With the rapid aging of the population in Japan, approximately 1 million people are affected by heart failure (HF).1
Renin-angiotensin-aldosterone (RAA) system inhibitors and β-blockers, which have come to be widely used for treating HF, drastically improving the patient’s long-term prognosis.2
Several patients experience exacerbation of HF despite the use of such effective pharmacotherapies.3
In the future, it is expected that the number of patients with HF will increase,4
as will the associated medical expenses. Therefore, improving the long-term prognosis and reducing the number of hospital admissions for exacerbation of HF are presently urgent issues that need to be addressed as goals for the field of HF treatment.
In the 1970 s, cardiac rehabilitation came into practice with the aim of addressing early ambulation, and social rehabilitation in patients following acute myocardial infarction (AMI). Thereafter, satisfactory evidence was established indicating that rehabilitation performed comprehensively with exercise training, patient education, and counseling for patients following AMI improves exercise tolerability and is useful for secondary prevention.5,6
Such programs also proved effective for patients treated for coronary artery disease in general,7
including coronary intervention,8,9
and coronary bypass surgery.10
Cardiac rehabilitation for HF effectively progresses exercise tolerability, reduces the rate of rehospitalization, and improves long-term prognosis by suppressing neurohumoral factors and inflammatory cytokines, and improving vascular endothelium function and musculoskeletal metabolism through exercise training.11–16
Cardiac rehabilitation with such multifaceted effects is becoming increasingly perceived as advanced medical care. At the same time, its usefulness as a disease management program implemented by a multidisciplinary team has been recognized.17,18
In Japan, however, efforts are poured into treatment for acute HF to stabilize hemodynamics. Yet, once hemodynamics are stable, the implementation of systematic patient education, lifestyle guidance, and exercise training as part of a necessary disease management program remains inadequate. Furthermore, after hospital discharge, numerous patients are referred back to their general practitioner. Therefore, after discharge, few patients continue cardiac rehabilitation, including exercise training commenced during their hospital stay, and the rate of outpatient cardiac rehabilitation implementation is very low.19
To function as a HF management program, the popularization of an outpatient cardiac rehabilitation program after hospital discharge is a major challenge. “Guidelines for Rehabilitation in Patients with Cardiovascular Disease (JCS2012)”20
have been established in Japan. Although this guideline presents the essential policy and implementation summary, there is no mention of specific procedures in actual clinical settings. The Japanese Association of Cardiac Rehabilitation (JACR) has indicated that a standard program needs to be prepared for utilization in clinical settings to promote appropriate cardiac rehabilitation implementation. Therefore, the JACR released a “Standard rehabilitation program from acute-to-recovery phase myocardial infarction” in 2014.
“Standard Heart Failure Program”
Target Outcomes
With the aim of implementing and popularizing appropriate cardiac rehabilitation for HF, we (Japanese Association of Cardiac Rehabilitation with the approval of the Japanese Circulation Society and the Japanese Heart Failure Society) created a standard, comprehensive cardiac rehabilitation program primarily for patients with HF who are able to tolerate exercise training and were previously independent with their activities of daily living (ADLs) prior to hospital admission. The target outcomes of this “Standard Heart Failure Program” are: (1) improve prognosis, (2) prevent rehospitalization, and (3) prevent physical dysfunction. To attain these outcomes, this cardiac rehabilitation program for HF needs to be accessible to all. The standard program includes essential elements, which we would like to see adopted by all institutions implementing the cardiac rehabilitation program, and desirable elements, which require the development and establishment of human resources, education, devices, and facilities at each institution to achieve the target outcomes of the standard program.
Features
This “Standard Heart Failure Program” begins with an acute-phase ambulation program, and introduces exercise training after stabilization of hemodynamics, until cardiac rehabilitation is implemented after hospital discharge while the patient is receiving outpatient treatment. The general rules are designed for implementation within regional core hospitals that provide acute-phase care; however, even at medical institutions that primarily provide chronic-phase care, these guidelines can be used as a reference when performing cardiac rehabilitation.
The content of the Standard Program is based on the “Guidelines for Rehabilitation in Patients with Cardiovascular Disease (JCS2012)”,20
which was created through collaboration of various groups, including the Japanese Circulation Society. Although evidence exists of the benefits of cardiac rehabilitation for patients with HF, there is little detailed evidence, and a substantial portion of what is available is based on the experiences and opinions of experts who have carried out rehabilitation in practical settings.
