2019 年 83 巻 12 号 p. 2479-2486
2019 年 83 巻 12 号 p. 2479-2486
Background: This study examined the association between prehospital supraglottic airway (SGA) and/or epinephrine compared with bag-mask ventilation (BMV) and Glasgow–Pittsburgh cerebral performance category (CPC) 1 status in patients with out-of-hospital cardiac arrest (OHCA) using a large, nationwide, population-based registry dataset.
Methods and Results: This was a post hoc analysis of the All-Japan Utstein Registry. We included patients with OHCA of cardiac origin aged ≥18 years with resuscitation performed by emergency medical services (EMS) between January 2011 and December 2015. The primary endpoint was favorable neurological outcome (CPC 1). The patients were divided into 4 groups according to the prehospital management performed by EMS: BMV group received only basic life support (BLS); epinephrine group received BLS plus epinephrine; SGA group received BLS plus SGA; and combined group received BLS plus epinephrine and SGA. Univariate and multivariable logistic regression analyses were performed for the primary endpoint. Among the 106,434 patients with OHCA, 48,847 received only BMV, 8,958 received BLS+epinephrine, 25,467 received BLS+SGA, and 15,551 received BLS+epinephrine+SGA. Using the BMV group as the reference, multivariable analysis showed that the epinephrine, SGA, and combined groups were independently associated with a reduced incidence of favorable neurological outcomes.
Conclusions: Our results indicated that compared with BLS, patients in the prehospital SGA and/or epinephrine groups had a significantly reduced incidence of CPC 1 status.
Prehospital management by emergency medical services (EMS) is the bridge between basic life support (BLS) at the scene and advanced hospital care in patients with out-of-hospital cardiac arrest (OHCA), and is a fundamental link in the chain of survival.1,2 An association between advanced airway management (AAM), consisting of the establishment of a supraglottic airway (SGA) and endotracheal intubation (EIT),3,4 and unfavorable neurological outcomes in patients with OHCA has been reported: 3 separate randomized control trials (RCTs) did not show a benefit of prehospital EIT compared with bag-mask ventilation (BMV) or SGA.5–7 Recently, Izawa et al reported that AAM was associated with better survival among patients with OHCA with non-shockable rhythms using the time-dependent propensity score sequential.8 However, the association between prehospital SGA (compared with BMV) and neurological outcomes in patients with OHCA has not been fully examined.
Favorable neurological outcome is commonly defined as a Glasgow–Pittsburgh cerebral performance category (CPC) 1 (good performance) or 2 (moderate disability),3,9–12 and is often used as the primary outcome in OHCA studies. The other CPC categories are 3 (severe cerebral disability), 4 (vegetative state), and 5 (death). Although patients with CPC 1 or 2 are clearly different in their functional status, researchers have usually combined these 2 categories into 1 as an indicator of favorable neurological outcomes, because of study population limitations. Therefore, no studies have examined the effect of prehospital management, such as epinephrine and/or AAM, specifically in patients classified as CPC 1.3,13–15
Thus, the purpose of this study was to comprehensively examine the association between prehospital SGA and/or epinephrine (compared with BMV) and CPC 1 status in patients with OHCA using a large, nationwide, population-based registry dataset.
The All-Japan Utstein Registry, a prospective and nationwide population-based registry of OHCA, was established on January 1, 2005, by the Fire and Disaster Management Agency (FDMA) following ethics guidelines in Japan. The registry uses Utstein-style data collection methods. All fire stations with dispatch centers and all collaborating medical institutions participate in the registry. All data are transferred and stored in the nationwide database developed by the FDMA for public use. A subcommittee of the resuscitation science study operated by the Japanese Circulation Society (JCS-ReSS) was provided with registry data,16,17 and data cleansing was performed. We therefore conducted our post hoc analysis using this cleaned database.
We included patients with OHCA of cardiac origin, aged ≥18 years, who underwent resuscitation by the EMS and had a bystander witness between January 2011 and December 2015. We excluded patients with OHCA and lost data or with conflicting records of epinephrine use and intravenous access, patients whose elapsed time from witness or call to EMS arrival was >60 min, patients whose elapsed time from witness or call to EMS to cardiopulmonary resuscitation (CPR) by the EMS was >60 min, patients whose elapsed time from witness or call to hospital arrival was >120 min, and patients who underwent EIT.
