2018 年 82 巻 2 号 p. 464-468
2018 年 82 巻 2 号 p. 464-468
Background: Because infective endocarditis (IE) carries a high risk of morbidity and mortality, rapid diagnosis and effective treatment are essential to achieving a good patient outcome. However, the diagnosis of IE is often difficult in patients presenting with nonspecific clinical manifestations. An association between IE and hypointense signal spots on brain T2*-weighted magnetic resonance imaging (MRI) has been reported, but the clinical significance remains unclear.
Methods and Results: To assess the clinical importance of silent lesions in the brains of IE patients, hypointense signal spots detected on their brain T2*-weighted MRI scans were investigated in a retrospective review of 44 consecutive patients with definite or suspected IE evaluated by MRI between June 2006 and January 2014. Hypointense signal spots on T2*-weighted MRI were detected in 37 (84%) patients; of these, 21 (46%) had ischemic lesions, 10 (22%) had subarachnoid hemorrhage, 4 (9%) had intraparenchymal hemorrhage, and 4 (9%) had infectious aneurysm. The hypointense signal spots on T2*-weighted images were preferentially distributed in cortical areas.
Conclusions: T2*-weighted hypointense signal spots are highly frequent in patients with IE and their presence may be informative in the monitoring of IE-associated brain lesions, even those that are neurologically asymptomatic. The strong association between IE and T2*-weighted hypointense signal spots supports the need to consider additional criteria in the diagnosis of IE.
Infective endocarditis (IE) carries a high risk of severe morbidity and mortality.1–6 Rapid diagnosis and treatment are essential to a good patient outcome but are often difficult in patients presenting with nonspecific clinical manifestations. Although the modified Duke criteria guide the diagnosis of IE,7 with a sensitivity and specificity of >90%,8 confirmation of their major standards requires patient hospitalization and the results are not rapidly obtained, but the minor standards are nonspecific and include minor changes that are easily overlooked.
An association between IE and brain magnetic resonance imaging (MRI) abnormalities has been reported. Specifically, 10–70% of patients with IE have abnormal cerebral lesions on T2*-weighted MRI.6,9–11 Thus, some studies have suggested neuroimaging for all IE patients, even those without clinical neurological symptoms.12 MRI is minimally invasive and provides a wealth of information, including the detection of microaneurysm, but the clinical significance of the findings in IE patients is unclear. The aim of this study was to evaluate the utility of MRI in the early diagnosis of IE.
We retrospectively reviewed consecutive patients with IE treated at Nagasaki University Hospital from June 2006 to January 2014. All patients were diagnosed with IE according to the modified Duke criteria. This study included only patients who underwent brain T2*-weighted MRI, although when the imaging was performed was not specified. Patients were excluded if they had undergone emergency cardiac surgery during the first 24 h after admission. Both the initial and follow-up imaging scans were carried out using 1.5- or 3-Tesla MRI with a standard head coil. Clinical presentation, MRI findings, and treatment were retrospectively evaluated in the 44 patients with IE who met the inclusion criteria. During the study period, 77 patients were diagnosed with IE, but 33 patients were excluded because of emergency cardiac surgery without brain MRI evaluation.
The clinical characteristics and MRI findings of the 44 patients are summarized in Table 1 and Table 2, respectively. The most common initial symptom was fever (n=34, 77%), followed by neurological symptoms and arthralgia (n=7, 16%). The remaining 3 patients (7%) had cardiovascular symptoms, respiratory failure, and general fatigue. The interval between the clinical manifestation and the diagnosis of IE ranged from 2 days to 5 months, with a median of 36 days. Cardiac surgery was performed in 37 (84%) patients and neurologic surgery in 7 patients (16%). In-hospital mortality rate was 7% (3 patients). Intracranial abnormalities were identified on the brain MRI scans of 37 patients (84%). All patients had intracerebral hemorrhages, including hypointense spots on T2*-weighted MRI. The patients complicated by subarachnoid hemorrhage numbered 10 (23%), by cerebral infarct in 21 (48%), and by intracranial aneurysm in 4 patients (9%). All aneurysms were detected by MR angiography and confirmed by CT angiography; 3 aneurysms were located in the middle cerebral artery and 1 was in the posterior cerebral artery. There were no cases of multiple aneurysms and no relationship with hypointense signal spots was recognized. Follow-up MRI was performed in 18 patients; the interval between initial and follow-up MRI ranged from 6 days to 2 months. An increased number of hypointense signal spots since the first scan was found in 11 of them (61%). The median C-reactive protein (CRP) level on admission was 8.17 mg/dL and tended to be higher in patients with T2* hypointense signal spots on their MRI scans (Figure 1).
