Abstract
Background:
Evaluate the safety and efficacy of guideline-recommended risk score-directed dual antiplatelet therapy (GD-DAPT) based on THE PRECISE-DAPT score after 2nd-generation drug-eluting stent (DES) implantation.
Methods and Results:
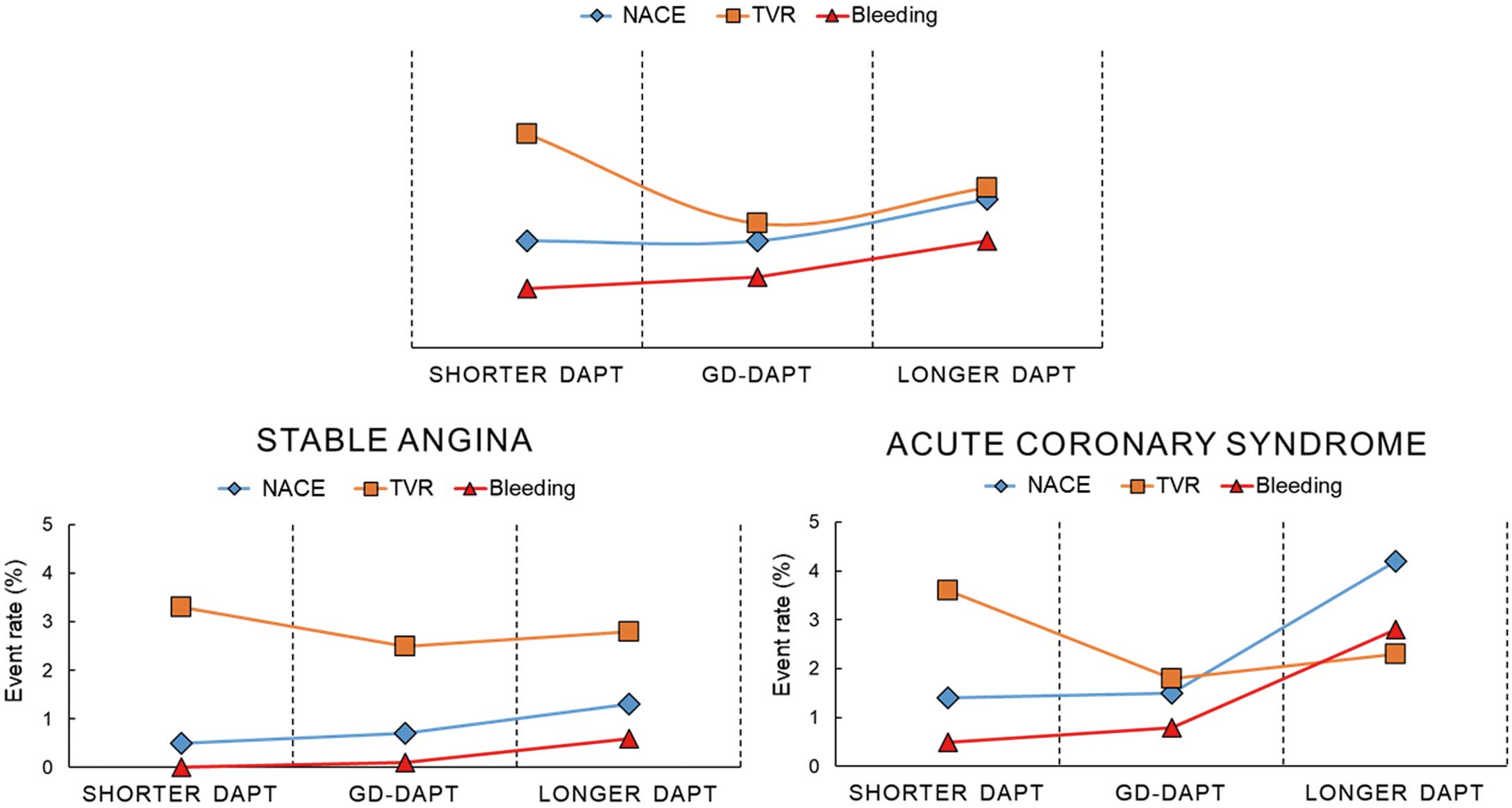
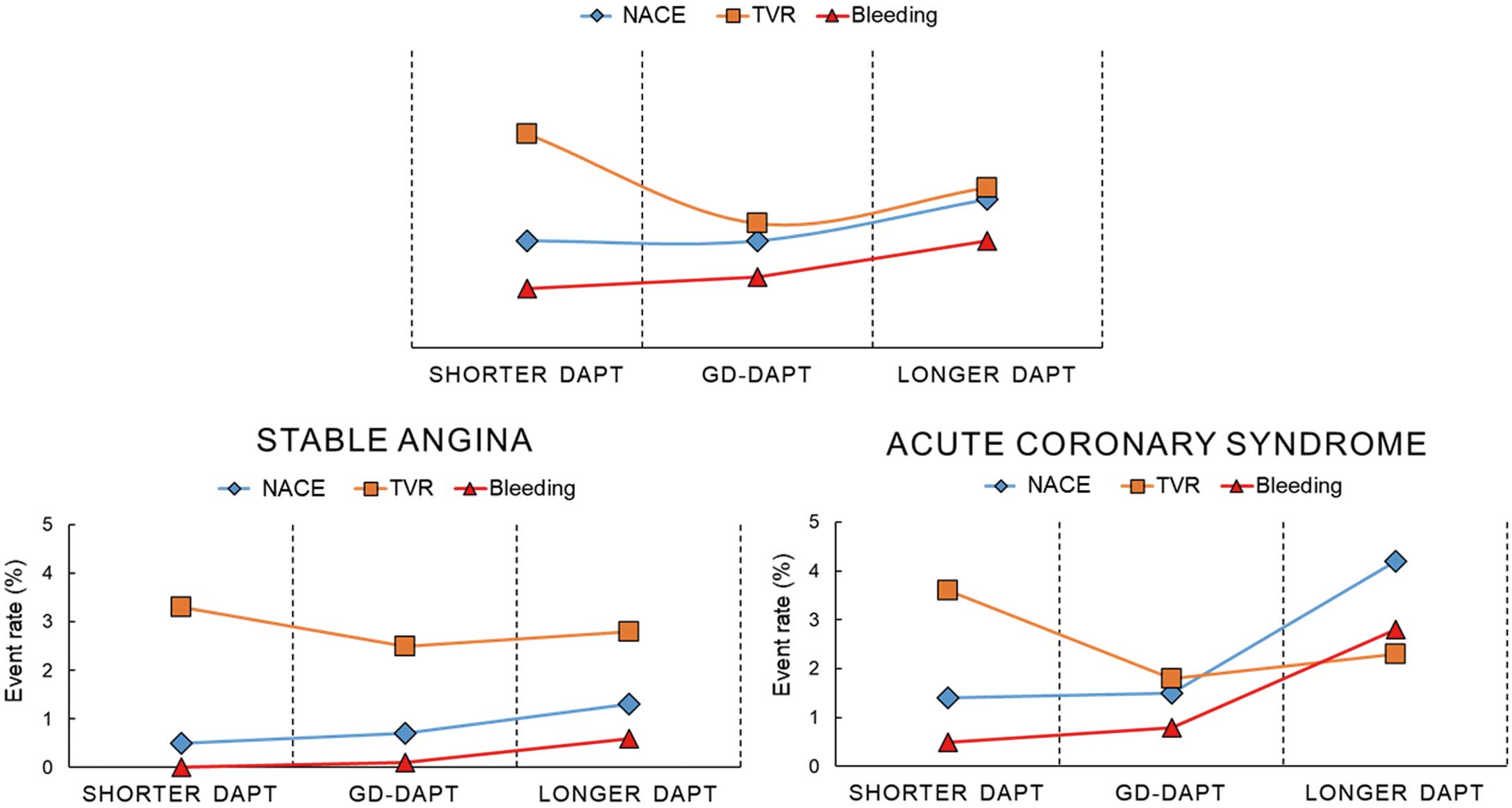
We analyzed 5,131 patients pooled from 4 clinical trials. Patients were divided into 3 groups according to current recommendations on the duration of DAPT and their actual DAPT duration: GD-DAPT (n=2,183), shorter DAPT (n=1,540), longer DAPT (n=1,408). The primary endpoint was the rate of net adverse clinical events (NACE) during the first 12 months. The secondary endpoints were ischemic or bleeding events. Overall, GD-DAPT did not affect NACE (1.2% vs. 1.2% for shorter DAPT and 1.7% for longer DAPT) or bleeding events (0.6% vs. 0.5% and 0.9%), and there were fewer ischemic events (2.8% vs. 4.4% and 4.0%, P=0.03) than with shorter DAPT. Especially in acute coronary syndrome (ACS) patients, GD-DAPT had fewer NACE (1.5% vs. 1.4% and 4.2%; P=0.006) and bleeding events (0.8% vs. 0.5% and 2.8%; P=0.001) than longer DAPT as well as fewer ischemic events (2.8% vs. 4.4% and 4.7%; P=0.03) than shorter DAPT.
Conclusions:
GD-DAPT did not affect NACE or bleeding events and reduced the number of ischemic events at 12 months compared with shorter DAPT. For ACS, GD-DAPT was associated with favorable outcomes compared with non-GD-DAPT. Therefore, GD-DAPT may optimize efficacy and safety.
