aid for Scientific Research (A) (16H02644 and 16H02692), (B) (16H05850), and (C) (26350895, 26460748, 15K09267, 15K08738, 15K09835, and 16K09244) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; by Health and Labour Sciences Research Grants of the Ministry of Health, Labour and Welfare of Japan (H25-Junkankitou [Seishuu]-Sitei-022, H26-Junkankitou [Seisaku]-Ippan-001, and H27-Shokuhin-[Sitei]-017); and by the Japan Agency for Medical Research and Development (AMED) (16dk0207025h0001, 16ek0210042h0002, and 16gm0610007h0204 (CREST)).
Conflict of Interest / Disclosures
None.
Supplementary Files
Supplementary File 1
Figure S1.
Correlation of morning and evening home blood pressures.
Table S1.
Clinical characteristics of participants according to evening HBP levels
Table S2.
ORs for advanced carotid wall thickening according to morning or evening HBP levels
Table S3.
Geometric averages of mean IMT according to morning or evening HBP levels among subjects with and without antihypertensive medication
Table S4.
Geometric averages of maximum IMT according to morning or evening HBP levels among subjects with and without antihypertensive medication
Table S5.
Geometric averages of mean IMT according to morning or evening HBP levels among subjects stratified by drinking status
Table S6.
Geometric averages of maximum IMT according to morning or evening HBP levels among subjects stratified by drinking status
Table S7.
Geometric averages of mean and maximum IMT according to HBP categories
Table S8.
Geometric averages of mean and maximum IMT according to HBP categories among subjects with and without antihypertensive medication
Table S9.
Geometric averages of mean and maximum IMT according to HBP categories
Table S10.
Geometric averages of mean and maximum IMT according to HBP categories (different cutoff values for morning and evening)
Table S11.
Geometric averages of mean and maximum IMT according to HBP categories among subjects with and without antihypertensive medication (different cutoff values for morning and evening)
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-16-1306
References
- 1.
Menard J, Chatellier G, Day M, Vaur L. Self-measurement of blood pressure at home to evaluate drug effects by the trough: peak ratio. J Hypertens Suppl 1994; 12: S21–S25.
- 2.
Stergiou GS, Efstathiou SP, Skeva II, Baibas NM, Roussias LG, Mountokalakis TD. Comparison of the smoothness index, the trough: peak ratio and the morning: evening ratio in assessing the features of the antihypertensive drug effect. J Hypertens 2003; 21: 913–920.
- 3.
Shimamoto K, Ando K, Fujita T Hasebe N, Higaki J, Horiuchi M, et al; Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res 2014; 37: 253–390.
- 4.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
- 5.
Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. Call to action on use and reimbursement for home blood pressure monitoring: A joint scientific statement from the American Heart Association, American Society of Hypertension, and the Preventive Cardiovascular Nurses’ Association. Hypertension 2008; 52: 10–29.
- 6.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a strong predictive power for mortality than does screening blood pressure measurement: A population-based observation in Ohasama, Japan. J Hypertens 1998; 16: 971–975.
- 7.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: Follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) Study. Circulation 2005; 111: 1777–1783.
- 8.
Matsui Y, Eguchi K, Shibasaki S, Ishikawa J, Shimada K, Kario K. Morning hypertension assessed by home monitoring is a strong predictor of concentric left ventricular hypertrophy in patients with untreated hypertension. J Clin Hypertens 2010; 12: 776–783.
- 9.
Ishikawa J, Hoshide S, Shibasaki S, Matsui Y, Kabutoya T, Eguchi K, et al; the JMS-1 Study Group. Relationship between morning hypertension identified by home blood pressure monitoring and brain natriuretic peptide and estimated glomerular filtration rate: The Japan Morning Surge 1 (JMS-1) Study. J Clin Hypertens 2008; 10: 34–42.
- 10.
Linsell CR, Lightman SL, Mullen PE, Brown MJ, Causon RC. Circadian rhythms of epinephrine and norepinephrine in man. J Clin Endocrinol Metab 1985; 60: 1210–1215.
- 11.
Kawasaki T, Cugini P, Uezono K, Sasaki H, Itoh K, Nishiura M, et al. Circadian variations of total renin, active renin, plasma renin activity, and plasma aldosterone in clinically healthy young subjects. Horm Metab Res 1990; 22: 636–639.
- 12.
Imai Y, Nishiyama A, Sekino M, Aihara A, Kikuya M, Ohkubo T, et al. Characteristics of blood pressure measured at home in the morning and in the evening: The Ohasama Study. J Hypertens 1999; 17: 889–898.
- 13.
Kawabe H, Saito I, Saruta T. Status of home blood pressure measured in morning and evening: Evaluation in normotensives and hypertensives in Japanese urban population. Hypertens Res 2005; 28: 491–498.
- 14.
Kawano Y, Pontes CS, Abe H, Takishita S, Omae T. Effects of alcohol consumption and restriction on home blood pressure in hypertensive patients: Serial changes in the morning and evening records. Clin Exp Hypertens 2002; 24: 33–39.
- 15.
Hackam DG, Quinn RR, Ravani P, Rabi DM, Dasgupta K, Daskalopoulou SS, et al. The 2013 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol 2013; 29: 528–542.