Each program activity has
essential
and
desirable
elements. This involves creating an exercise program based on the patient’s condition after stabilization of hemodynamics, and includes elements that address lifestyle and medication adherence, evaluation and management of comorbidities, disease management such as psychological counseling, medical cooperation and confirmation of medical welfare services following discharge, outpatient disease management to prevent re-admission, and specific evaluations, interventions, and goals. Lastly, the program describes frail patients, and patients with dual-chamber pacing [cardiac resynchronization therapy (CRT)], an implantable cardioverter defibrillator (ICD), or ventricular assist device (VAD), which are used by an increasing number of patients.
The Standard Program Planning Committee consists of members from various disciplines who are highly experienced in cardiac rehabilitation based on JACR recommendations. This committee designed the program to include practical content that can be readily applied in clinical practice settings in Japan. Here, we describe a standard program, guided by JACR recommendations. Following incorporation of a wide spectrum of opinions, we hope to continually revise and improve the program, moving forward.
As a disease management program, comprehensive cardiac rehabilitation is needed during hospital stay, and should also be continued after patients are discharged from the hospital and return to society. Although a consensus has been reached that intervention by a multidisciplinary team is needed for the treatment and management of patients with HF to prevent rehospitalization caused by the exacerbation of HF and to improve long-term prognosis, we hope that comprehensive cardiac rehabilitation will be implemented throughout Japan, based on the standard program within each institution.
Components of the Standard Cardiac Rehabilitation Program (see Supplementary File)
I. Acute phase
Ambulation period
1. Acute phase ambulation program⋯See Below
Preparation period for the exercise training
2. Evaluation of patient backgrounds and acute exacerbation factors⋯4
3. Evaluation of cardiac function and hemodynamics⋯7
4. Evaluation of indications and contraindications for exercise training⋯9
5. Creation of an exercise program for introduction of exercise training⋯11
II. Early recovery phase
Inpatient rehabilitation period
1. Creation of an exercise program⋯13
2. Regular evaluation and revision of the exercise program⋯16
3. Nutrition and fluid management⋯18
4. Medication management⋯20
5. Evaluation and management of systemic comorbidities (hypertension, renal dysfunction, diabetes, anemia, sleep-disordered breathing)⋯21
6. Management of psychological and social factors⋯23
Discharge preparation period
7. Evaluation of cardiac function and hemodynamics prior to discharge⋯26
8. Creation of a post-discharge exercise program⋯28
9. Guidance for activities of daily living following discharge⋯30
III. Late recovery phase (Outpatient rehabilitation period)
1. Regular evaluation and revision of the exercise program⋯31
2. Disease management focusing on acute exacerbation factors⋯33
IV. Cooperation with local medical institutions and facilities
1. Hospital-clinic coordination and local cooperation⋯35
V. Patients who require particular attention
1. Frail patients⋯37
2. Patients receiving cardiac resynchronization therapy (CRT)/ implantable cardioverter defibrillators (ICD)⋯39
3. Patients receiving a left ventricular assist device (LVAD)⋯41
VI. Basic requirements for program implementation
1. Program management system⋯44
2. System to manage emergencies and unusual situations⋯46
How to Use This Standard Program
The “Standard Cardiac Rehabilitation Program for Heart Failure” is indicated for patients with HF who were independently and adequately performing ADLs prior to hospital admission, and for whom exercise training is not contraindicated.
This program is written according to a time line in which cardiac rehabilitation is commenced following hospital admission for HF, starting from the acute-phase ambulation program, to the early recovery phase, late recovery phase, and maintenance phase (Figure 1).
Chapter I describes the acute HF path implemented as the ambulation program of the acute phase after admission. During the acute phase after admission, the ambulation program proceeds in parallel with acute-phase treatment, leading to introduction of exercise training.
When commencing exercise training in the stable disease period, the following items should be checked prior to introducing exercise training: the patient’s background, evaluation of the patient’s condition (especially acute exacerbation factors that could result in hospitalization), and contraindications for exercise training. During this period, if the patient is able to walk at least 300 m during a 6-min walking test, an exercise program is created and exercise training is commenced. Points to be adopted when introducing exercise training are also noted.
