Abstract
Background:
Despite the rapidly increasing attention being given to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, more commonly known as coronavirus disease 2019 (COVID-19), the relationship between cardiovascular disease and COVID-19 has not been fully described.
Methods and Results:
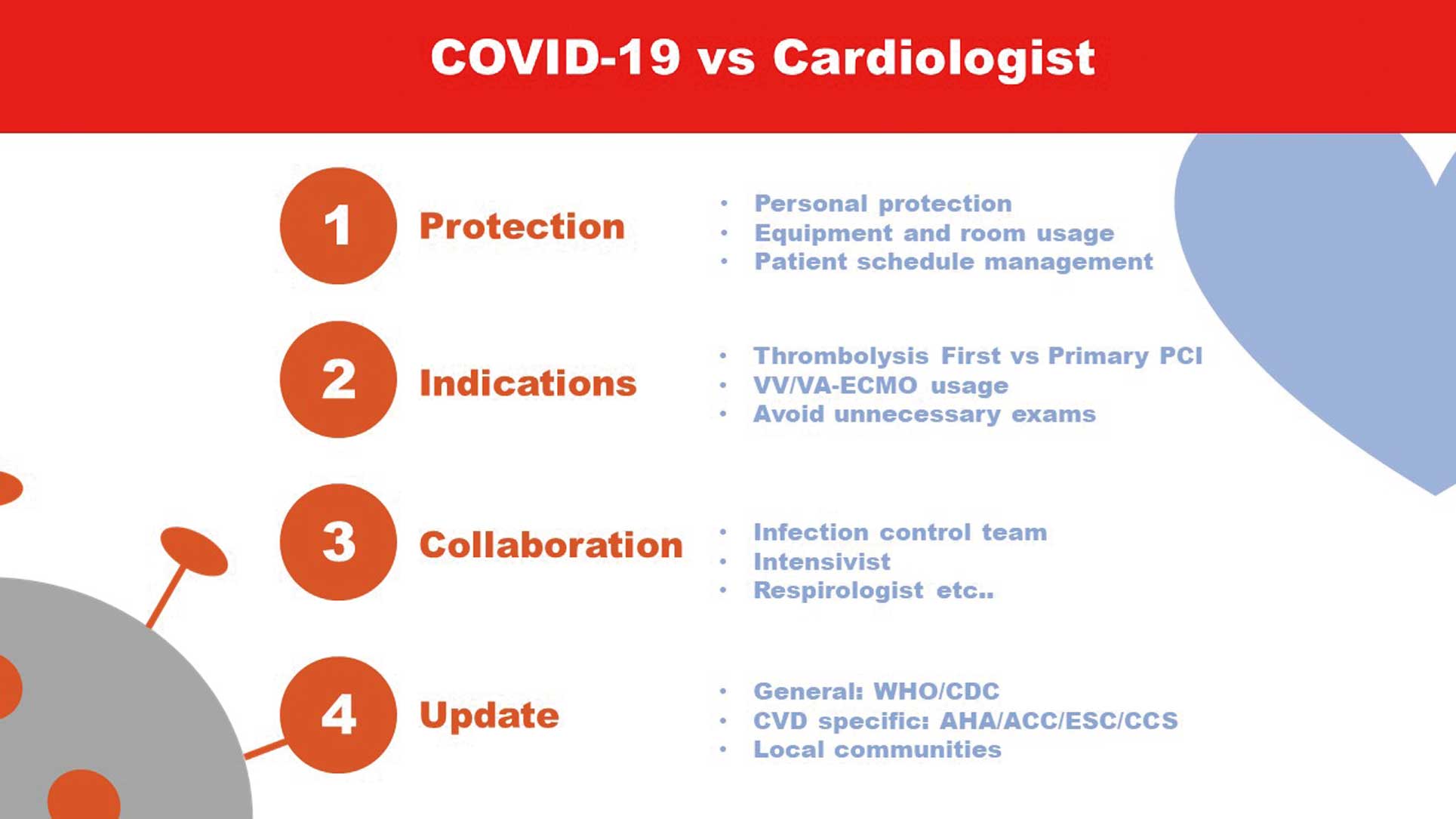
