2018 年 82 巻 2 号 p. 332-333
2018 年 82 巻 2 号 p. 332-333
Atherosclerosis is characterized by subendothelial cholesterol storage and involves a complicated cascade of chronic vascular inflammation. Statin and nonstatin low-density lipoprotein cholesterol (LDL-C) lowering medications, such as ezetimibe, fibrates, bile acid sequestrants, niacin, cholesteryl ester transporter protein inhibitors, and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, have shown linear relative risk reduction per change in LDL-C.1 The PCSK9 inhibitors are potent LDL-C lowering medicines even compared with LDL apheresis.2 Recently, a secondary analysis of the FOURIER study using a PCSK9 inhibitor demonstrated a monotonic relationship of major cardiovascular events with achieved LDL-C levels of <10 mg/dL in patients with established cardiovascular diseases.3 However, more than 8% of these patients, whose LDL-C levels were <20 mg/dL, exhibited a recurrence of major cardiovascular events during a 2.2 year of observation period.3 Thus, a “residual risk” persists even after aggressive LDL-C lowering therapy.
Article p 596
From approximately 50 years ago, a lower incidence of ischemic heart disease was documented in Greenlandic Inuit, who consumed extremely high amounts of animal fat from fish and marine mammals. Thereafter, inverse associations between fish consumption and death from ischemic heart disease were reported from the rest of the world. Because n-3 polyunsaturated fatty acids (n-3 PUFA), such as eicosapentaenoic acid (EPA, 20:5n3) and docosahexanoic acid (DHA, 22:6n3), are abundant in fish oils, they are believed to have antiatherogenic properties. The EPA/arachidonic acid ratio was reported to predict major adverse cardiovascular events in patients who undergo percutaneous coronary intervention.4 However, multiple prospective randomized placebo-controlled studies in the past decade have failed to show a decrease in cardiovascular events by n-3 PUFA supplementation in patients with a high cardiovascular risk.5–7 The optimal medical therapies introduced to those populations may explain the negative results. There are few prospective open-label interventional trials that have shown a reduction of composite cardiovascular events.8,9 One of the most likely cardioprotective mechanisms is stabilization of ischemia-induced myocyte resulting in ischemia-induced ventricular fibrillation and sudden cardiac death.10 Thus, questions remain on whether n-3 PUFAs are truly antiatherogenic.
In the past, large-scale observational cohort studies have revealed risk factors of diseases or an outcome. Although known confounding factors have been corrected, it is impossible to correct for all the “unknown” confounding factors that may be present in these cohort study. Thus, the prospective randomized double-blind placebo-controlled trial has become the gold standard for finding a causal relationship between risk factors and outcomes. Recently, a Mendelian randomization study (MRS)11 detected causality between a risk factor (usually a biomarker) and an outcome. A genetic variant associated with a particular biomarker, instead of its values, was used as a proxy, and outcomes were compared between the groups harboring the effect allele and the reference allele.11 The MRS as well as a prospective randomized double-blind placebo-controlled trial indicated LDL-C as a strong causal risk factor of atherosclerotic diseases, whereas some risk factors, such as high-density lipoprotein (HDL) cholesterol, C-reactive protein, and uric acid, detected by the observational study, did not show any significant relationship with atherosclerotic cardiovascular diseases in the MRS.
The vast majority of n-3 PUFAs are derived directly from the diet; EPA and DHA can also be produced from essential α-linoleic acid by several desaturation and elongation steps. Thus, the catalyzing enzymes of the n-3 PUFA metabolic pathway are thought to be the determinants of their levels (Figure), and the candidate genes associated with n-3PUFAs levels have been detected.12 However, no genes associated with n-3 PUFAs were identified as a cause of coronary artery disease in the latest comprehensive genome-wide association study.13 Thus, pathophysiological studies to show the antiatherogenic effects of n-3 PUFAs are also needed.