Dual antiplatelet therapy (DAPT) effectively treats ischemic heart disease by preventing thrombotic complications, especially after stent implantation.1
With 1st-generation drug-eluting stents (DES), DAPT therapy was recommended for 12 months to prevent late or very late stent thrombosis (ST).2
However, the clinical benefits of longer DAPT have been attenuated following the introduction of improved stent technology that has reduced thrombotic events, including the 2nd-generation DES.3
Importantly, results have consistently shown that during longer DAPT, there is a trade-off between fewer ischemic events and increased bleeding events.4
Alternatively, studies evaluating the clinical compatibility of short-term DAPT showed non-inferior clinical outcomes for patients with low thrombotic risk.5–9
However, similar analysis revealed high variability for higher thrombotic risk patients, including those with acute coronary syndrome (ACS).10–12
Editorial p 153
These conflicting findings make determining the optimal DAPT duration difficult, thereby increasing the demand for individualized DAPT duration regimens based on each patient’s ischemic and bleeding risks. The 2017 European Society of Cardiology guidelines on the management of DAPT advocate the use of the PRECISE-DAPT score as a tool for predicting the risk of out-of-hospital bleeding after percutaneous coronary intervention (PCI) and, hence, inform decision-making on the optimal duration of DAPT.13,14
However, clinical data regarding DAPT strategies, based on guideline-recommended risk score-directed (GD)-DAPT with 2nd-generation DES, are limited. Therefore, we evaluated the safety and efficacy of GD-DAPT compared with shorter or longer DAPT by analyzing the data of patients who were treated with 2nd-generation DES pooled from 4 random study populations: Effect of Intravascular Ultrasound-Guided vs. Angiography-Guided Everolimus-Eluting Stent Implantation (IVUS-XPL); REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation (RESET); safety of 6-month dual antiplatelet therapy after second-generation drug-eluting stent implantation (OPTIMA-C); and the Efficacy of Xience/Promus Versus Cypher to Reduce Late Loss After Stenting (EXCELLENT).6–9
Methods
Study Design
This was a patient-level pooled analysis of data from 4 multicenter, prospective, open-label, randomized trials comparing the effects of short-duration (≤6 months) and standard-duration (≥12 months) DAPT. Patients who were treated with a 2nd-generation DES and had the PRECISE-DAPT score available were included. Each study protocol is summarized in
Supplementary Table 1. Briefly, the IVUS-XPL trial included 1,400 patients who underwent everolimus DES implantation for long coronary lesions (implanted stent length ≥28 mm). The patients were randomly assigned to treatments using a 2×2 factorial design according to DAPT duration (6 vs. 12 months) and whether intravascular ultrasound was used.6
The RESET trial enrolled 2,117 patients who were randomly assigned in a 1:1 ratio to receive either an Endeavor zotarolimus DES with 3 months of DAPT or a Resolute zotarolimus DES, everolimus DES, or 1st-generation sirolimus DES with 12 months of DAPT.7
The OPTIMA-C trial enrolled 1,367 patients with at least 1 de novo lesion treated with a biolimus or zotarolimus DES randomly assigned to DAPT for 6 or 12 months.8
The EXCELLENT trial enrolled 1,443 patients with at least 1 de novo lesion treated with an everolimus or 1st-generation sirolimus DES.9
From a total of 6,327 patients, 1,045 treated with a 1st-generation DES were excluded, leaving a study population of 5,282 patients treated with a 2nd-generation DES. PRECISE-DAPT scores were calculated using a web calculator (www.precisedapt.com). Patients lacking PRECISE-DAPT scores (n=151) were also excluded, resulting in a final study population of 5,131 patients. For high bleeding risk patients (PRECISE-DAPT score ≥25), European guidelines suggest 6 months of DAPT for ACS and 3 months for stable angina. For non-high bleeding risk patients, the guidelines recommend 12 months DAPT for ACS and 6 months for stable angina.13,14
Based on these guidelines, we divided patients into 3 groups: shorter DAPT duration than the guideline (shorter DAPT, n=1,540), GD-DAPT (n=2,183), and longer DAPT duration than the guideline (longer DAPT, n=1,408). Both shorter and longer DAPT were classified as non-GD-DAPT (n=2,948) (Figure 1). Subgroup analysis was performed based on DAPT duration relative to both the guideline and clinical presentation.

The primary endpoint was net adverse clinical events (NACE), comprising cardiac death, myocardial infarction (MI), ST, stroke, or major bleeding during the first 12 months. Secondary endpoints were ischemic and bleeding events. Ischemic events were defined as a composite of cardiac death, MI, ST, stroke, or ischemia-driven target vessel revascularization (TVR). Bleeding events met the Thrombolysis in Myocardial Infarction (TIMI) criteria for minor or major bleeding events. Clinical events were defined according to the recommendations of the Academic Research Consortium.15
All deaths were considered cardiac unless a definite non-cardiac cause was established. MI was defined as the presence of clinical signs of MI, plus a creatine kinase-MB fraction or troponin T or I increase above the upper normal limit. ST was defined as definite or probable ST. Stroke was defined according to the definition used in each trial. TVR was defined as ischemia-driven repeat revascularization of the treated vessel by PCI or bypass surgery.
Statistical Analysis
Patient-level data were obtained from the principal investigators of each trial. Individual patient data were pooled into a single dataset and analyzed with a single-stage approach. We used the intention-to-treat population for analysis. Continuous variables, presented as mean (standard deviation [SD]), were compared using Student’s t-test or ANOVA. Categorical variables, presented as count (percentage), were compared using the χ2
test or Fisher’s exact test, as appropriate. Cumulative event rates were estimated using the Kaplan-Meier method, and survival curves were compared using the log-rank test stratified by the trial in which the patients were enrolled. Multivariate Cox proportional analysis was performed to compare hazards of each adverse event between DAPT strategies, adjusting for potential confounders. Explanatory variables with P-values <0.2 in the univariate analysis were considered for inclusion in the multivariable models, including age, sex, diabetes mellitus, hypertension, ACS, and type of DES. Two-sided P-value <0.05 was considered significant. All analyses were performed using SAS version 9.2 (SAS Institute, Inc., Cary, NC, USA).