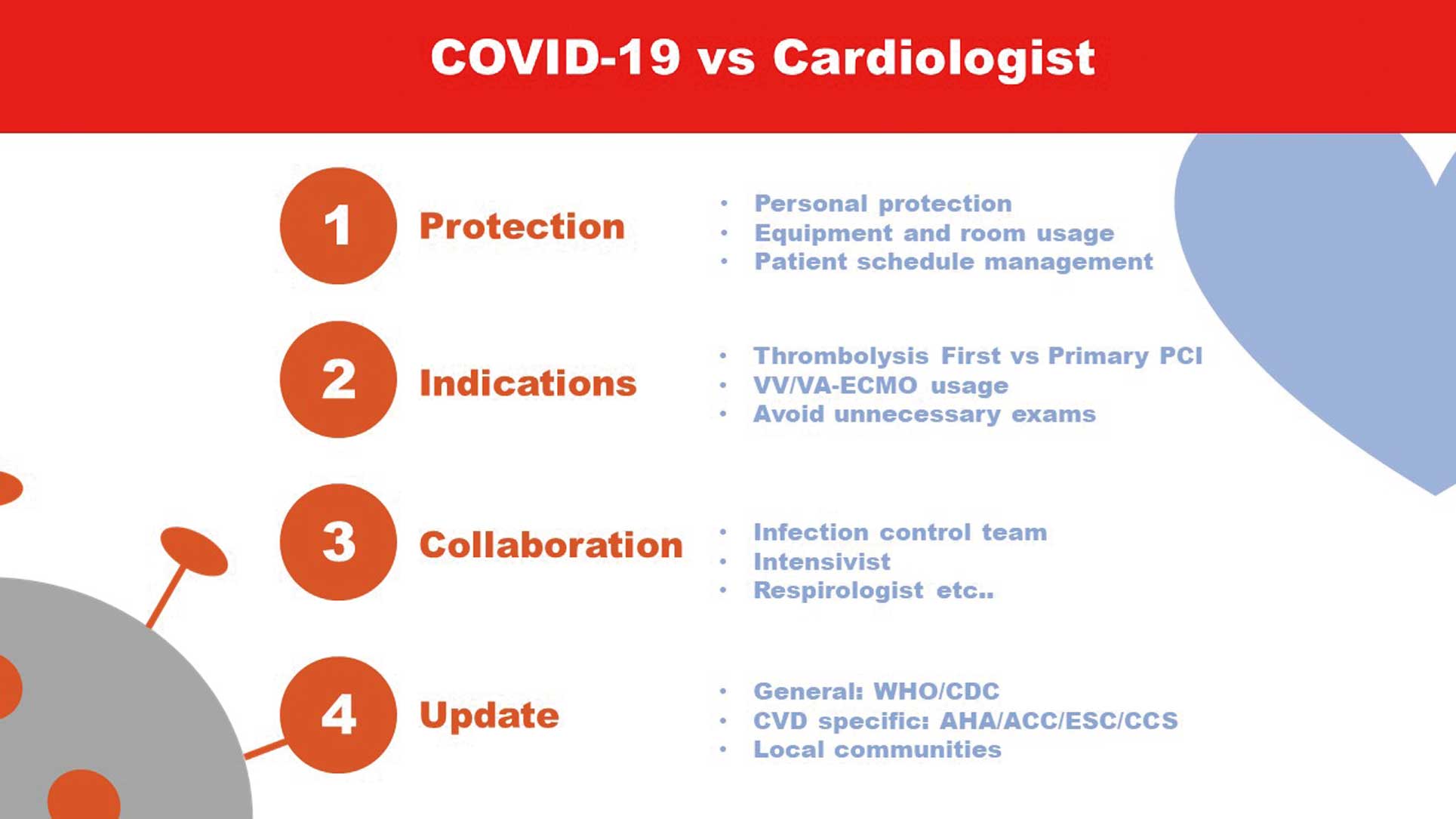
A systematic review was undertaken to summarize the important aspects of COVID-19 for cardiologists. Protection both for patients and healthcare providers, indication for treatments, collaboration with other departments and hospitals, and regular update of information are essentials to front COVID-19 patients.
