2017 年 81 巻 2 号 p. 153-154
2017 年 81 巻 2 号 p. 153-154
As Japan is well on the way to being an aging society with a declining population, the increasing number of patients of heart failure (HF) is becoming a serious social problem.1 A recent report using a nationwide claim-based database, the Japanese Registry of All Cardiac and Vascular Diseases (JROAD)-DPC, has demonstrated that Japanese HF patients are relatively old, particularly in the women, and the peak age is 80–89 years in both men and women.2 HF with preserved ejection fraction (HFpEF) is observed in approximately one-half of patients with HF and the prognosis of HFpEF is as poor as that of HF with reduced EF (HFrEF).3 The characteristic features of HFpEF are higher age and higher prevalence of females, hypertension, diabetes, and atrial fibrillation, compared with HFrEF.4 Nocturnal BP elevation, such as the riser and non-dipper patterns of the circadian BP rhythm on the ambulatory BP measurements (ABPM), is strongly associated with hypertensive organ damage.5 However, it is still unknown whether abnormal circadian BP changes are associated with the prognosis of HF patients.
Article p 220
In this issue of the Journal, Komori et al report that HFpEF patients with the riser pattern at baseline showed a higher incidence of the composite of all-cause death and cardiovascular events (coronary events, HF re-hospitalization, and stroke), as compared with those with the dipper pattern, based on a prospective, observational, multicenter cohort study.6 Moreover, they demonstrate that the riser pattern was an independent predictor for the adverse outcomes in HFpEF patients, but not HFrEF patients. Preceding this longitudinal analysis, the authors performed a cross-sectional analysis of the baseline data of their HF cohort and demonstrated that the riser pattern was a significant factor associated with HFpEF, but not HFrEF.7 A series of their studies had the advantage that patient number was relatively larger than in previous studies of hospitalized HF patients who underwent ABPM. However, the mechanisms underling the different effect of the riser pattern on cardiovascular events and all-cause death in HFpEF and HFrEF patients still remain unclear at present. The body fluid retention related to the increased salt-sensitivity, obesity, and diabetes, the increased arterial stiffness due to aging and hypertension, and the impairment of baroreceptor reflex system and/or sympathetic nerve system are frequently found in patients with the riser pattern. Patients with the left ventricular diastolic dysfunction and the increased arterial stiffness with/without the impaired neural regulation are vulnerable to the ventricular-arterial interaction mismatch upon BP elevation, resulting in acute decompensation of HFpEF (Figure).8,9 A fluid volume shift from the extremities to the heart would trigger acute pulmonary edema during sleep in the HFpEF patients, particularly those with the fluid retention.10,11 Moreover, atrial fibrillation and non-cardiovascular comorbidities, including anemia, sleep-disordered breathing and chronic obstructive pulmonary disease, may have a role in the association between the riser pattern and HFpEF.12 However, these factors are not necessarily specific for HFpEF. The mechanism of the differential effects of the riser pattern on HFpEF and HFrEF is awaited to be determined.
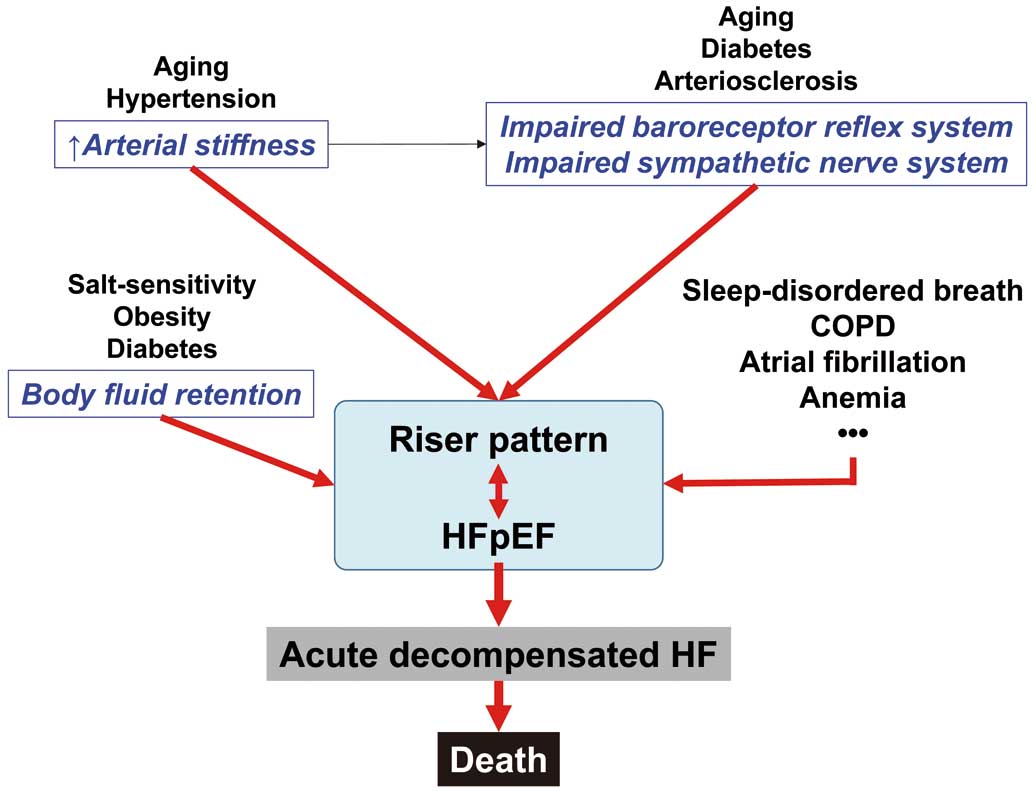
Possible common pathogenesis of heart failure with preserved ejection fraction (HFpEF) and the riser pattern of blood pressure. COPD, chronic obstructive pulmonary disease.
This study raises a possibility that nocturnal BP elevation would be a novel therapeutic target for improving the outcomes of HFpEF patients. Because thiazide diuretics normalize circadian BP changes from abnormal non-dipper pattern to normal dipper pattern,13 it is suggested that thiazide diuretics may be a suitable option for treatment of the riser pattern in HFpEF patients. Recently, the Systolic Blood Pressure Intervention Trial (SPRINT) and a subanalysis of the SPRINT enrolling elderly patients aged ≥75 years have demonstrated that intensive systolic BP reduction reduces fatal and non-fatal major cardiovascular events and all-cause death in patients at high risk for cardiovascular events but without diabetes.14,15 And, the EMPA-REG OUTCOME trial has shown that empagliflozin, a sodium-glucose cotransporter 2 (SGLT2) inhibitor, decreases major cardiovascular events and all-cause death in diabetic patients at high cardiovascular risk.16 Similar results were obtained from a HF subanalysis of the EMPA-REG OUTCOME trial.17 It is noteworthy that the reduction of cardiovascular events and cardiovascular death was attributable mainly to the reduction of HF in both the SPRINT and EMPA-REG OUTCOME trials. The thiazide-based regimen was adopted for the intensive BP lowering in the SPRINT. It is considered that SGLT2 inhibitors possess a thiazide-like diuretic action.18 Although the cardiac function was not assessed in the SPRINT and the ENPA-REG OUTCOME trials, it is interesting to discuss whether thiazide diuretics and empagliflozin might reduce HF and resultant HF death by improving the abnormal nocturnal BP elevation in patients enrolled in these trials. This issue should be addressed in future study.
None.