Results
Of the 5,131 patients, the numbers in the shorter DAPT, GD-DAPT, and longer DAPT groups were 1,540, 2,183, and 1,408, respectively. The longer DAPT group was older, and had more females, hypertension, and diabetes (Table 1,
Supplementary Tables 2,3). Overall, NACE did not differ among the 3 DAPT groups (1.2% for GD-DAPT vs. 1.2% for shorter DAPT and 1.7% for longer DAPT,
Table 2, Figure 2). Shorter DAPT significantly increased the rate of TVR relative to the other groups (2.1% vs. 3.6% and 2.7%; P=0.02) and the rate of ischemic events (2.8%, 4.4% and 4.0%; P=0.03). The frequency of bleeding events gradually increased with DAPT duration (0.6% vs. 0.5%, and 0.9%), but was not statistically significant because of the overall low incidence of bleeding events. In the multivariate analysis, shorter DAPT was significant predictor for TVR (hazard ratio (HR) 1.88 [95% confidence interval (CI) 1.26–2.80], P=0.002) and ischemic events (HR 1.64 [95% CI 1.16–2.32], P=0.005).
Table 1.
Clinical and Angiographic Characteristics of the DAPT Subgroups
| Characteristics |
Shorter DAPT
(n=1,540) |
GD DAPT
(n=2,183) |
Longer DAPT
(n=1,408) |
P value |
| Age, (years) |
62±9 |
62±10 |
66±10 |
0.001 |
| Male sex |
1,047 (68.0) |
1,524 (69.8) |
846 (60.1) |
0.001 |
| Diabetes mellitus |
527 (34.2) |
713 (32.7) |
611 (43.4) |
0.001 |
| Hypertension |
966 (62.7) |
1,384 (63.4) |
1,006 (71.4) |
0.001 |
| CHF |
96 (7.6) |
81 (5.3) |
44 (4.4) |
0.003 |
| Current smoker |
453 (29.4) |
582 (26.7) |
286 (20.3) |
0.001 |
| Clinical presentation at index procedure |
|
|
|
0.001 |
| Stable angina |
209 (13.6) |
808 (37.0) |
1,194 (84.8) |
|
| Unstable angina |
956 (62.1) |
980 (44.9) |
141 (10.0) |
|
| Non-ST-elevation MI |
336 (21.8) |
361 (16.5) |
69 (4.9) |
|
| ST-elevation MI |
39 (2.5) |
34 (1.6) |
4 (0.3) |
|
| Prior PCI |
94 (6.1) |
179 (8.2) |
131 (9.3) |
0.004 |
| Prior MI |
58 (3.8) |
76 (3.5) |
46 (3.3) |
0.76 |
| LVEF, % |
62±10 |
63±9 |
63±9 |
0.01 |
| PRECISE-DAPT score groups† |
|
|
|
0.001 |
| Very low |
551 (35.8) |
828 (37.9) |
364 (25.9) |
|
| Low |
570 (37.0) |
767 (35.1) |
404 (28.7) |
|
| Moderate |
328 (21.3) |
455 (20.8) |
201 (14.3) |
|
| High |
91 (5.9) |
133 (6.1) |
439 (13.1) |
|
| Angiographic variables |
| No. of diseased vessels |
|
|
|
0.08 |
| 1 |
764 (49.6) |
1,084 (49.7) |
637 (45.2) |
|
| 2 |
460 (29.9) |
654 (30.0) |
467 (33.2) |
|
| 3 |
316 (20.5) |
445 (20.3) |
304 (21.6) |
|
| Stent type |
|
|
|
0.001 |
| EES |
540 (35.0) |
1,262 (57.8) |
873 (62.0) |
|
| Endeavor ZES |
856 (55.6) |
315 (14.4) |
193 (13.7) |
|
| Resolute ZES |
0 |
313 (14.4) |
122 (8.7) |
|
| BES |
144 (9.4) |
293 (13.4) |
220 (15.6) |
|
| No. of stents per patient |
1.4±0.7 |
1.4±0.7 |
1.5±0.7 |
0.002 |
| Total stent length (mm) |
32±18 |
32±18 |
34±18 |
0.04 |
Data are presented as n (%) or mean±SD. BES, biolimus-eluting stent; CHF, congestive heart failure; EES, everolimus-eluting stent; GD-DAPT, guideline-recommended score-directed dual antiplatelet therapy; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention; ZES, zotarolimus-eluting stent.
Table 2.