Data CollectionThe main items included in the dataset were age, sex, bystander witness status, time course of resuscitation, initial cardiac rhythm, dispatcher instructions, presence of emergency lifesaving technician or a physician in the ambulance, use of public-access automated external defibrillator (AED) by bystander, type of CPR performed by bystander, year of cardiac arrest, type of prehospital management performed by the EMS, prehospital return of spontaneous circulation (ROSC), 1-month survival, and neurological status 1 month after cardiac arrest. In this dataset, SGA included laryngeal mask airway and esophageal–tracheal twin-lumen airway.
Primary EndpointThe primary endpoint was a favorable neurological outcome, defined as CPC 1.
Statistical AnalysisThe patients were divided into 4 groups according to the type of prehospital management performed by the EMS: the BMV group received only BLS; the epinephrine group received BLS plus epinephrine; the SGA group received BLS plus SGA; and the combined group received BLS plus both epinephrine and SGA.
We compared the baseline characteristics and EMS records using the χ2 test for categorical variables and the Kruskal–Wallis H test for continuous variables. Univariate and multivariable logistic regression analyses were performed for the primary endpoint. The multivariable analysis was adjusted for potential confounders (age, sex, bystander witness status, time from witness to hospital arrival, initial cardiac rhythm, presence of physician in ambulance, dispatcher instruction, use of public-access AED by a bystander, type of CPR by a bystander, and presence of prehospital ROSC). We additionally conducted 2 subgroup analyses to control for the effects of time from EMS arrival to hospital arrival and initial cardiac rhythm on the incidence of favorable neurological outcomes. Patients were stratified across 4 categories according to the quartile of time from EMS arrival to hospital arrival (0–19, 20–24, 25–31, and 32–116 min). We then examined the association between the type of prehospital management by the EMS and the incidence of favorable neurological outcomes. We also stratified patients into 2 categories according to the initial cardiac rhythm (shockable or non-shockable) and examined the association between the type of prehospital management by the EMS and favorable neurological outcomes. We then performed 2 multivariable analyses for the primary endpoint, including the confounding factors mentioned above. Furthermore, multivariable analyses were performed for the primary endpoint in patients without prehospital ROSC. All statistical analyses were performed using JMP Pro (version 13; SAS Institute INS., Cary, NC, USA). All tests were two-sided, and P<0.05 was considered statistically significant.
