2018 年 82 巻 2 号 p. 606-607
2018 年 82 巻 2 号 p. 606-607
A 77-year-old woman with aortic regurgitation, mitral valve regurgitation, tricuspid valve regurgitation and chronic atrial flutter underwent surgery for aortic valve replacement, mitral valve plasty, tricuspid valve plasty, and maze procedure. After developing postoperative reduction in platelet count, seizure, and hemiplegia, she was diagnosed with heparin-induced thrombocytopenia (HIT) based on positive HIT antibody test. She was treated with therapeutic-dose argatroban under a diagnosis of HIT; nevertheless, seizure, hemiplegia, melena, and respiratory failure progressed. To detect complications due to HIT with thrombosis (HITT), dual-energy 64-slice computed tomography and 1.5-T magnetic resonance imaging were carried out, but lung embolization, acute cerebral infarction, and cerebral venous sinus thrombosis were not able to be visualized. Multiple organ failure rapidly developed, and the patient died on the 15th postoperative day.
An autopsy was performed 37 h after death. The macroscopic findings consisted of massive necrosis of the small and large intestine, multiple pulmonary hemorrhagic infarctions, and spotty hemorrhagic pancreatic necrosis. No thrombus or stenosis was confirmed in the large supply arteries such as the superior and inferior mesenteric arteries and the celiac artery.
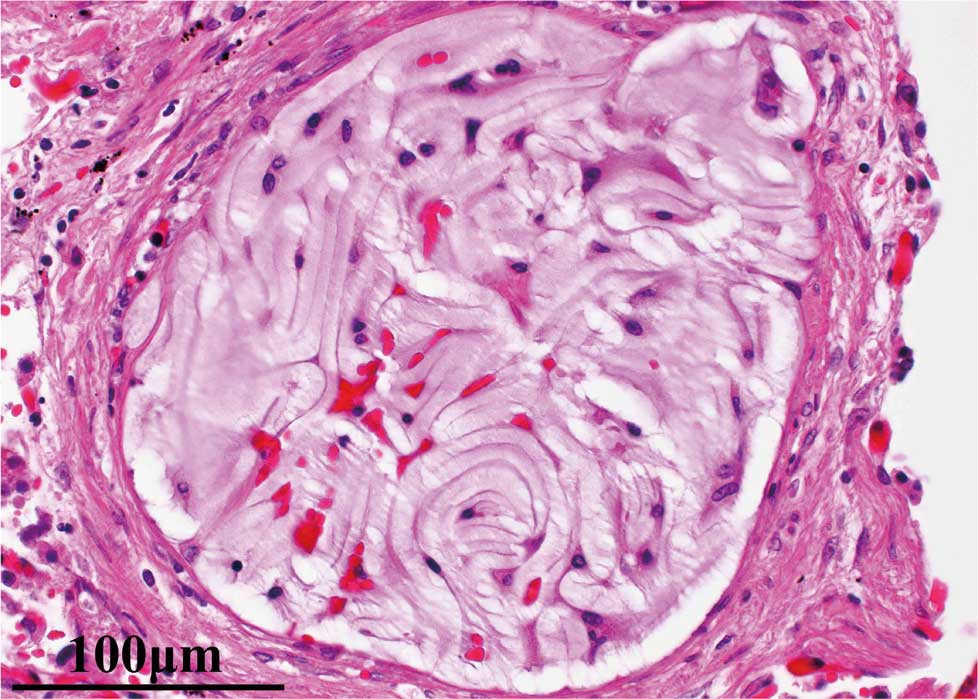
On microscopy, there were micro-thrombi in multiple organs (brain [Figure 1], lung, adrenal gland, spleen, and pancreas, among others), although postmortem autolysis was significant in some organs, such as the gastrointestinal tract. A thrombus in the cerebral venous sinus was also found, prompting suspicion that these thrombi in peripheral vessels might have been the cause of the seizure.

Histopathology at the sites of the small vessels in the left frontal cortex of the cerebrum. (A) Occlusion of the small vessels with granular thrombi on hematoxylin-eosin staining. (B) Positive thrombus on immunostaining with CD42b antibody. (C) Phosphotungstic acid-hematoxylin staining of the thrombus showing a negative reaction for fibrin.
Platelets were immunostained by CD42b antibody, and fibrin was stained by phosphotungstic acid-hematoxylin. On histopathology, the small vessels were occluded by granular platelet-rich thrombi (Figure 1). Additionally, a few hydrophilic polymer emboli were present in the lungs (Figure 2).
Histopathology of the left upper lobe of the lung: hydrophilic polymer embolisms in the peripheral pulmonary arteries on hematoxylin-eosin.
The main cause of death was diagnosed as HITT, specifically due to the presence of necrosis of the small and large intestine and pulmonary infarction.
Hydrophilic polymer embolism is an underdiagnosed phenomenon that has only recently been recognized.1 Due to the advantages of lubrication and biocompatibility, coating substances are widely used in medical devices for minimally invasive diagnostic and therapeutic cerebrovascular, cardiovascular and peripheral procedures. Polymer emboli involving the lung were first documented as an embolization of hydrophilic coating of a central venous catheter, which resulted in the development of cavitary lung nodules.2 Reports of these complications have increased in recent years.3 Indeed, 13% of hospital autopsy cases (18/136) involve hydrophilic embolization in the lung, and only 6 of these 18 cases had lung disease (respiratory insufficiency, acute pulmonary embolism, and pneumonia) as a clinical cause of death.1 We suspect that hydrophilic polymer embolization in the lung is not typically a critical cause of death, unlike embolization in the coronary or cerebral arteries. Friction between devices and excess friction between devices and the vessel walls during cannulation may also play a role in the development of complications.3
In the present case, although heparin was withdrawn and replaced by argatroban on the 10th postoperative day, thromboembolisms due to HIT occurred in multiple organs. We herein report this instructive autopsy case of thromboembolisms in multiple organs due to HIT. In addition, as an adverse event, we report hydrophilic polymer embolism in the lung. Hydrophilic polymer embolization may occur more often than suspected. Due to sampling limitations, it is difficult to determine the relative incidence of hydrophilic polymer embolization. To our knowledge, this is the first English-language report of hydrophilic polymer embolism in the lung in Japan.
This finding of hydrophilic polymer embolism seems to have been an incidental adverse event and not the main cause of death. It is important, however, to take every adverse event into account given the widespread application of new devices. The clinical significance of hydrophilic polymer emboli at the microvascular level of pulmonary arteries is thus expected to be elucidated in further studies.
We would like to express our deepest appreciation to Dr. Shigeki Miyata and Dr. Takuma Maeda in the National Cerebral and Cardiovascular Center in Japan for their careful guidance, prompt HIT antibody measurement and invaluable discussions.
The authors declare no conflict of interest.