Clinical Outcomes in the First 12 Months Among the DAPT Subgroups
| |
Shorter DAPT
(n=1,540) |
GD-DAPT
(n=2,183) |
Longer
DAPT
(n=1,408) |
HR (95%CI)
for shorter
DAPT |
P value* |
P value† |
HR (95% CI)
for longer
DAPT |
P value* |
P value† |
| NACE |
19
(1.2) |
26
(1.2) |
24
(1.7) |
0.93
(0.50–1.71) |
0.82 |
0.37 |
1.24
(0.70–2.17) |
0.46 |
0.85 |
Cardiac death, MI,
ST, or stroke |
17
(1.1) |
21
(1.0) |
21
(1.5) |
1.12
(0.58–2.17) |
0.73 |
0.55 |
1.36
(0.74–2.50) |
0.33 |
0.90 |
| ST |
6
(0.4) |
6
(0.3) |
1
(0.1) |
1.53
(0.49–4.78) |
0.46 |
0.87 |
0.25
(0.03–2.08) |
0.20 |
0.99 |
| TVR |
55
(3.6) |
45
(2.1) |
38
(2.7) |
1.88
(1.26–2.80) |
0.002 |
0.69 |
1.25
(0.81–1.94) |
0.31 |
0.79 |
| Non-TVR |
20
(1.3) |
23
(1.1) |
19
(1.3) |
1.17
(0.63–2.17) |
0.62 |
0.45 |
1.38
(0.74–2.57) |
0.30 |
0.52 |
| Ischemic event |
67
(4.4) |
62
(2.8) |
57
(4.0) |
1.64
(1.16–2.32) |
0.005 |
0.49 |
1.34
(0.93–1.92) |
0.12 |
0.87 |
| Bleeding event |
7
(0.5) |
12
(0.6) |
13
(0.9) |
0.64
(0.25–1.68) |
0.37 |
0.82 |
1.50
(0.67–3.36) |
0.32 |
0.94 |
Stable angina
(n=2,211) |
209 |
808 |
1,194 |
|
|
|
|
|
|
| NACE |
1
(0.5) |
6
(0.7) |
15
(1.3) |
0.58
(0.07–5.10) |
0.62 |
|
1.46
(0.56–3.81) |
0.44 |
|
Cardiac death, MI,
ST, or stroke |
1
(0.5) |
5
(0.6) |
14
(1.2) |
0.85
(0.09–7.71) |
0.88 |
|
1.71
(0.61–4.80) |
0.31 |
|
| ST |
0 |
2
(0.2) |
0 |
Not available |
|
|
Not available |
|
|
| TVR |
7
(3.3) |
20
(2.5) |
33
(2.8) |
1.39
(0.50–3.89) |
0.53 |
|
1.08
(0.61–1.90) |
0.79 |
|
| Non-TVR |
2
(1.0) |
7
(0.9) |
17
(1.4) |
2.22
(0.27–18.2) |
0.46 |
|
1.78
(0.73–4.38) |
0.21 |
|
| Ischemic event |
8
(3.8) |
24
(3.0) |
47
(3.9) |
1.16
(0.45–2.99) |
0.76 |
|
1.23
(0.74–2.04) |
0.43 |
|
| Bleeding event |
0 |
1
(0.1) |
7
(0.6) |
Not available |
|
|
3.44
(0.41–28.8) |
0.03 |
|
| ACS (n=2,920) |
1,331 |
1,375 |
214 |
|
|
|
|
|
|
| NACE |
18
(1.4) |
20
(1.5) |
9
(4.2) |
0.88
(0.47–1.67) |
0.70 |
|
2.41
(1.06–5.48) |
0.04 |
|
Cardiac death, MI,
ST, or stroke |
16
(1.2) |
16
(1.2) |
7
(3.3) |
1.02
(0.51–2.03) |
0.97 |
|
2.43
(0.97–6.12) |
0.06 |
|
| ST |
6
(0.5) |
4
(0.3) |
1
(0.5) |
1.48
(0.42–5.26) |
0.54 |
|
1.85
(0.20–17.2) |
0.59 |
|
| TVR |
48
(3.6) |
25
(1.8) |
5
(2.3) |
2.06
(1.27–3.35) |
0.04 |
|
1.20
(0.45–3.19) |
0.72 |
|
| Non-TVR |
18
(1.4) |
16
(1.2) |
2
(0.9) |
1.19
(0.60–2.36) |
0.62 |
|
0.88
(0.19–4.01) |
0.87 |
|
| Ischemic event |
59
(4.4) |
38
(2.8) |
10
(4.7) |
1.63
(1.08–2.45) |
0.02 |
|
1.50
(0.73–3.06) |
0.27 |
|
| Bleeding event |
7
(0.5) |
11
(0.8) |
6
(2.8) |
0.60
(0.23–1.56) |
0.30 |
|
2.95
(1.03–8.48) |
0.04 |
|
Data are presented as number (%). *Multivariate proportional Cox analysis, including variables with P-values <0.2 in univariate analysis. †Interaction between each DAPT group (GD-DAPT group as reference) and clinical presentation (acute coronary syndrome vs. stable angina). GD-DAPT, guideline-recommended score-directed dual antiplatelet therapy; MI, myocardial infarction; NACE, net clinical adverse events; ST, stent thrombosis; TVR, target vessel revascularization.