Chapter II discusses the creation of an exercise program based on the results of cardiopulmonary exercise testing (CPX), with periodic evaluations and revisions. This chapter also describes a disease management program implemented during hospitalization, in parallel with exercise training, including ADLs, medication adherence, evaluation and management of comorbidities, and psychological counseling.
Prior to continuing exercise training on an outpatient basis after discharge, cardiac function and hemodynamics should be evaluated immediately prior to discharge. Then, the exercise program can be completed upon evaluation of exercise tolerance, considering ADL needs following discharge.
Chapter III discusses re-evaluation and revision of the exercise program during hospital visits conducted during the rehabilitation period. An additional focus is disease management, particularly the management of factors related to the exacerbation of HF, in order to prevent rehospitalization.
Chapter IV discusses multidisciplinary activities and confirmation of medical welfare services following discharge, including items that are necessary when cooperating with local health promotion facilities.
Chapter V discusses the program for frail elderly patients and patients with dual-chamber pacing CRT, an ICD, or VAD, used in increasing numbers of patients.
Chapter VI discusses the provision of a management system, and a system to deal with emergencies/abnormalities as basic programmatic requirements.
All program evaluations, interventions, and target goals are divided between
essential elements
and
desirable elements, based on the criteria given below. Essential elements are the minimum-necessary requirements for cardiac rehabilitation program implementation. Desirable elements are items that we would ultimately like to be conducted by all institutions that implement cardiac rehabilitation.
We would like members of the cardiac rehabilitation team, regardless of their respective disciplines, to check the items written here, and share their status with their team. We hope to create a system of information-sharing during team meetings in order to determine who is responsible for the various items.
Explanation of the Elements
| Essential elements |
| Minimum required content of the cardiac rehabilitation program |
| Desirable elements |
| Content aimed towards developing and ultimately establishing human resources, education, devices, and facilities at each participating institution |
I. Acute Phase (Ambulation Period)
In the acute phase after admission (ambulation period), the ambulation program proceeds in parallel with acute-phase treatment, leading to the introduction of exercise training. The ambulation program is an essential element for all medical institutions that provide acute-phase care for patients with HF, and there are no desirable elements in this chapter. A typical example of the acute-phase ambulation program is given below. The program is a sample, and s created in accordance with the circumstances of each institution, such as the walking distance.
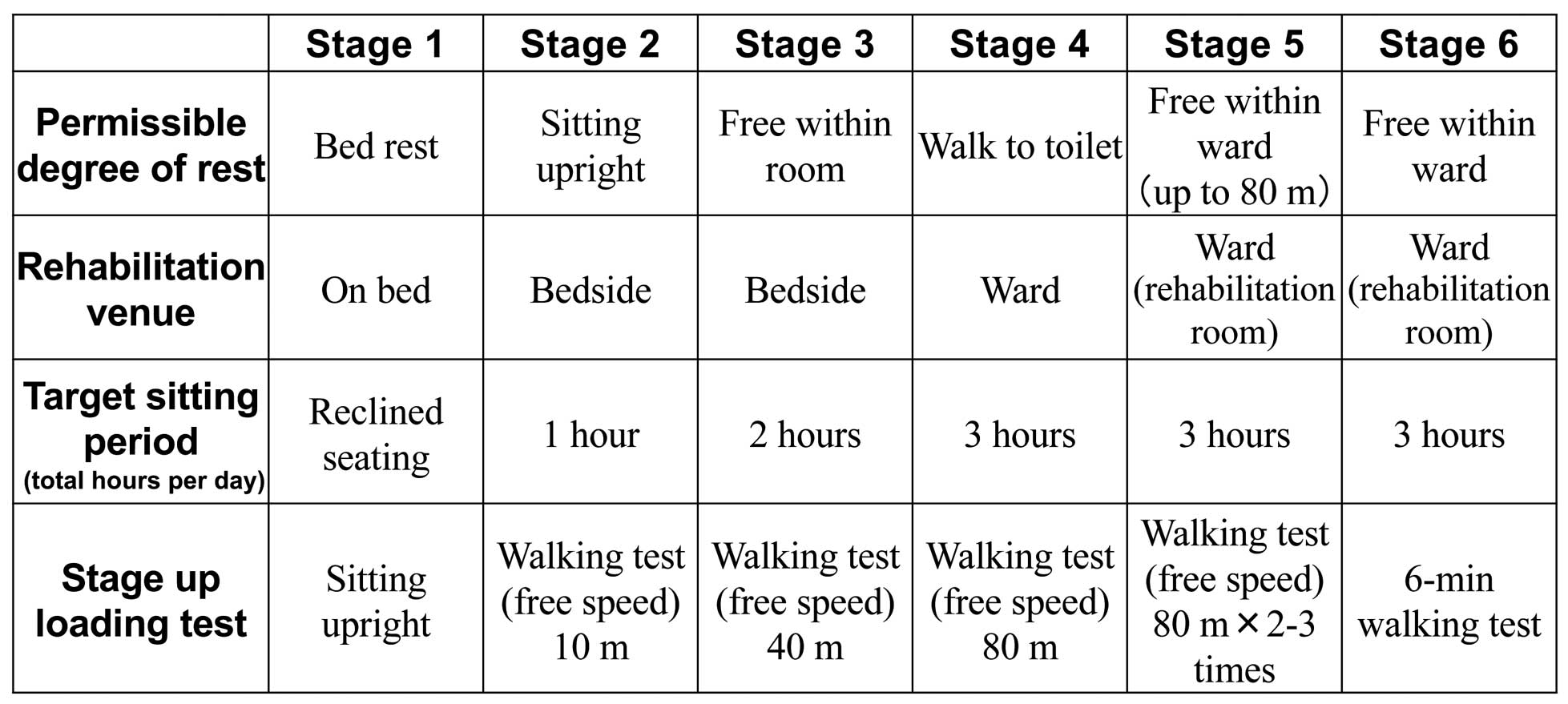
1. Acute-Phase Ambulation Program (Figure 2)