A total of 629,471 patients with OHCA were enrolled in the JCS-ReSS database between January 1, 2011, and December 31, 2015. Of these, 98,823 patients with OHCA were included in the analysis, among which 48,847 (49.4%) received only BLS (BVM group), 8,958 (9.1%) received BLS+epinephrine, 25,467 (25.8%) received BLS+SGA, and 15,551 (15.7%) received BLS+epinephrine+SGA (Figure).
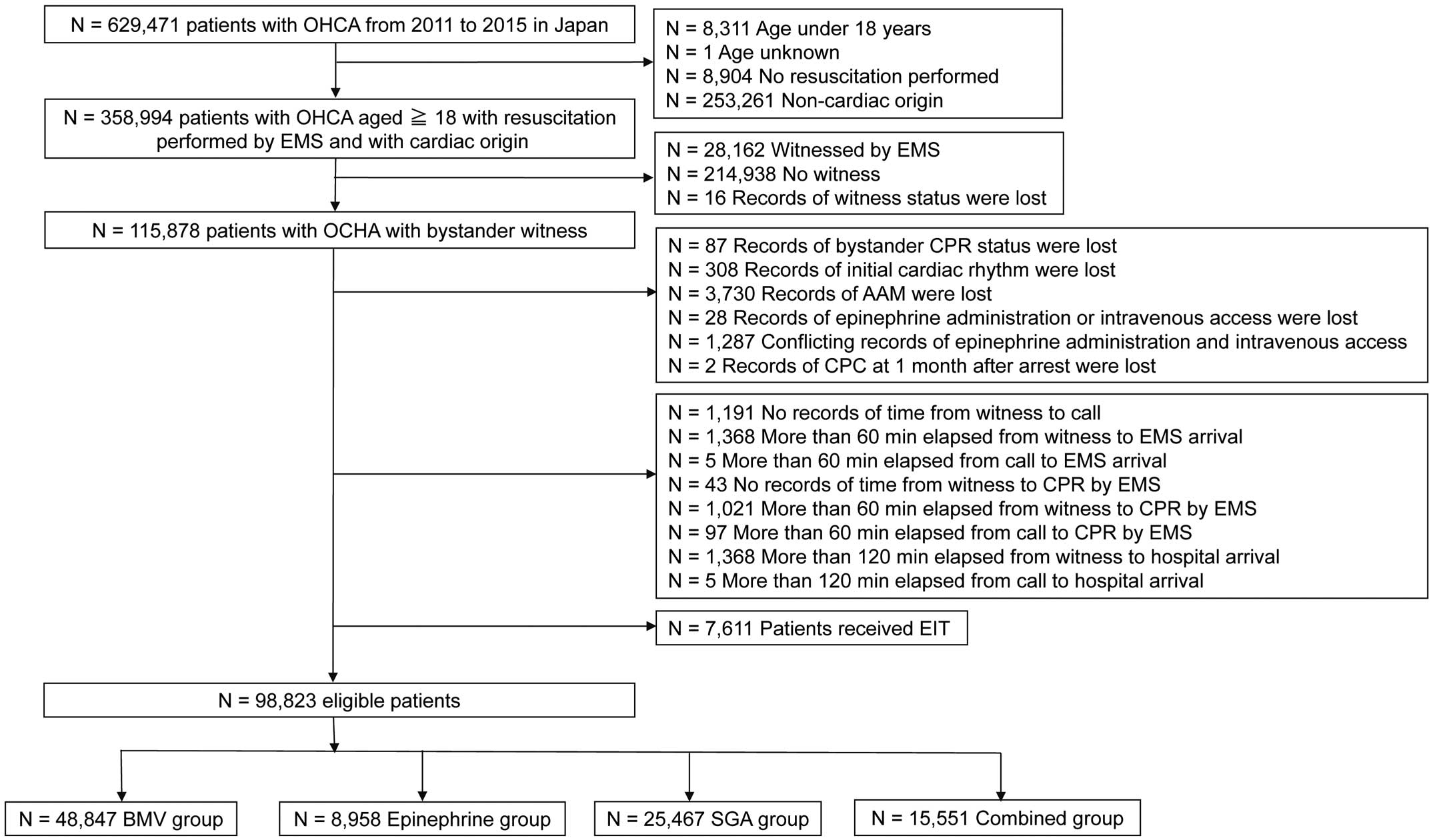
Study participant selection. BMV group received only BLS, epinephrine group received BLS+epinephrine administration, SGA group received BLS+SGA, and the combined group received BLS+epinephrine administration+SGA. AAM, advanced airway management; BLS, basic life support; BMV, bag-mask ventilation; CPC, cerebral performance category; CPR, cardiopulmonary resuscitation; EIT, endotracheal intubation; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation; SGA, supraglottic airway.
Overall, 5.4% (5,320 of 98,823) of patients were classified as CPC 1. We compared the patients’ baseline characteristics and EMS records across the 4 groups, divided by the type of prehospital management performed by the EMS. At baseline, there were significant differences among the 4 groups for all the listed variables. The frequency of CPC 1 was 8.30% (4,056 of 48,847) in the BMV group, 2.98% (267 of 8,958) in the epinephrine group, 2.91% (742 of 25,467) in the SGA group, and 1.64% (255 of 15,551) in the combined group (Table 1).
| Total (n=98,823) |
BMV group (n=48,847) |
Epinephrine group (n=8,958) |
SGA group (n=25,467) |
Combined group (n=15,551) |
P value | |
|---|---|---|---|---|---|---|
| Age, years, mean (SD) | 75.6 (14.7) | 76.3 (15.1) | 73.8 (14.6) | 75.6 (14.2) | 74.6 (14.2) | <0.001 |
| Male, n (%) | 60,384 (61.1) | 28,525 (58.4) | 6,039 (67.4) | 15,499 (60.9) | 10,321 (66.4) | <0.001 |
| Bystander witness status | <0.001 | |||||
| Family member, n (%) | 62,849 (63.6) | 29,026 (59.4) | 5,999 (66.9) | 17,178 (67.5) | 10,646 (68.5) | |
| Friend, n (%) | 3,900 (3.94) | 1,812 (3.71) | 453 (5.06) | 898 (3.53) | 737 (4.74) | |
| Colleague, n (%) | 3,713 (3.76) | 1,820 (3.73) | 460 (5.14) | 813 (3.19) | 620 (3.99) | |
| Passerby, n (%) | 3,942 (4.00) | 1,984 (4.06) | 465 (5.19) | 872 (3.42) | 621 (3.99) | |
| Other, n (%) | 24,419 (24.7) | 14,205 (29.1) | 1,581 (17.7) | 5,706 (22.4) | 2,927 (18.8) | |
| Time from witness to call, min, mean (SD) |
2.93 (6.83) | 3.21 (7.23) | 2.33 (5.88) | 2.84 (6.77) | 2.55 (6.07) | <0.001 |
| Time from witness to EMS arrival, min, mean (SD) |
10.7 (7.47) | 10.8 (7.79) | 10.2 (6.68) | 10.7 (7.42) | 10.7 (6.88) | <0.001 |
| Time from witness to CPR by EMS, min, mean (SD) |
12.3 (7.65) | 12.4 (8.00) | 11.8 (6.82) | 12.3 (7.57) | 12.3 (7.05) | <0.001 |
| Time from witness to hospital arrival, min, mean (SD) |
36.9 (13.9) | 35.1 (14.1) | 39.7 (13.1) | 37.0 (13.2) | 41.1 (13.5) | <0.001 |