For stable angina patients, although longer DAPT increased NACE, these differences were not significant because of their overall low incidence (Figure 3). The bleeding event rate was higher in the longer DAPT group. TVR and ischemic event rates were similar between GD-DAPT and shorter DAPT.

In ACS patients, longer DAPT was associated with increased NACE (1.5% vs. 1.4%, and 4.2%; P=0.006) and bleeding events (0.8% vs. 0.5% and 2.8%; P=0.001) compared with the other groups. Even after excluding procedure-related bleeding, longer DAPT still increased the number of bleeding events (Supplementary Figure 1). Shorter DAPT significantly increased the rate of TVR (1.8% vs. 3.6% and 2.3%, P=0.008) and ischemic events (2.8% vs. 4.4% and 4.7% , P= 0.03). In the multivariate analysis, longer DAPT was a significant predictor for NACE (HR 2.41 [95% CI, 1.06–5.48], P=0.04) and bleeding events (HR 2.95 [95% CI, 1.03–8.48], P=0.04), whereas shorter DAPT was a predictor for TVR (HR 2.06 [95% CI, 1.27–3.35], P=0.04) and ischemic events (HR 1.63 [95% CI, 1.08–2.45], P=0.02). Interestingly, there was a negative association between TVR and NACE frequency with regards to DAPT duration. Specifically, longer DAPT increased the risk of NACE and bleeding compared with GD-DAPT. In contrast, shorter DAPT increased the risk of ischemic event and TVR compared with GD-DAPT. Therefore, GD-DAPT may optimize the balance between thrombotic and bleeding events (Figure 4).
Discussion
In this pooled analysis involving patients treated with 2nd-generation DES, GD-DAPT did not affect NACE or bleeding events, but reduced TVR and ischemic events at 12 months compared with shorter DAPT. In ACS, GD-DAPT reduced NACE and bleeding events compared with longer DAPT, and lowered the TVR and ischemic rates compared with shorter DAPT. Therefore, individualized DAPT duration regimens according to PRECISE-DAPT bleeding scores could optimize both the efficacy and safety of DAPT, especially in patients with ACS (Supplementary Figure 2).
Although 12 months of DAPT therapy is recommended for preventing ST with 1st-generation DES,2
the incidence of ST has declined considerably following the advent of safer, newer-generation DES. Indeed, a recent study of optimal stent implantation showed zero ST incidence after 1 year with everolimus stents.16
Furthermore, the SECURITY trial, which evaluated short DAPT after 2nd-generation DES implantation, showed no additional benefit of DAPT therapy for 12 months.5
Because potent and prolonged antiplatelet therapy increases the bleeding risk, prolonged DAPT is not justified by the currently small benefit towards ST prevention.
However, data also suggest that potent antiplatelet therapy can reduce ischemic events, including non-stent-related MI and stroke, for high ischemic risk patients. Such patients include post-acute MI or patients who have undergone complex coronary interventions.10,17
Indeed, the SMART-DATE trial, which evaluated 2nd-generation DES for ACS, showed that short DAPT increased MI incidence compared with the standard DAPT duration.12
This discrepancy created the need for risk stratification to determine which patients would benefit from shorter or longer DAPT, based on individual bleeding and ischemic event risk. Current European guidelines recommend a well-validated 2-score system. DAPT duration within 1 year is based on PRECISE-DAPT, and that after 1 year is based on the DAPT score.13
However, tailored DAPT duration has not yet been validated in terms of efficacy and safety after treatment with 2nd-generation DES.
Our data showed that GD-DAPT did not reduce NACE or bleeding events compared with non-GD-DAPT, which suggests that DAPT does not confer significant clinical benefits in patients treated with 2nd-generation DES, because of the low overall incidence of such events. However, shorter DAPT increased the rate of early ischemia-driven TVR. Although TVR is considered as a soft event, recent meta-analysis has shown that TVR is related to increased long-term mortality.18
Therefore, further evaluation of the long-term safety of shorter DAPT in terms of thrombotic events is needed.
In ACS, longer DAPT was significantly associated with high NACE and bleeding events. NACE as a net clinical outcome was significantly associated with the major bleeding event itself, as well as with subsequent ischemic events, because of discontinuation of antiplatelet agents. More than half of recorded NACE were bleeding events in the longer DAPT group, which means that lower thrombotic risk combined with the safety of 2nd-generation DES attenuated the clinical benefits of longer DAPT for reducing ischemic events. Furthermore, previous reports showed that longer DAPT or potent P12Y12 inhibitors increased bleeding events as well as major adverse cardiovascular and clinical events (MACCE).19
These findings can be explained by increased bleeding events, which may be associated with higher MACCE caused by bleeding events and a higher tendency to discontinue antiplatelet agents after bleeding events. However, our results should be interpreted with caution because the majority of ACS cases was unstable angina, with relatively lower ischemic risk than MI. The SMART-DATE trial included a higher ischemic risk population with more than half of the patients experiencing acute MI and showing longer DAPT (>12 months) and reduced recurrent MI events.12
Therefore, ischemic risk stratification, in addition to the suggested bleeding risk stratification, might require tailored DAPT regimens to consider the ischemic and bleeding risks in each clinical situation.20
Bleeding events are ultimately associated with poor clinical outcomes. In the PARIS registry, disruptions because of bleeding or non-compliance were associated with a substantial increase in MACE.21
Once bleeding events occur, DAPT cannot be reduced, because the amount of ongoing bleeding is unpredictable. Transfusion followed by bleeding also increases thrombotic risk.22
Even without a transfusion, enhanced hematopoietic function increases the platelet turnover rate. Furthermore, immature platelets not inhibited by clopidogrel can increase the thrombotic risk.23
Iron deficiency combined with chronic anemia after DAPT also affects clinical outcomes. In our study, one-third of bleeding events were chronic severe anemia with unknown bleeding focus (Supplementary Table 4). Chronic blood loss with DAPT can enhance iron deficiency. Iron, in addition to oxygen transport and storage, is also fundamental for the activity of key enzymes in the citric acid cycle and for metabolism of reactive oxygen species. Iron deficiency impairs cellular energy release and exacerbates atrophy and cardiac apoptosis. However, the clinical relevance of iron deficiency in coronary disease must be further investigated.