Conclusions:
Because the chief manifestations of COVID-19 infection are respiratory and acute respiratory distress syndrome, cardiologists do not see infected patients directly. Cardiologists need to be better prepared regarding standard disinfection procedures, and be aware of the indications for extracorporeal membrane oxygenation and its use in the critical care setting.
As of March 7, 2020, 101,927 laboratory-confirmed cases of coronavirus disease 2019 (COVID-19) had been documented globally.1
Despite the rapidly increasing attention being given to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, more commonly known as COVID-19, the relationship between cardiovascular disease (CVD) and COVID-19 has not been fully described. A recent report from China briefly summarized the baseline characteristics of 72,314 clinical cases of COVID-19 and their outcomes.2
In that report, of 44,415 confirmed cases, 6,168 (13.8%) had severe disease. Of note, compared with an overall case fatality rate of 2.3% among all confirmed cases, the case fatality rate in patients with CVD was 10.5%.2
Guan et al reported more detailed clinical data on confirmed cases of COVID-19 that revealed that over one-fifth (23.7%) of patients had previous coexisting disorders (e.g., hypertension and diabetes) and this was associated with poor outcome.3
These results indicate that people with pre-existing comorbidities should be aware of the risk of COVID-19 and its associated complications. In this review we summarize the current understanding and key points for cardiologists to tackle COVID-19 and to support their preparedness. Before summarizing the dataset, we performed a systematic review, the results of which are given in
Supplementary File.
Pathophysiology of COVID-19 and Its Relationship With CVD
SARS-CoV-2 is a positive-strand RNA virus and is the seventh coronavirus that has been proven to infect humans. The genome of SARS-CoV-2 shares 75–80% identity with that of SARS-CoV and uses the same cell receptor, namely the angiotensin-converting enzyme 2 (ACE2) receptor, which has a crucial role in the cardiovascular and immune systems.4,5
Considering that SARS-CoV-2 binds to ACE2 receptors, some investigators have suggested that there may be a relationship between COVID-19 and hypertension treatments, such as angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs).6,7
However, the European Society of Hypertension has stated that the currently available data on COVID-19 infections do not support the differential use of renin–angiotensin system (RAS) blockers (ACEI or ARBs) in patients infected with COVID-19.8
Several studies of complete and partial autopsies of patients with Severe Acute Respiratory Syndrome (SARS) have reported that the predominant pathological finding is diffuse alveolar damage caused both by direct viral effects and immunopathogenetic factors.9
The main target organs of SARS, the lungs and intestines, have been widely investigated. In contrast, the pathology of SARS-CoV infection in CVDs has not been well described. Edema of both the myocardial stroma and vascular walls, as well as atrophy of cardiac muscle fibers, have been demonstrated as pathological features of SARS-CoV infection in the heart.9
Risk and Prognosis in the Overall Population and in Individuals With CVD
Several epidemiological studies have been published regarding COVID-19 and its severity and prognosis. One of these studies has reported that among 1,099 hospitalized patients with COVID-19, 15.7% were categorized as “severe” on admission.3
Compared with patients with non-severe disease, those with severe disease were older and had coexisting illnesses, including coronary artery disease (5.8%) and cerebrovascular disease (2.3%).3
In that dataset, 6.1% of patients met the primary composite endpoint (including 5.0% admitted to the intensive care unit [ICU], of whom 2.3% underwent invasive mechanical ventilation and 1.4% died). In a case series of 138 consecutive hospitalized patients with COVID-19, 26.1% required ICU care because of complications, including acute respiratory distress syndrome (ARDS; 61.1%), arrhythmia (44.4%), shock (30.6%), and acute cardiac injury (22.0%), as defined by abnormal elevation of serum cardiac biomarkers or new-onset abnormal electrocardiogram (ECG) and echocardiogram findings.10
Although the mechanism of myocardial injury has not been fully evaluated, Wei et al inferred plausible mechanisms, such as myocarditis directly caused by the virus, hemodynamic damage induced by hypoxia or shock, and an immune response or cytokine storm.11