| Characteristics | |
|---|---|
| Age (years) | 59±18 |
| Sex (male), n (%) | 23 (52) |
| Hypertension, n (%) | 18 (41) |
| Affected heart valve, n (%) | |
| Aortic | 10 (23) |
| Mitral | 19 (43) |
| Aortic and mitral | 6 (14) |
| Other | 10 (23) |
| Clinical presentation, n (%) | |
| Cardiovascular or respiratory failure | 3 (7) |
| Prolonged fever | 34 (77) |
| Neurological symptoms | 7 (16) |
| Arthralgia | 7 (16) |
| CRP level at admission (mg/dL) | 8.2±8.2 |
| Hypointense signal spot positive | 8.8±8.6 |
| Hypointense signal spot negative | 4.8±3.9 |
| Interval between onset and diagnosis (days) | 36±34 |
| Surgical care, n (%) | |
| Cardiac surgery | 37 (84) |
| Neurologic surgery | 4 (9) |
| Death at 3 months, n (%) | 3 (7) |
Data are mean±SD or n (%). CRP, C-reactive protein; IE, infective endocarditis; MRI, magnetic resonance imaging.
| Cerebral lesions | |
|---|---|
| Ischemic lesion, n (%) | 21 (48) |
| Hemorrhagic lesion, n (%) | |
| Intraparenchymal hemorrhagic lesion | 4 (9) |
| T2* hypointense signal spot | 37 (84) |
| Subarachnoid hemorrhage, n (%) | 10 (23) |
| Intracranial aneurysm, n (%) | 4 (9) |
IE, infective endocarditis; MRI, magnetic resonance imaging.
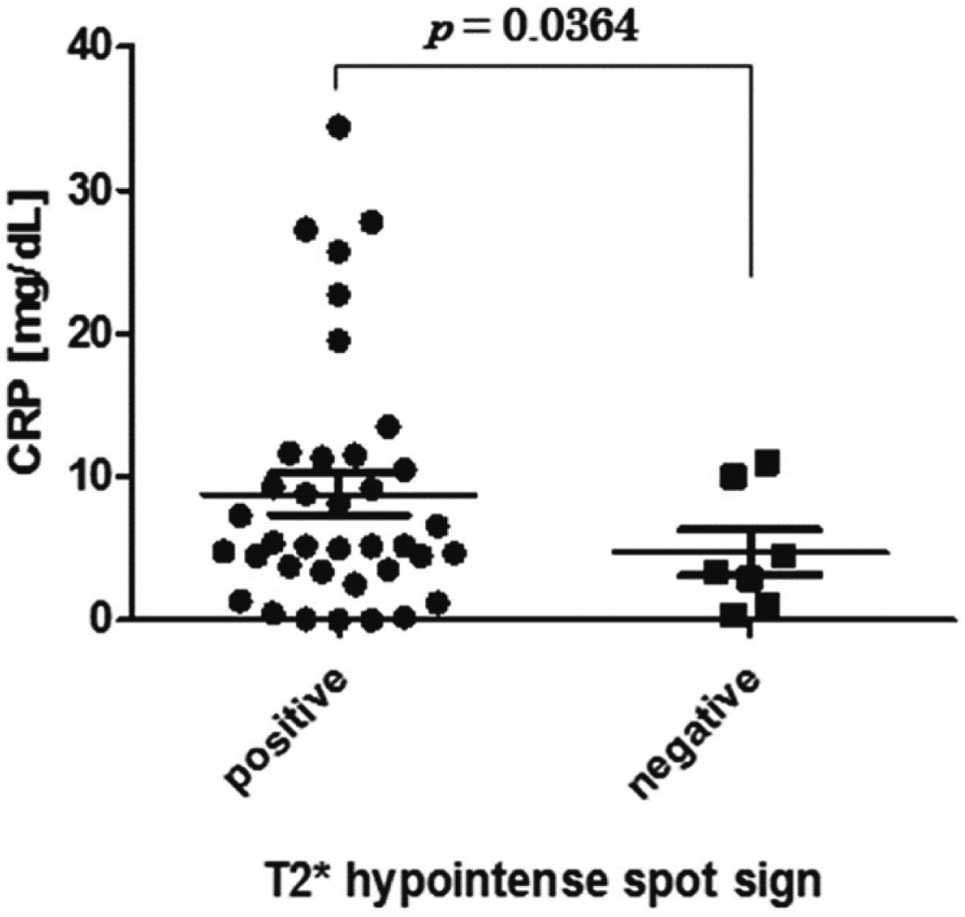
C-reactive protein (CRP) levels on admission of patients with infective endocarditis show a tendency to be higher in patients with hypointense signal spots on T2*-weighted magnetic resonance imaging (P=0.036; unpaired t-test with Welch’s correction).