Study Limitations
First, only clopidogrel was used with aspirin as DAPT in our studies, so we could not expand the effects of GD-DAPT with other antiplatelet agents, such as ticagrelor or prasugrel. Second, we could not evaluate DAPT shorter than the guideline for stable angina or patients with very high bleeding risk, as there were no data on DAPT of less than 3 months in this analysis. Data from recent random trials evaluating 1-month DAPT followed by ticagrelor monotherapy suggest this was not superior to 12 months of DAPT in preventing all-cause death or MI in both stable angina and ACS patients.24
This suggests that DAPT duration only based on clinical presentation may not be sufficient to optimize clinical outcomes. Therefore, more precise and personalized DAPT treatment may be needed. Third, in our study, the incidence of bleeding events was low, potentially because of most of the study population had non-high bleeding risk or there was a lack of detailed information on bleeding. Indeed, only the TIMI bleeding criteria were available in our study, so bleeding events may have been underestimated. Fourth, 1 year of clinical follow-up may not be sufficient to assess late outcomes, and we could not evaluate the efficacy and safety of DAPT score-based therapy after 1 year. Finally, our study showed an association between guideline-based DAPT and optimal clinical results rather than causality. Therefore, our observations should be considered as non-conclusive and hypothesis-generating.
At 12 months, GD-DAPT did not affect NACE or bleeding events, but reduced ischemic events compared with shorter GD-DAPT. For ACS, GD-DAPT was associated with low NACE compared with longer DAPT and reduced TVR frequency compared with shorter DAPT, with a modest bleeding event rate. Thus, GD-DAPT may optimize treatment efficacy and safety after 2nd-generation DES implantation, particularly in ACS patients.
Acknowledgments
Funding/Support:
This work was supported by a grant from the Korea Healthcare Technology Research & Development Project, Ministry for Health & Welfare, Republic of Korea [grant numbers A085136, HI15C1277], the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) [grant number 2017R1A2B2003191], and the Cardiovascular Research Centre, Seoul, Korea. No funder/sponsor had any role in the design and conduct of the study.
Author Contributions:
Jung-Sun Kim, MD and Ji-Yong Jang, MD had full access to all data in the study, and take responsibility for data integrity and data analysis accuracy.
Study concept and design:
All authors
Acquisition of data:
All authors
Analysis and interpretation of data:
All authors
Drafting of the manuscript:
Ji-Yong Jang, MD; Dong-Ho Shin, MD; Byoung-Kwon Lee, MD; and Jung-Sun Kim, MD
Critical revision of the manuscript for important intellectual content:
All authors
Statistical analysis:
Dong-Ho Shin, MD, MPH
Study supervision:
Yangsoo Jang, MD; Myeong-Ki Hong, MD.
Conflict of Interest
The authors have no conflicts of interest to disclose.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-19-0667
References
- 1.
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019; 40: 87–165.
- 2.
Eisenstein EL, Anstrom KJ, Kong DF, Shaw LK, Tuttle RH, Mark DB, et al. Clopidogrel use and long-term clinical outcomes after drug-eluting stent implantation. JAMA 2007; 297: 159–168.
- 3.
Raber L, Magro M, Stefanini GG, Kalesan B, van Domburg RT, Onuma Y, et al. Very late coronary stent thrombosis of a newer-generation everolimus-eluting stent compared with early-generation drug-eluting stents: A prospective cohort study. Circulation 2012; 125: 1110–1121.
- 4.
Palmerini T, Della Riva D, Benedetto U, Bacchi Reggiani L, Feres F, Abizaid A, et al. Three, six, or twelve months of dual antiplatelet therapy after DES implantation in patients with or without acute coronary syndromes: An individual patient data pairwise and network meta-analysis of six randomized trials and 11,473 patients. Eur Heart J 2017; 38: 1034–1043.
- 5.
Colombo A, Chieffo A, Frasheri A, Garbo R, Masotti-Centol M, Salvatella N, et al. Second-generation drug-eluting stent implantation followed by 6- versus 12-month dual antiplatelet therapy: The SECURITY randomized clinical trial. J Am Coll Cardiol 2014; 64: 2086–2097.