| Time from call to EMS arrival, min, mean (SD) |
7.76 (3.42) | 7.57 (3.33) | 7.92 (3.47) | 7.84 (3.39) | 8.13 (3.65) | <0.001 |
| Time from call to CPR by the EMS, min, mean (SD) |
9.35 (3.73) | 9.18 (3.71) | 9.47 (3.63) | 9.44 (3.68) | 9.70 (3.88) | <0.001 |
| Time from call to hospital arrival, min, mean (SD) |
34.0 (12.2) | 31.8 (12.2) | 37.4 (11.8) | 34.1 (11.3) | 39.6 (12.1) | <0.001 |
| Time from EMS arrival to hospital arrival, min, mean (SD) |
26.2 (11.2) | 24.3 (11.3) | 29.4 (10.9) | 26.3 (10.1) | 30.4 (10.8) | <0.001 |
| Shockable initial cardiac rhythm, n (%) |
21,067 (21.3) | 10,647 (21.8) | 2,338 (26.1) | 4,693 (18.4) | 3,389 (21.8) | <0.001 |
| Dispatcher instruction, n (%) | 48,561 (49.1) | 22,373 (45.8) | 4,530 (50.6) | 13,075 (51.3) | 8,583 (55.2) | <0.001 |
| Presence of certified ELSTs in ambulance, n (%) |
96,423 (97.6) | 46,871 (96.0) | 8,837 (98.7) | 25,289 (99.3) | 15,426 (99.2) | <0.001 |
| Presence of physician in ambulance, n (%) |
3,710 (3.73) | 1,972 (4.04) | 340 (3.80) | 837 (3.29) | 561 (3.61) | <0.001 |
| Use of public-access AED by citizen, n (%) |
2,812 (2.84) | 1,688 (3.46) | 259 (2.89) | 494 (1.94) | 371 (2.39) | <0.001 |
| Prehospital ROSC, n (%) | 15,011 (15.2) | 7,855 (16.1) | 1,888 (21.1) | 2,090 (8.21) | 3,178 (20.4) | <0.001 |
| Type of CPR performed by bystander |
<0.001 | |||||
| Chest-compression-only CPR, n (%) |
41,700 (42.2) | 20,535 (42.0) | 3,717 (41.5) | 10,745 (42.2) | 6,703 (43.1) | |
| Conventional CPR, n (%) | 9,076 (9.18) | 4,957 (10.2) | 670 (7.48) | 2,193 (8.61) | 1,256 (8.08) | |
| Breathing only, n (%) | 377 (0.38) | 219 (0.45) | 31 (0.35) | 81 (0.32) | 46 (0.45) | |
| No CPR, n (%) | 47,670 (48.2) | 23,136 (47.4) | 4,540 (50.7) | 12,448 (48.9) | 7,546 (48.5) | |
| Year of cardiac arrest, n (%) | <0.001 | |||||
| 2011 | 19,845 (20.1) | 9,836 (20.1) | 1,582 (17.7) | 5,711 (22.4) | 2,716 (17.5) | |
| 2012 | 20,223 (20.5) | 10,256 (21.0) | 1,708 (19.1) | 5,326 (21.0) | 2,933 (18.9) | |
| 2013 | 20,748 (21.0) | 10,555 (21.6) | 1,915 (21.4) | 5,110 (20.1) | 3,168 (20.4) | |
| 2014 | 21,137 (21.4) | 10,899 (22.3) | 2,093 (23.4) | 4,768 (18.7) | 3,377 (21.7) | |
| 2015 | 16,870 (17.1) | 7,301 (15.0) | 1,660 (18.5) | 4,552 (17.9) | 3,357 (21.6) | |
| 1-month survival, n (%) | 10,422 (10.5) | 6,704 (13.7) | 722 (8.06) | 1,898 (7.45) | 1,098 (7.06) | <0.001 |
| Neurological status at 1 month after cardiac arrest |
<0.001 | |||||
| CPC 1, n (%) | 5,320 (5.38) | 4,056 (8.30) | 267 (2.98) | 742 (2.91) | 255 (1.64) | |
| CPC 2, n (%) | 1,105 (1.12) | 729 (1.49) | 66 (0.74) | 195 (0.77) | 115 (0.74) | |
| CPC 3, n (%) | 1,376 (1.39) | 778 (1.59) | 121 (1.35) | 307 (1.21) | 170 (1.09) | |
| CPC 4, n (%) | 2,367 (2.40) | 1,030 (2.11) | 233 (2.59) | 600 (2.36) | 505 (3.25) | |
| CPC 5, n (%) | 88,655 (89.7) | 42,254 (86.5) | 8,272 (92.3) | 23,623 (92.8) | 14,506 (93.3) |
