2019 年 83 巻 12 号 p. 2416-2417
2019 年 83 巻 12 号 p. 2416-2417
The grafting of the internal thoracic artery (ITA) to the left anterior descending artery brings better long-term survival results compared with the usage of saphenous vein graft after coronary artery bypass graft surgery (CABG),1 and it is strongly recommended in guidelines (Figure 1).2 ITA usage in CABG is >97% in Japan.3 Usually, the cardiac surgeon would not hesitate to use 1 ITA graft even when required to do a concomitant cardiac operation (e.g., valve operation, aortic operation). However, nobody would be certain about using bilateral ITA (BITA) for patients with multivessel disease.
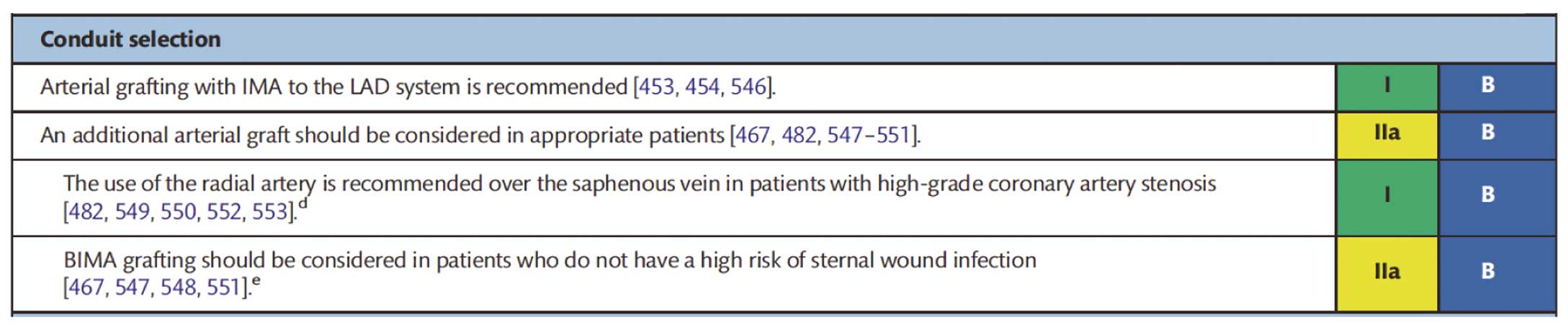
Recommendations on procedural aspects of coronary artery bypass grafting. IMA, internal mammary artery; LAD, left anterior descending. (Already requested to reuse to Eur J Cardiothorac Surg publisher, Oxford Academic.8)
Article p 2466
In this issue of the Journal, Gatti et al report on the safety of using BITA concomitant with other cardiac operations.4 They note that although the use of BITA in such cases is risky and the increased operation duration, risk of bleeding and sternal complications because of BITA harvest might outweigh the potential benefits of BITA, such as reduced manipulation of the ascending aorta and long-term survival rate, it can be performed with satisfactory results. Also, the long-term outcomes mostly depend on sex, preoperative comorbidities and baseline cardiac function. They collected data from 3 European institutes for 1,123 patients who underwent combined CABG using BITA with other cardiac surgery, valve operation, left ventricular or thoracic aortic operations.
It is still controversial whether BITA usage even in isolated CABG brings better long-term results compared with SITA usage. Since the reports that 2 ITA grafts are better than 1,5–7 the passion for multiple arterial grafting or total arterial grafting has been increasing. However, usage of BITA in the USA or in European countries is not high at around 5–10%.8 The reasons for the low usage of BITA are long duration of operation, more bleeding and concern about sternal infections. In the European guideline, usage of the right ITA is limited to patients who do not have a high risk of sternal infection.2 Gaudino et al began using systematic BITA grafting, but concluded that in the real-world setting it was associated with a higher incidence of perioperative adverse events (particularly sternal complications) and they stopped the study.9 Because there had not been a randomized study of comparison between SITA and BITA until the Arterial Revascularization Trial (ART)10 was designed, it was controversial and the usage of BITA depended on surgeon’s preference.