- 6.
Hong SJ, Kim BK, Shin DH, Nam CM, Kim JS, Ko YG, et al. Effect of intravascular ultrasound-guided vs. angiography-guided everolimus-eluting stent implantation: The IVUS-XPL randomized clinical trial. JAMA 2015; 314: 2155–2163.
- 7.
Kim BK, Hong MK, Shin DH, Nam CM, Kim JS, Ko YG, et al. A new strategy for discontinuation of dual antiplatelet therapy: The RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol 2012; 60: 1340–1348.
- 8.
Lee BK, Kim JS, Lee OH, Min PK, Yoon YW, Hong BK, et al. Safety of six-month dual antiplatelet therapy after second-generation drug-eluting stent implantation: OPTIMA-C randomised clinical trial and OCT substudy. EuroIntervention 2018; 13: 1923–1930.
- 9.
Gwon HC, Hahn JY, Park KW, Song YB, Chae IH, Lim DS, et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: The Efficacy of Xience/Promus Versus Cypher to Reduce Late Loss After Stenting (EXCELLENT) randomized, multicenter study. Circulation 2012; 125: 505–513.
- 10.
Yeh RW, Kereiakes DJ, Steg PG, Windecker S, Rinaldi MJ, Gershlick AH, et al. Benefits and risks of extended duration dual antiplatelet therapy after PCI in patients with and without acute myocardial infarction. J Am Coll Cardiol 2015; 5: 2211–2221.
- 11.
Costa F, Vranckx P, Leonardi S, Moscarella E, Ando G, Calabro P, et al. Impact of clinical presentation on ischemic and bleeding outcomes in patients receiving 6- or 24-month duration of dual-antiplatelet therapy after stent implantation: A pre-specified analysis from the PRODIGY (Prolonging Dual-Antiplatelet Treatment After Grading Stent-Induced Intimal Hyperplasia) trial. Eur Heart J 2015; 36: 1242–1251.
- 12.
Hahn JY, Song YB, Oh JH, Cho DK, Lee JB, Doh JH, et al. 6-month versus 12-month or longer dual antiplatelet therapy after percutaneous coronary intervention in patients with acute coronary syndrome (SMART-DATE): A randomized, open-label, non-inferiority trial. Lancet 2018; 391: 1274–1284.
- 13.
Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2018; 39: 213–260.
- 14.
Costa F, van Klaveren D, James S, Heg D, Raber L, Feres F, et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: A pooled analysis of individual-patient datasets from clinical trials. Lancet 2017; 389: 1025–1034.
- 15.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical endpoints in coronary stent trials: A case for standardized definitions. Circulation 2007; 115: 2344–2351.
- 16.
Stone GW, Abizaid A, Onuma Y, Seth A, Gao R, Ormiston J, et al. Effect of technique on outcomes following bioresorbable vascular scaffold implantation: Analysis from the ABSORB trials. J Am Coll Cardiol 2017; 70: 2863–2874.
- 17.
Giustino G, Chieffo A, Palmerini T, Valgimigli M, Feres F, Abizaid A, et al. Efficacy and safety of dual antiplatelet therapy after complex PCI. J Am Coll Cardiol 2016; 68: 1851–1864.
- 18.
Palmerini T, Della Riva D, Biondi-Zoccai G, Leon MB, Serruys PW, Smits PC, et al. Mortality Following nonemergent, uncomplicated target lesion revascularization after percutaneous coronary intervention: An individual patient data pooled analysis of 21 randomized trials and 32,524 patients. JACC Cardiovasc Interv 2018; 11: 892–902.
- 19.
Kupka D, Sibbing D. de-escalation of p2y12 receptor inhibitor therapy after acute coronary syndromes in patients undergoing percutaneous coronary intervention. Korean Circ J 2018; 48: 863–872.
- 20.
Costa F, Van Klaveren D, Feres F, James S, Räber L, Pilgrim T, et al. Dual antiplatelet therapy duration based on ischemic and bleeding risks after coronary stenting. J Am Coll Cardiol 2019; 73: 741–754.
- 21.
Mehran R, Baber U, Steg PG, Ariti C, Weisz G, Witzenbichler B, et al. Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (PARIS): 2 year results from a prospective observational study. Lancet 2013; 382: 1714–1722.
- 22.
Sherwood MW, Wang Y, Curtis JP, Peterson ED, Rao SV. Patterns and outcomes of red blood cell transfusion in patients undergoing percutaneous coronary intervention. JAMA 2014; 311: 836–843.
- 23.
Cesari F, Marcucci R, Caporale R, Paniccia R, Romano E, Gensini GF, et al. Relationship between high platelet turnover and platelet function in high-risk patients with coronary artery disease on dual antiplatelet therapy. Thromb Haemost 2008; 99: 930–935.
- 24.
Vranckx P, Valgimigli M, Juni P, Hamm C, Steg PG, Heg D, et al. Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs. aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months after implantation of a drug-eluting stent: A multicentre, open-label, randomised superiority trial. Lancet 2018; 392: 940–949.