The in-hospital mortality rate of IE patients is as high as 15–20% and the 1-year rate is 40%.13–15 However, physicians may overlook the core diagnosis of IE because patients typically present with mild and nonspecific symptoms, such as fever, arthralgia, and general fatigue, during the early manifestation. The modified Duke criteria are useful in the diagnosis of IE because of their high sensitivity and specificity,8 but confirmation of the major standards requires hemoculture and transesophageal echocardiography, which are invasive and do not yield rapid results.16,17 In addition, the minor criteria are nonspecific and do not greatly aid in the diagnosis.18 Therefore, the Duke criteria are of limited use in clinical practice. Delay in diagnosis and thus in treatment result in damage progression and adverse sequelae. In our study, the median period from onset to diagnosis was relatively long, 36 days, which may have been related to the prognosis of the patients. Multidetector CT angiography and 18F-fluorodeoxyglucose PET-CT can detect perivalvular complications and may improve the diagnosis of IE,19 but they are not available for routine clinical use. A recent study demonstrated the utility of brain MRI in patients with IE, with T2*-weighted MRI having particularly high sensitivity in this setting.6,20 It suggested that the T2*-weighted MRI findings can provide novel, additional criteria for the diagnosis of IE.2,11 In our study, 84% of patients had hypointense signal spots on the T2*-weighted images, a value higher than in other studies,20 but probably attributable to the serious condition of most of the patients, as 84% underwent cardiac surgery. In this group, the abnormal finding on the T2*-weighted MRI may have been indicative of the severity of the disease, which was also confirmed by the CRP value on admission. Prolonged fever was a frequent finding in patients with IE; 81% patient with hypointense signal spots had prolonged fever, compared with 57% patients without hypointense spots and prolonged fever. In addition, the median CRP level on admission tended to be higher in patients with hypointense spots, so it might be related to the progress of the IE. Patients without hypointense spots had relatively mild symptoms such as arthralgia and general fatigue. All 7 neurologically symptomatic patients had hypointense spots, whereas 30 of 37 asymptomatic patients (81%) had hypointense spots. Hypointense signal spots are a highly frequent finding in patients with IE, even those who are neurologically asymptomatic. Interestingly, all 7 patients without hypointense spots achieved a good neurological outcome at 90 days after diagnosis of IE. Recent studies have focused on diagnosis and treatment decisions in patients with IE, but there are few studies describing the MRI findings or their relationship to disease severity. Hypointense signal spots on T2*-weighted MRI are also observed in chronic hypertension, changes of an arteriosclerotic nature, and amyloid angiopathy.21,22 In a cross-sectional study of 1,965 elderly subjects in Framingham, 78% of the patients with hypointense signal spots had hypertension, and the prevalence of patients with hypointense signal spots increased with age.23 In our study, only 41% patients with hypointense signal spots had hypertension, and hypointense signal spots appeared in patients with regardless of age. However, most patients with IE have multiple lesions that predominantly appear in the cortical areas.24,25 In our study, 86% of patients with hypointense signal spots had multiple lesions, almost all of which were located in the cortex, subcortex, and around the sulci (Figure 2). Ajay et al reported that susceptibility-weighted MRI imaging (SWI) is a more sensitive diagnostic technique for detecting IE.26 SWI has been shown to be more sensitive than T2*-weighted MRI for detecting cerebral microbleeds, irrespective of the location of the cerebral microbleeds. However, SWI might detect susceptibility effects within veins as cerebral microbleeds. We selected T2*-weighted MRI to detect hypointense signal spots for IE to avoid over-diagnosis. The preference for these sites may facilitate the distinction between IE and the aforementioned pathologies (Figure 3). In addition, in IE, new lesions often appear within a short period.11,27 In our study, the number of hypointense spots had increased on the second scans of 11 (61%) of the 18 patients who underwent a second MRI. This suggests that the hypointensity spots on T2*-weighted MRI did not simply indicate microbleeds, but pathologies such as vasculitis, thrombotic aneurysm, infarct, and bleeding as well. Champey et al reported that 70% of IE patients had abnormal brain MRI findings but that these abnormalities did not significantly affect either the diagnosis or the surgical treatment plan.10 Although the modified Duke criteria may suffice for a reliable diagnosis of IE, brain MRI, in addition to being noninvasive and yielding rapid results, reveals not only the presence but also the severity of the disease and related pathologies. We recommend that patients with findings suggestive of IE undergo MRI as soon as possible, and, in ambiguous cases, a follow-up MRI, to improve the early diagnosis and treatment of the disease and therefore patient outcome.