Patients who required ICU care were reported to be older and to have coexisting illnesses, including hypertension (58.3%), diabetes (22.2%), CVD (25.0%), and cerebrovascular disease (16.7%).11
In addition, the overall mortality in that study was 4.3%, which is consistent with previous data. In the limited dataset from Hubei, the epicenter of the outbreak, the mortality rate was 11.7%,12
but this was considered to result from a lack of resources, and the study population was significantly biased. COVID-19 mortality is usually considered to be lower than that for SARS, but COVID-19 mortality is high in the elderly population.13
There are few studies regarding outcomes of COVID-19 infection in patients with CVD, but mortality in this population is due chiefly to multiorgan failure.14
Clinical Implications for Cardiologists
Currently, the cardiac manifestations in patients infected with COVID-19 are considered to be the following: myocardial injury, myocarditis, arrhythmia, venous thrombosis and heart failure.15,16
However, there is little clinical data available regarding these diseases in association with COVID-19. As noted in many reports, the chief manifestation of infection and exacerbation of illness is due to pneumonia and ARDS.17
Therefore, intensivists, respirologists, infectious disease specialists, and primary care physicians are at the frontline of this disease.18
Cardiologists may not directly encounter any patients suspected as being infected with COVID-19. However, considering the aforementioned high-risk characteristics of patients with CVD, cardiologists should be prepared to deal with these patients as consultants. The American College of Cardiology publishes a clinical bulletin, the ACC Clinical Bulletin COVID-19 Clinical Guidance For the CV Care Team, which is frequently updated.19
As stated in this bulletin, preparedness is crucial, especially regarding personal protective equipment (PPE) and the management of facilities and devices, including ECGs, echocardiograms, catheterization laboratories, and operating rooms. These instructions are both for the prevention of widespread disease and staff protection (Figure).20
The most up-to-date information regarding PPE is available online at the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) websites.21,22
Device management should also be considered when cardiologists see patients with COVID-19. In addition to using PPE, it is imperative that devices, including ultrasound equipment, are cleaned and disinfected. As reported by Kampf et al, many coronaviruses can persist on inanimate surfaces, such as metal, glass, or plastic, for up to 9 days, but they can be efficiently inactivated within 1 min by surface disinfection procedures with 62–71% ethanol, 0.5% hydrogen peroxide, or 0.1% sodium hypochlorite.23
Guidance on cleaning and disinfection procedures is also available online at the CDC and WHO websites, but usually requires further reference to manufacturers’ instructions, especially for the disinfection of ultrasound probes.24,25
Similar disinfection and prevention concepts should be applied to the clinical environment, including the ICU, catheterization room, and operating room.26
From early reports, if a patient (even a neonate) has shared a room with other patients before being identified as infected with COVID-19, all patients who shared a room with that person are considered to be isolated for at least 14 days unless SARS-CoV-2 infection is ruled out.27
Although only limited data are available regarding how to prepare cardiology equipment and facilities for managing patients with COVID-19, Si et al described their experiences with the perioperative management of acute aortic syndrome in patients with COVID-19.28
These considerations could be applied to the pericatheterization situation. Zeng et al recently advocated a routine diagnosis and treatment protocol for acute myocardial infarction in patients with suspected or confirmed COVID-19 infection.29
Recently, the American Society of Echocardiography published a statement on the protection of patients and echocardiography service providers during the COVID-19 outbreak, which is also informative for many ultrasonographers and cardiologists.30
Because there are many recommendations regarding COVID-19 and online resources (Table), following or developing policies in each hospital in consultation with departments of infectious diseases and infection control teams may be the best option for providing appropriate care for patients.