ART is an international multicenter randomized study enrolling more than 31,000 patients. Recently the 10-year outcomes were published and concluded there was no difference in the primary endpoint of death at 10 years (20.3% in the BITA group and 21.2% in the SITA group: P=0.62) (Figure 2). It was a sort of shocking report, indicating there is no rationale to use BITA in CABG. There are, however, some confusing methodological problems with that study: 40% of the patients in ART actually received a different treatment strategy from that initially proposed; 22% of the SITA group received a radial artery graft as the second arterial graft and there were high crossovers from the BITA to SITA group (14%) and low crossovers from SITA to BITA (4%). Taggart et al did honestly as-treated analysis to compare outcomes in patients who received a SITA with other vein graft and those in the BITA group who received ≥2 arterial grafts, showing 8% difference in absolute survival in favor of multiple arterial grafts and likewise a highly significant reduction in the composite of death, myocardial infarction and stroke, with divergence between the groups although it was not randomized study.8
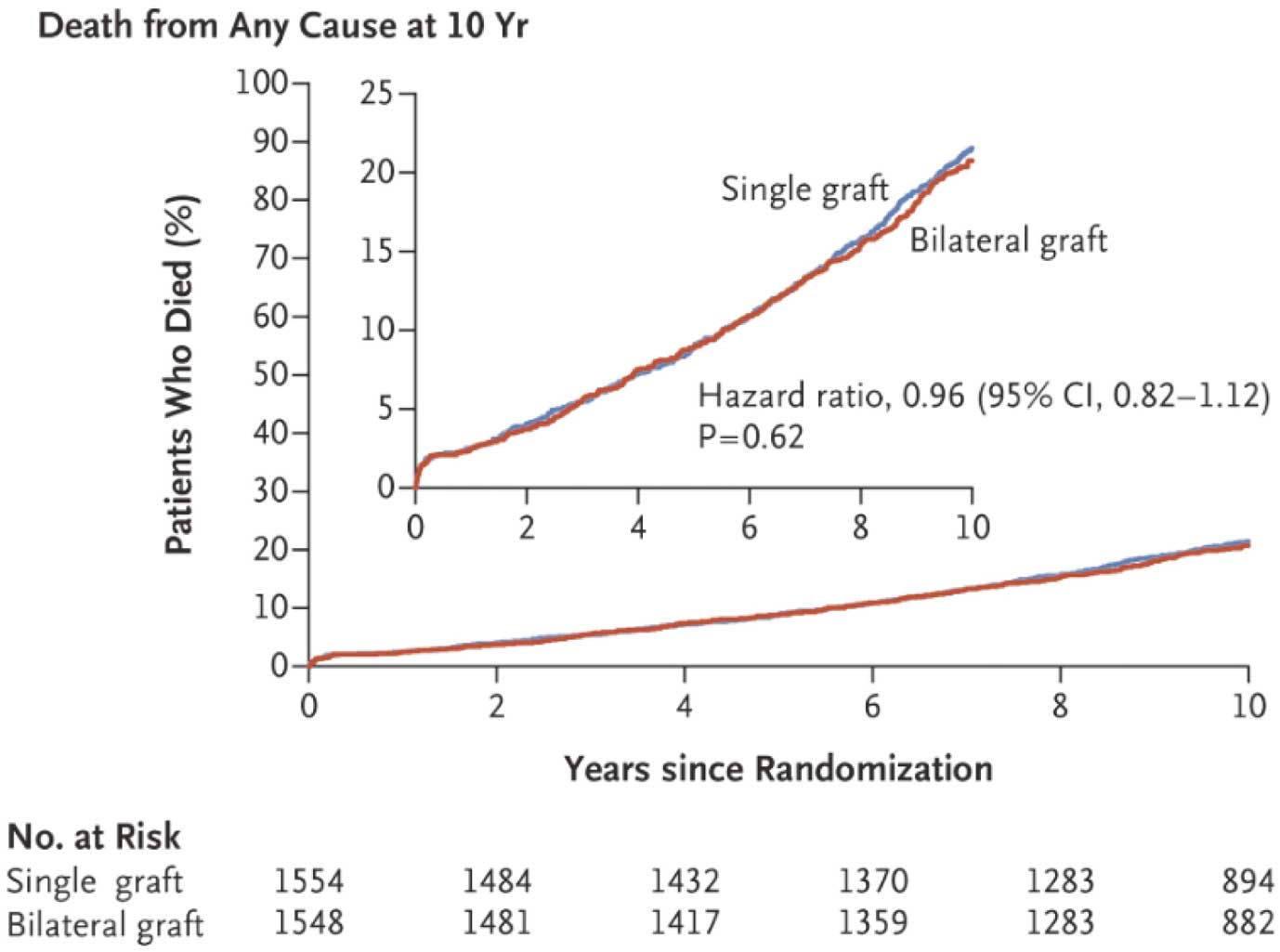
Comparison of survival rate between groups with single and bilateral usage of internal thoracic artery. CI, confidence interval. (Already requested to reuse to N Engl J Med.10)
Even in isolated CABG, it appears difficult to show the advantage of BITA usage. Furthermore, there is no study on whether BITA-based CABG is better than SITA-used CABG with other concomitant cardiac operations. The predictors for long-term outcome after combined coronary revascularization and other cardiac operation depends on the factors associated with CABG and the valvular, left ventricular or aortic operation. According to their conclusion, the predictors were sex, preoperative comorbidities and baseline cardiac function. They conclude that BITA grafting concomitant with other cardiac operations may be performed with acceptable hospital mortality and postoperative complication rates.
As they mention, there are some limitations, including retrospective study, data from 3 different centers and a period spanning about 20 years. The study did not target a comparison of BITA and SITA use. So they added the comparison between BITA and SITA use. There was no significant difference after adjusting for multiple covariates.
Although they could not show the superiority of BITA usage over SITA usage with concomitant other cardiac operations, they at least showed that BITA can be used with acceptable mortality and morbidity and acceptable long-time survival. There has not been a study targeting the feasibility and safety of BITA usage and this requires further evaluation.