2018 年 82 巻 2 号 p. 609-610
2018 年 82 巻 2 号 p. 609-610
We thank Dr. Kounis and colleagues for thier interest in our article.1 They raise issues concerning the increased incidence of restenosis and thrombosis associated with bioresorbable vascular scaffolds (BVS) and suggest that hypersensitivity to PLLA/PDLLA, everolimus and the 4 platinum markers induce systemic reactions, which may induce restenosis and thrombosis. Also, they suggest that the acidosis induced by the PLLA degradation process may eventually decrease activated partial thromboplastin and thus provoke thrombus formation. Although this is a very important issue to understand in the physiology of BVS, we would like to point out some erroneous assumptions that may be misleading.
First, regarding hypersensitivity to PLLA, the incidence of hypersensitive reactions to PLLA screws is very low compared with the vast amount of orthopedic procedures performed. Also, the “dose” or size of a bioresorbable implant is important in inducing a biological response. In other words, unlike bone screws which have a large volume and mass, the largest Absorb scaffold (3.5×28 mm) contains approximately 18.8 mg of the polylactide polymer (PLLA), which is a small amount to induce a systemic hypersensitivity. Moreover, in the case series report of allergic granulomatous reaction to injectable PLLA gel, the authors of that case series mentioned that other dermal implants (e.g., collagen, silicone, polyalkylimide, polyacrylamide, hyaluronic acid, Gore-Tex and methacrylate) also elicit a granulomatous ous reaction. This was also mentioned in a review paper by Lowe et al,2 who stated that granuloma formation is influenced by the implantation technique and the concentration of the injected material.
Second, everolimus is the active pharmaceutical ingredient used in various DES, with established safety and efficacy. Although Kounis et al provide a reference for hypersensitivity reactions to everolimus, the dose of a pharmaceutical is important in inducing a biological response. Hypersensitivity reactions have been reported in cancer and immunosuppressive therapies, which used a daily dose of 1–10 mg everolimus for extended periods.3,4 In comparison, the everolimus dose on the largest Absorb scaffold is approximately 0.31 mg and present as a single controlled-release dose. In particular, everolimus is used in the Xience stent, which has been the active comparator in various studies, meaning that everolimus cannot be the cause of “increased” adverse effects.
Third, Kounis et al provide examples of hypersensitivity to platinum salts. However, the platinum markers in Absorb are made of the pure metal, which is a noble metal with high resistance to corrosion.5 Platinum salt and pure platinum metal are completely different chemical compounds, having scarce common points in their chemical and biological properties. Moreover, the reference for the hypersensitivity reactions to taxanes seems to have little to do with the Absorb scaffold.
Another important issue that Kounis et al have raised is the acidosis that is induced during the process of Absorb degradation. Although it is true that acidosis can have harmful effects on the local coronary vasculature, it is very unlikely that the lactic acid produced by Absorb degradation induces a significant acidic condition, based on the following data.
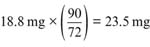
1. The average polymer weight of the largest size 3.5×28 mm Absorb is 18.8 mg, and the total amount of lactic acid generated from this scaffold is 23.5 mg (the molecular weight of PLA repeating unit is 72 Daltons and the molecular weight of lactic acid is 90 Daltons).
2. Assuming that an Absorb stent is fully degraded in 2 years, the average lactic acid release rate from one 3.5×28 mm Absorb is 0.25 nmol/min.
23.5 mg÷90 Daltons÷(1,051,200 min (2 years))=2.5*10−7 mmol/min=0.25 nmol/min
3. Endogenous lactic acid is approximately 280–360 mg at rest and can rise to levels as high as 3,600–4,500 mg during exercise; the normal human plasma lactate concentration at 0.3–1.3 µmol/mL.6,7 Also, a normal 28-mm coronary vessel has approximately 0.07 mL of interstitial fluid. The amount of interstitial endogenous lactate in a 3.5×28-mm vessel in the resting state can be estimated as 28 nmol.
0.3 µmol/mL×0.07 mL=0.021 µmol=21 nmol
4. Therefore, against the background of a normal interstitial lactate content, one minute of lactate generation from Absorb is 84 times (=21 nmol/0.25 nmol/min) less than lactate normally found in a 28-mm vessel.
5. Regarding myocardial ischemia inducing tissue hypoxia, which can increase endogenous lactic acid,8 the amount of lactic acid from a Absorb BVS is a relatively small amount that does not induce acidosis.
As discussed above, although clinical trials have exhibited a higher incidence of thrombosis with Absorb than with Xience DES, this is unlikely because of hypersensitivity reactions to the Absorb components or acidosis during degradation of the Absorb BVS. The Food & Drug Administration warnings labeled on the Absorb GT1 BVS system include clauses that Absorb BVS is contraindicated for use in patients with hypersensitivity to any component of Absorb BVS.9 However this is the practice that is applied to all other FDA-approved DES products, not only to the specific label for Absorb BVS. We still argue that the thicker and wider struts, under-expansion caused by the recoil property, and scaffold malapposition are that factors that contribute to the protrusion of the dismantled scaffold fragments into the vascular lumen in the resolution phase, leading to scaffold thrombosis.