During the acute phase, immediately after hospital admission for acute HF, the focus of treatment is hemodynamic stabilization. Prolonged bed rest can reduce muscle strength and exercise tolerance; therefore, the ambulation program given below is commenced at bedside during the acute phase, ideally leading to early implementation of exercise training.
To proceed to the next stage, the patient’s hemodynamics must be stable, as demonstrated by the stage completion loading test. For example, when proceeding from stage 1 to stage 2, the degree of rest changes from bed rest to sitting upright; however, hypertension, heart rate, partial arterial pressure of oxygen, and ECG monitors must be checked while the patient is sitting upright to confirm hemodynamic stability before the patient moves on to stage 2.
In stage 2, sitting upright is permitted, and the target sitting period is 1 hour. Thereafter, and before moving up to the next stage, each stage completion loading test must be performed. Importantly, hemodynamic stability must be repeatedly confirmed. Clinicians should also confirm that severe arrhythmia does not arise from loading, and as the patient moves up to the next stage, his or her ambulation improves, and the target sitting time increases. From stage 2 onwards, patients will complete a walking test at their own pace with no specified distance or speed, to determine whether they are able to walk the target distance of each stage. In the 6-min walking test, if the patient can walk approximately 300 m, he or she completes stage 6, and proceeds onto the introduction of exercise training, as described in chapters one I to five V.
*Patients who progress smoothly through the ambulation program above, with sufficient exercise tolerance, such as younger patients and patients with milder disease, are able to skip stages while paying due care to hemodynamic stability. These patients can also perform CPX without completing the 6-min walk of stage 6.
*Patients with severe disease who cannot progress through the ambulation program and who cannot be weaned off catecholamines: investigate intensification of pharmacotherapy, and the indication of concurrent “Waon” therapy21
or nonpharmaceutical treatments (CRT, mitral annuloplasty, and auxiliary artificial heart) in order to help them progress even slightly more. In general, exercise training is contraindicated in patients with NYHA class IV HF; however, in patients with stable hemodynamics receiving catecholamine treatment, disuse syndrome can be prevented by carefully performing bedside muscle strength training.
*When frail patients are unable to progress through the ambulation program, they can be transported to the rehabilitation room upon completion of the intravenous drip management, to perform muscle strength training, and train for independence in ADLs. Please refer to Chapter V for details.
Hereafter, please see
Supplementary File
because of the limitation of number of letters.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-19-0670
References
- 1.
Okura Y, Ramadan MM, Ohno Y, Mitsuma W, Tanaka K, Ito M, et al. Impending epidemic: Future projection of heart failure in Japan to the year 2055. Circ J 2008; 72: 489–491.
- 2.
Jong P, Yusuf S, Rousseau MF, Ahn SA, Bangdiwala SI. Effect of enalapril on 12-year survival and life expectancy in patients with left ventricular systolic dysfunction: A follow-up study. Lancet 2003; 361: 1843–1848.