Data are expressed as number (%) of patients, or as mean (SD) of EMS records. Continuous variables were compared using the Kruskal-Wallis rank test. Categorical variables were compared using the χ2 test. BMV group received only BLS, epinephrine group received BLS+epinephrine, SGA group received BLS+SGA, and combined group received BLS+epinephrine+SGA. AED, automated external defibrillator; BLS, basic life support; BMV, bag-mask ventilation; CPC, cerebral performance category; CPR, cardiopulmonary resuscitation; ELST, emergency lifesaving technician; EMS, emergency medical service; ROSC, return of spontaneous circulation; SGA, supraglottic airway.
Multivariable analysis was performed to examine the association between the type of prehospital management and favorable neurological outcome. Using the BMV group as the reference, the epinephrine (adjusted odds ratio (OR), 0.28; 95% confidence interval (CI), 0.24–0.32), SGA (adjusted OR, 0.52; 95% CI, 0.47–0.58), and combined groups (adjusted OR, 0.17; 95% CI, 0.15–0.20) were independently associated with a reduced incidence of favorable neurological outcome. The other factors that were independently associated with reduced incidence of a favorable neurological outcome were older age, prolonged time from witness to hospital arrival, and no bystander CPR. The factors that were independently associated with improved favorable neurological outcome were male sex, witness by a friend, witness by a colleague, shockable initial cardiac rhythm, use of public-access AED by a bystander, and presence of prehospital ROSC (Table 2).
| Adjusted OR (95% CI) |
P value | |
|---|---|---|
| Age | 0.96 (0.96–0.96) | <0.001 |
| Male | 1.10 (1.01–1.21) | 0.03 |
| Bystander witness status | ||
| Family member | Ref. | |
| Friend | 1.45 (1.25–1.67) | <0.001 |
| Colleague | 1.17 (1.02–1.33) | 0.02 |
| Passerby | 1.11 (0.97–1.28) | 0.14 |
| Other | 0.92 (0.84–1.02) | 0.13 |
| Time from witness to hospital arrival | 0.98 (0.98–0.99) | <0.001 |
| Shockable initial cardiac rhythm | 4.74 (4.36–5.14) | <0.001 |
| Presence of physician in ambulance | 1.07 (0.93–1.23) | 0.37 |
| Dispatcher instruction | 0.95 (0.87–1.03) | 0.21 |
| Use of public-access AED by citizen | 1.50 (1.30–1.73) | <0.001 |
| Type of CPR performed by bystander | ||
| Conventional CPR | Ref. | |
| Chest-compression-only CPR | 0.95 (0.84–1.07) | 0.42 |
| Breathing only | 0.80 (0.44–1.43) | 0.45 |
| No CPR | 0.68 (0.60–0.77) | <0.001 |
| Prehospital ROSC | 27.2 (25.0–29.6) | <0.001 |
| Type of prehospital management performed by the EMS | ||
| BMV | Ref. | |
| BLS+epinephrine | 0.28 (0.24–0.32) | <0.001 |
| BLS+SGA | 0.52 (0.47–0.58) | <0.001 |
| Combined (BLS+epinephrine+SGA) | 0.17 (0.15–0.20) | <0.001 |
CI, confidence interval; OR, odds ratio. Other abbreviations as in Table 1.