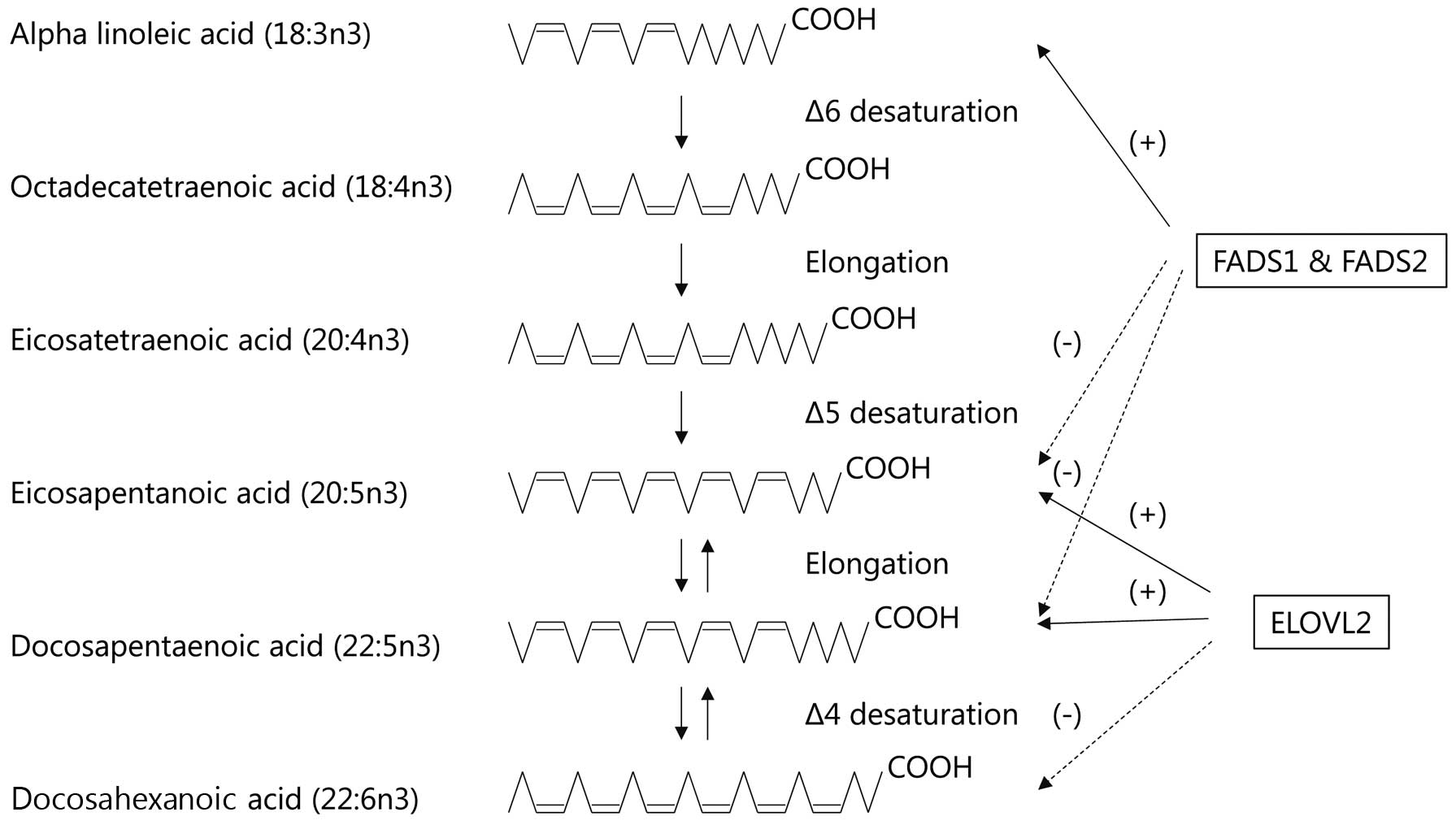
The n-3 polyunsaturated fatty acid metabolic pathway. The genome-wide significant associations of two loci with each fatty acid are shown. The solid and dashed lines indicate positive and negative directions, respectively. ELOVL, elongation of very long chain fatty acids protein; FADS, fatty acid desaturase.
In this issue of the Journal, Tanaka and colleagues investigate whether reconstituted HDL (rHDL) containing different amounts of EPA-phosphatidylcholine had antiatherogenic properties.14 They report a dose-dependent reduction in the expression of cytokine-stimulated vascular cell adhesion molecule-1 by rHDL containing EPA-phosphatidylcholine. Moreover, rHDL rich in EPA increased cholesterol efflux and the production of EPA-derived metabolites, anti-inflammatory resolvin E3 and its intermediate metabolites 18-hydroxyeicosapentaenoic acid. However, the results should be carefully interpreted. As the authors mention in the study limitations, the EPA proportion within the rHDL particles for this study was beyond physiological levels.14 Previously, the same research group demonstrated similar antiatherogenic effects in dyslipidemic patients who were orally administered high-dose EPA (1.8 g).15 In that human study, EPA/arachidonic acid ratios in HDL particles before and after EPA therapy were estimated as 0.4 and 1.25, respectively.15 The EPA/arachidonic acid ratios of rHDL (low, 20; intermediate, 80; high, 100) in the present study were 4.9, 72.9, and 257.0, respectively. Moreover, anti-inflammatory, antioxidative, and cholesterol efflux capacities were evident at the highest concentration of EPA.14 Thus, it is hard to expect the same effects in vivo.
Antiatherogenic effects of n-3 PUFAs in human, if they exist, may be multifactorial, such as improvements in lipoprotein metabolism; antiinflammatory, antioxidant and, antithrombotic effects; plaque stabilization, etc., and are not fully solved yet. Hopefully, well-designed prospective randomized double-blind placebo-controlled trials or MRS enrolling low fish-consuming populations will be conducted to show the causality of n-3 PUFAs for atherosclerosis.
M. Kawashiri received lecture fees from Amgen Astellas Biopharma K.K. and Astellas Pharma Inc.