- 3.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Executive summary: Heart disease and stroke statistics–2016 update: A report from the American Heart Association. Circulation 2016; 133: 447–454.
- 4.
Shimokawa H, Miura M, Nochioka K, Sakata Y. Heart failure as a general pandemic in Asia. Eur J Heart Fail 2015; 17: 884–892.
- 5.
May GS, Eberlein KA, Furberg CD, Passamani ER, DeMets DL. Secondary prevention after myocardial infarction: A review of long-term trials. Prog Cardiovasc Dis 1982; 24: 331–352.
- 6.
Witt BJ, Jacobsen SJ, Weston SA, Killian JM, Meverden RA, Allison TG, et al. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol 2004; 44: 988–996.
- 7.
Wenger NK. Current status of cardiac rehabilitation. J Am Coll Cardiol 2008; 51: 1619–1631.
- 8.
Kubo H, Yano K, Hirai H, Yabuki S, Machii K. Preventive effect of exercise training on recurrent stenosis after percutaneous transluminal coronary angioplasty (PTCA). Jpn Circ J 1992; 56: 413–421.
- 9.
Belardinelli R, Paolini I, Cianci G, Piva R, Georgiou D, Purcaro A. Exercise training intervention after coronary angioplasty: The ETICA Trial. J Am Coll Cardiol 2001; 37: 1891–1900.
- 10.
Dubach P, Litscher K, Kuhn M, Laske P, Buser P, Miller P, et al. Cardiac rehabilitation in Switzerland: Efficacy of the residential approach following bypass surgery. Chest 1993; 103: 611–615.
- 11.
Demopoulos L, Bijou R, Fergus I, Jones M, Strom J, LeJemtel TH. Exercise training in patients with severe congestive heart failure: Enhancing peak aerobic capacity while minimizing the increase in ventricular wall stress. J Am Coll Cardiol 1997; 29: 597–603.
- 12.
Hambrecht R, Fiehn E, Weigl C, Gielen S, Hamann C, Kaiser R, et al. Regular physical exercise corrects endothelial dysfunction and improves exercise capacity in patients with chronic heart failure. Circulation 1998; 98: 2709–2715.
- 13.
Belardinelli R, Georgion D, Giovanni C, Gielen S, Hamann C, Kaiser R, et al. Randomized controlled trial of long term moderate training in chronic heart failure. Circulation 1999; 99: 1173–1182.
- 14.
ExTraMATCH Collaborative. Exercise training meta-analysis of trials in patients with chronic heart failure (ExTraMATCH). BMJ 2004; 328: 189–192.
- 15.
Linke A, Adams V, Schulze PC, Erbs S, Gielen S, Fiehn E, et al. Antioxidative effects of exercise training in patients with chronic heart failure: Increase in radical scavenger enzyme activity in skeletal muscle. Circulation 2005; 111: 1763–1770.
- 16.
O’Connor CM, Whellan DJ, Lee KL, Keteyian SJ, Cooper LS, Ellis SJ, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 2009; 301: 1439–1450.
- 17.
McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: A systematic review of randomized trials. J Am Coll Cardiol 2004; 44: 810–819.
- 18.
Davidson PM, Cockburn J, Newton PJ, Webster JK, Betihavas V, Howes L, et al. Can a heart failure-specific cardiac rehabilitation program decrease hospitalizations and improve outcomes in high-risk patients? Eur J Cardiovasc Prev Rehabil 2010; 17: 393–402.
- 19.
Arakawa T, Kumasaka L, Nakanishi M, Nagayama M, Adachi H, Ikeda K, et al. Regional clinical alliance path and cardiac rehabilitation after hospital discharge for acute myocardial infarction patients in Japan: A nationwide survey. Circ J 2016; 80: 1750–1755.
- 20.
JCS Joint Working Group. Guidelines for rehabilitation in patients with cardiovascular disease (JCS 2012): Digest version. Circ J 2014; 78: 2022–2093.
- 21.
Tei C, Imamura T, Kinugawa K, Inoue T, Masuyama T, Inoue H, et al; WAON-CHF Study Investigators. Waon therapy for managing chronic heart failure: Results from a multicenter prospective randomized WAON-CHF Study. Circ J 2016; 80: 827–834.