Table.
Examples of Online Resources From Major Cardiology Societies
| Society |
Summary and features |
URL |
| American College of Cardiology (ACC) |
| ACC’s COVID-19 Hub |
ACC’s COVID information platform including webinar
recordings and materials links and other resources
Webinar recordings of ACC and Chinese Cardiovascular
Association collaboration would be beneficial to overview
COVID-19-related cardiovascular problems |
https://www.acc.org/latest-in-cardiology/
features/accs-coronavirus-disease-2019
-covid-19-hub#sort=%40fcommonsortdate
90022%20descending |
ACC Clinical Bulletin
COVID-19 Clinical
Guidance for the CV
Care Team |
This is the first guidance for cardiologists; it was published
in February 2020 and is updated non-regularly |
https://www.acc.org/latest-in-cardiology/
features/~/media/Non-Clinical/Files-PDFs
-Excel-MS-Word-etc/2020/02/S20028-ACC
-Clinical-Bulletin-Coronavirus.pdf |
| American Society of Echocardiography (ASE) |
ASE Statement on
COVID-19 |
Statement describes how to perform echocardiography and
manage equipment |
https://www.asecho.org/ase-statement
-covid-19/ |
| American Heart Association (AHA) |
Coronavirus (COVID-19)
Resources |
Similar to the ACC’s COVID-19 Hub, but the AHA has
included more patient-friendly resources |
https://www.heart.org/en/about-us/
coronavirus-covid-19-resources |
| European Society of Cardiology (ESC) |
| COVID-19 and Cardiology |
Online platform including Insights From the Front Lines and
ESC COVID-19 Videos that feature many physicians and
their teams from European countries in clinical practice |
https://www.escardio.org/Education/COVID
-19-and-Cardiology |
ESC Council on
Hypertension Statement
on COVID-19 |
This statement recommends patients with hypertension
receive and continue treatment with ACEIs and ARBs
according to 2018 ESC/ESH guidelines despite COVID-19
infection |
https://www.escardio.org/Councils/Council
-on-Hypertension-(CHT)/News/position
-statement-of-the-esc-council-on-hyper
tension-on-ace-inhibitors-and-ang |
| Canadian Cardiovascular Society (CCS) |
Guidance from the CCS
COVID-19 Rapid
Response Team |
Similar to the ACC’s COVID-19 Hub, the CCS has also
included several webinar resources and guidance for
physicians, as well as Society messages to patients |
http://www.ccs.ca/en/ |
ACEIs, angiotensin-converting enzyme inhibitors; ARBs, angiotensin receptor blockers; COVID-19, coronavirus disease 2019; ESH, European Society of Hypertension.
Critical Care Patient Management
As noted above, chief management should be focused on respiratory diseases, including pneumonia and ARDS, which are usually managed by non-cardiologists. Yang et al retrospectively analyzed 52 critically ill adult patients with COVID-19.31
In that study population, 32 patients (61.5%) died at 28 days, which is comparable with previous coronavirus infections.26
From the cardiologist’s perspective, we should pay attention to the need for extracorporeal membrane oxygenation (ECMO) in this population. Because there is still debate surrounding the indication for ECMO for patients with COVID-19,32
the American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice guideline is neither for nor against the use of ECMO in patients with ARDS.33
Further investigations are needed into the scientific aspects of ECMO for COVID-19. Based on these limitations, resource allocation should be considered instead.34
The Italian College of Anesthesia, Analgesia, Resuscitation and Intensive Care (SIAARTI) published guidelines for physicians and other healthcare providers to refer to if they find themselves in the extraordinary situation in which there is a lack of appropriate medical resources.35,36
Cardiologists should also pay attention to resource allocation and share information among many hospitals within countries.