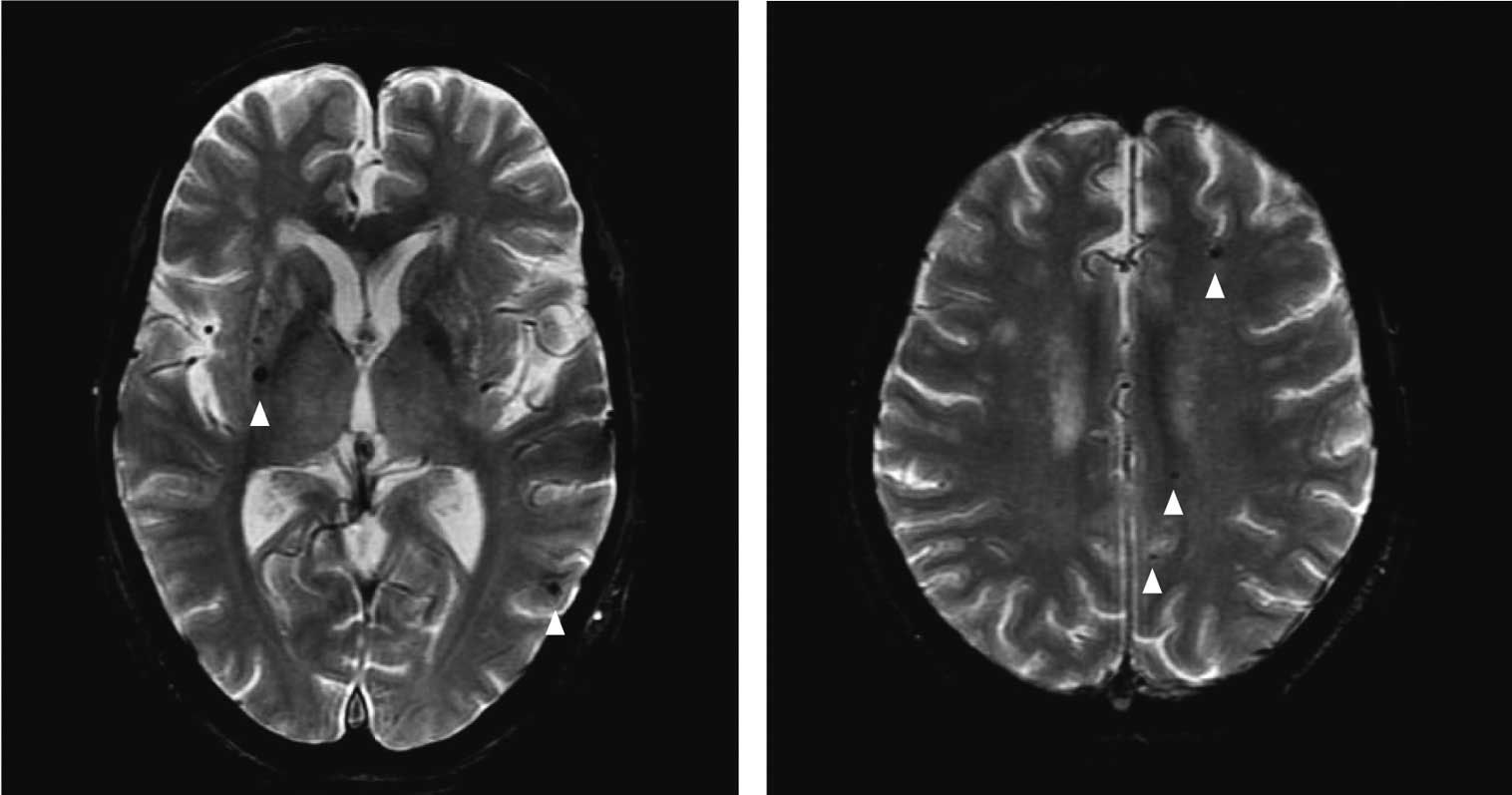
T2*-weighted magnetic resonance imaging shows multiple hypointense signal spots (arrowheads) in the cortex and paraventricular regions of a patient with infective endocarditis.

Hypointense signal spots on the T2*-weighted magnetic resonance images of patients with infective endocarditis. The number of hypointense spots increased asymptomatically despite antibiotic therapy in these patients.
Several limitations of this study should be addressed. First, it was a retrospective analysis with a small sample size. Second, because the institute in which the study was conducted is a tertiary referral hospital, our study might have included a larger proportion of patients in a serious condition, resulting in selection bias. Third, the hospital does not have a well-defined management protocol for patients with IE, and differences in treatment may have influenced the comparisons in this study. The further accumulation of cases and adoption of a set protocol for the management of IE patients are necessary.
Our results suggested that brain MRI has a role to play in IE, both diagnostically and in the detection of related pathologies such as arteritis, subclinical microbleeds, and infectious microaneurysm. Hypointense signal spots on T2*-weighted MRI are a very frequent finding in patients with IE and their presence may be useful in monitoring IE-associated brain lesions even if the patient is asymptomatic. The strong association between IE and hypointense signal spots on T2*-weighted MRI supports the need for further evaluation of including this finding as an additional diagnostic criterion of IE.
No financial support for this work.