We stratified the 4 categories according to the time from EMS arrival to hospital arrival (by quartiles: 0–19, 20–24, 25–31, 32–116 min). Using the BMV group as the reference, for patients with EMS arrival to hospital arrival time of 1–19 min, the epinephrine (adjusted OR, 0.53; 95% CI, 0.38–0.74), SGA (adjusted OR, 0.58; 95% CI, 0.48–0.69), and combined groups (adjusted OR, 0.32; 95% CI, 0.22–0.45) exhibited reduced favorable neurological outcomes. Similar results were obtained for all other EMS arrival to hospital arrival groupings (Table 3).
| 0–19 min (n=27,667) | 20–24 min (n=22,754) | 25–31 min (n=28,713) | 32–116 min (n=26,848) | |||||
|---|---|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) |
P value | Adjusted OR (95% CI) |
P value | Adjusted OR (95% CI) |
P value | Adjusted OR (95% CI) |
P value | |
| Age | 0.96 (0.96–0.97) |
<0.001 | 0.96 (0.96–0.97) |
<0.001 | 0.96 (0.96–0.97) |
<0.001 | 0.96 (0.96–0.97) |
<0.001 |
| Male | 1.25 (1.07–1.46) |
0.005 | 1.05 (0.87–1.25) |
0.62 | 1.10 (0.93–1.31) |
0.27 | 0.97 (0.81–1.16) |
0.73 |
| Bystander witness status | ||||||||
| Family member | Ref. | Ref. | Ref. | Ref. | ||||
| Friend | 1.35 (1.06–1.72) |
0.01 | 1.22 (0.91–1.63) |
0.18 | 1.50 (1.13–2.00) |
0.006 | 1.66 (1.22–2.27) |
0.001 |
| Colleague | 1.24 (0.99–1.55) |
0.06 | 1.06 (0.81–1.40) |
0.65 | 1.04 (0.80–1.35) |
0.76 | 1.03 (0.77–1.38) |
0.85 |
| Passerby | 1.24 (1.00–1.53) |
0.05 | 0.88 (0.65–1.18) |
0.40 | 0.86 (0.63–1.16) |
0.32 | 0.80 (0.56–1.13) |
0.20 |
| Other | 0.93 (0.79–1.10) |
0.40 | 0.88 (0.71–1.09) |
0.23 | 0.80 (0.65–0.99) |
0.04 | 0.86 (0.70–1.07) |
0.19 |
| Time from witness to hospital arrival |
0.95 (0.94–0.96) |
<0.001 | 0.96 (0.94–0.97) |
<0.001 | 0.94 (0.93–0.96) |
<0.001 | 1.00 (0.99–1.01) |
0.93 |
| Shockable initial cardiac rhythm |
5.15 (4.46–5.95) |
<0.001 | 4.28 (3.61–5.09) |
<0.001 | 4.14 (3.52–4.87) |
<0.001 | 4.77 (4.02–5.65) |
<0.001 |
| Presence of physician in ambulance |
1.14 (0.82–1.59) |
0.43 | 1.29 (0.94–1.75) |
0.11 | 1.20 (0.92–1.56) |
0.19 | 0.84 (0.67–1.05) |
0.14 |
| Dispatcher instruction | 0.97 (0.84–1.11) |
0.63 | 0.97 (0.82–1.15) |
0.73 | 1.01 (0.86–1.19) |
0.90 | 0.89 (0.75–1.06) |
0.19 |
| Use of public-access AED by citizen |
1.80 (1.41–2.29) |
<0.001 | 1.32 (0.97–1.79) |
0.08 | 1.98 (1.50–2.60) |
<0.001 | 1.16 (0.86–1.56) |
0.34 |
| Type of CPR performed by bystander | ||||||||
| Conventional CPR | Ref. | Ref. | Ref. | Ref. | ||||
| Chest-compression-only CPR |
0.90 (0.73–1.11) |
0.34 | 0.98 (0.76–1.25) |
0.84 | 0.95 (0.75–1.20) |
0.66 | 0.97 (0.75–1.25) |
0.82 |
| Breathing only | 0.66 (0.20–2.20) |
0.50 | 0.52 (0.14–1.88) |
0.32 | 1.02 (0.39–2.67) |
0.97 | 0.94 (0.26–3.38) |
0.93 |
| No CPR | 0.64 (0.51–0.81) |
0.0001 | 0.76 (0.58–0.99) |
0.047 | 0.66 (0.51–0.86) |
0.002 | 0.62 (0.47–0.82) |
0.0007 |
| Prehospital ROSC | 23.1 (20.2–26.4) |
<0.001 | 27.5 (23.1–32.8) |
<0.001 | 29.5 (24.6–35.3) |
<0.001 | 39.3 (31.7–48.8) |
<0.001 |
| Type of prehospital management performed by the EMS | ||||||||
| BMV | Ref. | Ref. | Ref. | Ref. | ||||
| BLS+epinephrine | 0.53 (0.38–0.74) |
0.0002 | 0.37 (0.28–0.49) |
<0.001 | 0.24 (0.18–0.31) |
<0.001 | 0.21 (0.16–0.27) |
<0.001 |
| BLS+SGA | 0.58 (0.48–0.69) |
<0.001 | 0.58 (0.48–0.70) |
<0.001 | 0.51 (0.43–0.62) |
<0.001 | 0.45 (0.37–0.56) |
<0.001 |
| Combined (BLS+epinephrine+SGA) |
0.32 (0.22–0.45) |
<0.001 | 0.19 (0.14–0.25) |
<0.001 | 0.18 (0.14–0.24) |
<0.001 | 0.13 (0.10–0.17) |
<0.001 |
Abbreviations as in Tables 1,2.