Future Perspectives and Conclusion
Information about COVID-19 is updated every hour. Confirmed COVID-19 cases are still increasing, with up to 2,477,426 cases reported globally on April 20, 2020. In order to share rapidly increasing clinical information, many COVID-19 research articles can be obtained free of charge, and preprint articles are also available on preprint servers, such as bioRxiv, medRxiv, and ChemRxiv, so that clinicians and researchers can access the latest information available worldwide.37
Under the current circumstances, preprints were not considered in our systematic review process; however, appropriate methods of searching and summarizing the rapidly growing amount of information need to be developed. In the future, we may be able to obtain updated information more smoothly.
The current coronavirus infection reminds us about the need to be prepared for a pandemic and the need for international collaboration. In particular, considering the low frequency of cardiovascular manifestations of COVID-19, we should actively gather information and share it quickly. Currently, we have no absolute treatment for this coronavirus; new treatments for COVID-19 are being studied in many ongoing trials.26
These treatments and ongoing scientific research will enhance and update our understanding of COVID-19.
Acknowledgments
We appreciate special assistance from Taro Inaba and Tomohiro Ogura, as well as the office staff of the Japanese Circulation Society, in the support of a COVID-19 team of the Japanese Circulation Society.
Disclosures
I.K., K.N. are members of
Circulation Journal
’ Editorial Team. The other authors report no potential conflicts of interest.
IRB Information
This study was granted an exemption from requiring ethics approval by St. Luke’s International Hospital.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-20-0302
References
- 1.
World Health Organization. Coronavirus disease 2019 (COVID-19) situation report – 47. https://web.archive.org/web/20200308150245/https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200307-sitrep-47-covid-19.pdf (accessed April 21, 2020).
- 2.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA, doi:10.1001/jama.2020.2648.
- 3.
Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med, doi:10.1056/NEJMoa2002032.
- 4.
Turner AJ, Hiscox JA, Hooper NM. ACE2: From vasopeptidase to SARS virus receptor. Trends Pharmacol Sci 2004; 25: 291–294.
- 5.
Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, doi:10.1038/s41586-020-2012-7.
- 6.
Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res, doi:10.1002/ddr.21656.
- 7.
Kickbusch I, Leung G. Response to the emerging novel coronavirus outbreak. BMJ 2020; 368: m406.
- 8.
European Society of Hypertension (ESH). ESH letter COVID-19. https://www.eshonline.org/spotlights/esh-stabtement-on-covid-19-2/ (accessed March 8, 2020).
- 9.
Gu J, Korteweg C. Pathology and pathogenesis of severe acute respiratory syndrome. Am J Pathol 2007; 170: 1136–1147.
- 10.
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA, doi:10.1001/jama.2020.1585.
- 11.
Wei ZY, Qian HY. [Myocardial injury in patients with COVID-19 pneumonia.] Zhonghua Xin Xue Guan Bing Za Zhi (in Chinese), doi:10.3760/cma.j.issn.cn112148-20200220–00106.
- 12.
Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl), doi:10.1097/cm9.0000000000000744.
- 13.
Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg 2020; 76: 71–76.
- 14.
Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med, doi:10.3390/jcm9020575.
- 15.
Tan ZC, Fu LH, Wang DD, Hong K. Cardiac manifestations of patients with COVID-19 pneumonia and related treatment recommendations. Zhonghua Xin Xue Guan Bing Za Zhi (in Chinese), doi:10.3760/cma.j.issn.cn112148-20200213-00077.
- 16.
Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Bondi-Zoccai G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol, doi:10.1016/j.jacc.2020.03.031.
- 17.
Murthy S, Gomersall CD, Fowler RA. Care for critically ill patients with COVID-19. JAMA, doi:10.1001/jama.2020.3633.
- 18.
Bouadma L, Lescure F-X, Lucet J-C, Yazdanpanah Y, Timsit J-F. Severe SARS-CoV-2 infections: Practical considerations and management strategy for intensivists. Intensive Care Med, doi:10.1007/s00134-020-05967-x.
- 19.
Mullen B. ACC clinical bulletin COVID-19 clinical guidance for the CV care team. https://www.acc.org/~/media/665AFA1E710B4B3293138D14BE8D1213.pdf (accessed March 8, 2020).