- 16.
Niiranen T, Jula A, Kantola I, Moilanen L, Kahonen M, Kesaniemi YA, et al. Home-measured blood pressure is more strongly associated with atherosclerosis than clinic blood pressure: The Finn-Home Study. J Hypertens 2007; 25: 1225–1231.
- 17.
Hanninen MR, Niiranen TJ, Puukka PJ, Kesaniemi YA, Kahonen M, Jula AM. Target organ damage and masked hypertension in the general population: The Finn-Home Study. J Hypertens 2013; 31: 1136–1143.
- 18.
Mancia G, Bombelli M, Brambilla G, Facchetti R, Sega R, Toso E, et al. Long-term prognostic value of white coat hypertension: An insight from diagnostic use of both ambulatory and home blood pressure measurements. Hypertension 2013; 62: 168–174.
- 19.
Tachibana R, Tabara Y, Kondo I, Miki T, Kohara K. Home blood pressure is a better predictor of carotid atherosclerosis than office blood pressure in community-dwelling subjects. Hypertens Res 2004; 27: 633–639.
- 20.
Hara A, Ohkubo T, Kikuya M, Shintani Y, Obara T, Metoki H, et al. Detection of carotid atherosclerosis in individuals with masked hypertension and white-coat hypertension by self-measured blood pressure at home: The Ohasama Study. J Hypertens 2007; 25: 321–327.
- 21.
Hata J, Ninomiya T, Hirakawa Y, Nagata M, Mukai N, Gotoh S, et al. Secular trends in cardiovascular disease and its risk factors in Japanese: Half-century data from the Hisayama Study (1961–2009). Circulation 2013; 128: 1198–1205.
- 22.
Arima H, Tanizaki Y, Yonemoto K, Doi Y, Ninomiya T, Hata J, et al. Impact of blood pressure levels on different types of stroke: The Hisayama Study. J Hypertens 2009; 27: 2437–2443.
- 23.
Fukuhara M, Arima H, Ninomiya T, Hata J, Yonemoto K, Doi Y, et al. Impact of lower range of prehypertension on cardiovascular events in a general population: The Hisayama Study. J Hypertens 2012; 30: 893–900.
- 24.
Fukuhara M, Arima H, Ninomiya T, Hata J, Hirakawa Y, Doi Y, et al. White-coat and masked hypertension are associated with carotid atherosclerosis in a general population: The Hisayama Study. Stroke 2013; 44: 1512–1517.
- 25.
Coleman A, Freeman P, Steel S, Shennan A. Validation of the Omron 705IT (HEM-759-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press Monit 2006; 11: 27–32.
- 26.
Yanase T, Nasu S, Mukuta Y, Shimizu Y, Nishihara T, Okabe T, et al. Evaluation of a new carotid intima-media thickness measurement by B-mode ultrasonography using an innovative measurement software, Intimascope. Am J Hypertens 2006; 19: 1206–1212.
- 27.
Hoshide S, Kario K, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, et al; the J-HOP Study Group. Association of morning and evening blood pressure at home with asymptomatic organ damage in the J-HOP Study. Am J Hypertens 2014; 27: 939–947.
- 28.
Chonan K, Hashimoto J, Ohkubo T, Tsuji I, Nagai K, Kikuya M, et al. Insufficient duration of action of antihypertensive drugs mediates high blood pressure in the morning in hypertensive population: The Ohasama Study. Clin Exp Hypertens 2002; 24: 261–275.
- 29.
Grassi G, Bombelli M, Seravalle G, Dell’Oro R, Quarti-Trevano F. Diurnal blood pressure variation and sympathetic activity. Hypertens Res 2010; 33: 381–385.
- 30.
Kohara K, Nishida W, Maguchi M, Hiwada K. Autonomic nervous function in non-dipper essential hypertensive subjects: Evaluation by power spectral analysis of heart rate variability. Hypertension 1995; 26: 808–814.
- 31.
Pecis M, Azevedo MJ, Moraes RS, Ferlin EL, Gross JL. Autonomic dysfunction and urinary albumin excretion rate are associated with an abnormal blood pressure pattern in normotensive normoalbuminuric type 1 diabetic patients. Diabetes Care 2000; 23: 989–993.
- 32.
Asayama K, Ohkubo T, Kikuya M, Obara T, Metoki H, Inoue R, et al. Prediction of stroke by home “morning” versus “evening” blood pressure values: The Ohasama Study. Hypertension 2006; 48: 737–743.
- 33.
Niiranen TJ, Johansson JK, Reunanen A, Jula AM. Optimal schedule for home blood pressure measurement based on prognostic data: The Finn-Home Study. Hypertension 2011; 57: 1081–1086.
- 34.
Kario K, White WB. Early morning hypertension: What does it contribute to overall cardiovascular risk assessment? J Am Soc Hypertens 2008; 2: 397–402.
- 35.
Kario K, Ishikawa J, Pickering TG, Hoshide S, Eguchi K, Morinari M, et al. Morning hypertension: The strongest independent risk factor for stroke in elderly hypertensive patients. Hypertens Res 2006; 29: 581–587.
- 36.
Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: A prospective study. Circulation 2003; 107: 1401–1406.