Association Between the Type of Prehospital Management Performed by the EMS and Favorable Neurological Outcomes Across 2 Categories Stratified by the Initial Cardiac Rhythm We stratified patients according to the initial cardiac rhythm (shockable and non-shockable). Compared with the BMV group as the reference, shockable patients in the epinephrine group (adjusted OR, 0.35; 95% CI, 0.30–0.42), SGA group (adjusted OR, 0.57; 95% CI, 0.50–0.63), and the combined group (adjusted OR, 0.21; 95% CI, 0.18–0.24) had reduced favorable neurological outcomes. Similarly, among non-shockable patients, those in the epinephrine (adjusted OR, 0.11; 95% CI, 0.08–0.16), SGA (adjusted OR, 0.44; 95% CI, 0.36–0.54), and combined groups (adjusted OR, 0.10; 95% CI, 0.07–0.13) had reduced favorable neurological outcomes (Table 4).
| Shockable (n=21,067) | Non-shockable (n=77,756) | |||
|---|---|---|---|---|
| Adjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P value | |
| Age | 0.96 (0.96–0.97) | <0.001 | 0.97 (0.96–0.97) | <0.001 |
| Male | 1.03 (0.93–1.15) | 0.55 | 1.13 (0.98–1.31) | 0.1 |
| Bystander witness status | ||||
| Family member | Ref. | Ref. | ||
| Friend | 1.34 (1.15–1.57) | 0.0002 | 1.78 (1.32–2.40) | 0.0002 |
| Colleague | 1.18 (1.02–1.36) | 0.02 | 1.10 (0.79–1.54) | 0.58 |
| Passerby | 0.99 (0.85–1.16) | 0.92 | 1.76 (1.35–2.30) | <0.001 |
| Other | 1.00 (0.88–1.13) | 0.99 | 0.89 (0.75–1.07) | 0.22 |
| Time from witness to hospital arrival | 0.98 (0.98–0.99) | <0.001 | 0.98 (0.97–0.99) | <0.001 |
| Presence of physician in ambulance | 1.22 (1.03–1.44) | 0.02 | 0.70 (0.53–0.92) | 0.01 |
| Dispatcher instruction | 1.00 (0.91–1.11) | 0.94 | 0.85 (0.73–0.99) | 0.04 |
| Use of public-access AED by citizen | 1.27 (1.08–1.48) | 0.003 | 2.28 (1.71–3.03) | <0.001 |
| Type of CPR performed by bystander | ||||
| Conventional CPR | Ref. | Ref. | ||
| Chest-compression-only CPR | 0.90 (0.78–1.04) | 0.14 | 1.08 (0.85–1.38) | 0.52 |
| Breathing only | 0.91 (0.46–1.81) | 0.79 | 0.56 (0.16–1.97) | 0.37 |
| No CPR | 0.56 (0.48–0.65) | <0.001 | 1.07 (0.83–1.38) | 0.62 |
| Prehospital ROSC | 17.8 (16.2–19.7) | <0.001 | 73.1 (61.4–86.9) | <0.001 |
| Type of prehospital management performed by the EMS | ||||
| BMV | Ref. | Ref. | ||
| BLS+epinephrine | 0.35 (0.30–0.42) | <0.001 | 0.11 (0.08–0.16) | <0.001 |
| BLS+SGA | 0.57 (0.50–0.63) | <0.001 | 0.44 (0.36–0.54) | <0.001 |
| Combined (BLS+epinephrine+SGA) | 0.21 (0.18–0.24) | <0.001 | 0.10 (0.7–0.13) | <0.001 |
Abbreviations as in Tables 1,2.