- 20.
World Health Organization (WHO). Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. Interim guidance. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 (accessed March 8, 2020).
- 21.
World Health Organization (WHO). Personal protective equipment. https://www.who.int/medical_devices/meddev_ppe/en/ (accessed March 9, 2020).
- 22.
Centers for Disease Control and Prevention (CDC). Protecting healthcare personnel. https://www.cdc.gov/hai/prevent/ppe.html (accessed March 8, 2020).
- 23.
Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020; 104: 246–251.
- 24.
Centers for Disease Control and Prevention (CDC). Interim infection prevention and control recommendations for patients with confirmed coronavirus disease 2019 (COVID-19) or persons under investigation for COVID-19 in healthcare settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html (accessed March 8, 2020).
- 25.
World Health Organization and Pan American Health Organization. Decontamination and reprocessing of medical devices for health-care facilities. https://www.who.int/infection-prevention/publications/decontamination/en/ (accessed March 8, 2020).
- 26.
Arabi YM, Murthy S, Webb S. COVID-19: A novel coronavirus and a novel challenge for critical care. Intensive Care Med, doi:10.1007/s00134-020-05955-1.
- 27.
Wang J, Qi H, Bao L, Li F, Shi Y. A contingency plan for the management of the 2019 novel coronavirus outbreak in neonatal intensive care units. Lancet Child Adolesc Health, doi:10.1016/s2352-4642(20)30040-7.
- 28.
Si Y, Sun XF, Zhong M, Yue JN, Fu WG. [Countermeasures and treatment for aortic acute syndrome with novel coronavirus pneumonia.] Zhonghua Wai Ke Za Zhi (in Chinese), doi:10.3760/cma.j.issn.0529-5815.2020.0002.
- 29.
Zeng J, Huang J, Pan L. How to balance acute myocardial infarction and COVID-19: The protocols from Sichuan Provincial People’s Hospital. Intensive Care Med, doi:10.1007/s00134-020-05993-9.
- 30.
American Society of Echocardiography (ASE). ASE Statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak. https://www.asecho.org/wp-content/uploads/2020/03/ASE-COVID-Statement-FINAL-1.pdf (accessed April 16, 2020).
- 31.
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med, doi:10.1016/s2213-2600(20)30079-5.
- 32.
Rochwerg B, Alhazzani W, Sevransky JE. Extracorporeal membrane oxygenation in acute respiratory distress syndrome: More research is needed. Crit Care Med 2019; 47: 118–120.
- 33.
Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: Mechanical ventilation in adult patients with acute respiratory distress syndrome [published erratum appears in Am J Respir Crit Care Med 2017; 195: 1540]. Am J Respir Crit Care Med 2017; 195: 1253–1263.
- 34.
MacLaren G, Fisher D, Brodie D. Preparing for the most critically ill patients with COVID-19: The potential role of extracorporeal membrane oxygenation. JAMA, doi:10.1001/jama.2020.2342.
- 35.
Mounk Y. The extraordinary decisions facing Italian doctors. There are now simply too many patients for each one of them to receive adequate care. The Atlantic 11 March 2020. https://www.theatlantic.com/ideas/archive/2020/03/who-gets-hospital-bed/607807/ (accessed 8 March 2020).
- 36.
SIAARTI. Raccomandazioni di etica clinica per l’ammissione atrattamenti intensivie per la loro sospensione, in condizioni eccezionalidi squilibrio tra necessitàe risorse disponibili. https://www.siaarti.it/SiteAssets/News/COVID19%20-%20documenti%20SIAARTI/SIAARTI%20-%20Covid19%20-%20Raccomandazioni%20di%20etica%20clinica.pdf (accessed March 8, 2020).
- 37.
Stoye E. Coronavirus papers appearing rapidly as researchers respond to outbreak. Nature News Round-up. https://www.nature.com/articles/d41586-020-00270-7 (accessed March 8, 2020).