Association Between the Type of Prehospital Management Performed by the EMS and Favorable Neurological Outcomes in Patients Without Prehospital ROSC Using the BMV group as the reference, the SGA (adjusted OR, 0.65; 95% CI, 0.54–0.78), and combined (adjusted OR, 0.60; 95% CI, 0.48–0.76) groups had reduced favorable neurological outcomes (Supplementary Table 1).
In the present study, prehospital SGA and/or epinephrine (compared with BMV) were significantly associated with reduced incidence of Glasgow–Pittsburgh CPC 1 in patients who sustained an OHCA. There were persistent, significant associations between prehospital SGA and/or epinephrine (compared with BMV) and unfavorable outcomes, even when patients were further divided relative to time from EMS arrival to hospital arrival (0–19, 20–24, 25–32, and 32–116 min), or if the initial cardiac rhythm was shockable or non-shockable.
No observational studies or RCTs have evaluated the association between prehospital epinephrine use and SGA (compared with BMV) exclusively in CPC 1 patients who experienced OHCA. According to the subgroup analysis conducted by Izawa et al, SGA (compared with BMV) was associated with unfavorable neurological outcomes [0.89 (0.81 to 0.99)] in shockable patients with OHCA; however, those authors defined CPC 1–2 as a favorable neurological outcome.8 In our study, SGA (compared with BMV) was associated with unfavorable neurological outcomes in patients with OHCA both shockable and non-shockable.
The reason why prehospital SGA (compared with BMV) was significantly associated with reduced incidence of CPC 1 in patients with OHCA is unclear. Considering the small number of CPC 2 patients included in the current study (only 6.19% of the CPC 1 and 2 patients were CPC 2), our results were similar to those of previously reported studies in which AAM was significantly associated with reduced incidence of favorable neurological outcomes, defined as CPC 1 and 2.3,4 Moreover, because very few patients underwent EIT (only 15.7%), SGA consisted of 85.3% AAM. Thus, our results resembled those of previous studies. From a theoretical point of view, delayed hospital admission because of the initiation of SGA may play a role in the preponderance of undesirable outcomes. However, we observed similar results even among patients who experienced a relatively quick (<20 min) transition from EMS arrival to hospital admission. Patients who received SGA might have had unevaluated factors for primary brain damage compared with BMV.
Izawa et al reported that earlier prehospital AAM by EMS personnel (within 4 min from CPR to AAM) was associated with functionally better survival among adult patients who received AAM;14 therefore, only patients in whom prompt establishment of a SGA is possible should be candidates for SGA by EMS personnel.
Although only 8,138 of 98,823 patients had records of the time of SGA establishment, we observed that the break point of the timing to SGA was within 5 min from CPR by the EMS (Supplementary Table 2), which was similar to the report by Izawa et al.
Otherwise, direct transfer to the hospital may produce better outcomes within the context of current clinical practice guidelines. With the development of cutting-edge devices, drugs, and/or systems, these concepts will require reconsideration.
Study LimitationsThere are several to note. First, detailed information pertaining to times (epinephrine use, AAM, and/or intravenous access) were not examined because of data unavailability. Second, the details of chest compression quality, including chest compression depth, rate, and fraction (which are closely associated neurological outcomes), were not evaluated because of data unavailability.18–22 Third, the details of hospital treatment were not examined because of data unavailability. Lastly, 17,057 patients (14.7%) were excluded. Favorable outcomes were noted in 5.38% of the analyzed data, and in 4.21% of the excluded data; thus, favorable outcomes may have been overestimated in the current study.
Prehospital SGA and/or epinephrine, compared with BVM, significantly reduced the incidence of CPC 1 status in patients with OHCA.
We thank all the EMS personnel and physicians concerned in Japan and the staff of the Fire and Disaster Management Agency and Institute for Fire Safety and Disaster Preparedness of Japan for their generous cooperation in establishing and following the Utstein database. We also thank Takashi Amano and Kanako Kojima for their administrative assistance to the Subcommittee of Resuscitation Science of the Japanese Circulation Society.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-19-0553