2021 年 85 巻 11 号 p. 1972-1980
2021 年 85 巻 11 号 p. 1972-1980
Background: Percutaneous coronary intervention (PCI) for coronary bifurcation lesions using the 2-stent strategy remains a challenging procedure for interventionalists because of the higher incidence of in-stent restenosis (ISR) and adverse events. ISR predictors in patients treated with newer-generation everolimus-eluting stents (EES) and the 2-stent strategy remain unknown. Hence, we aimed to evaluate the 1-year clinical and angiographic outcomes of non-left main trunk (LMT) bifurcation lesions treated with the 2-stent strategy using newer-generation EES.
Methods and Results: The study sample consisted of 262 non-LMT bifurcation lesions treated using culotte or T-stenting with EES between 2010 and 2018. One-year post-procedural angiographic and clinical examinations were conducted in 208 (79.4%) and 260 (99.2%) lesions, respectively. The primary outcome measure was the 1-year post-procedural ISR rate, which was found to be 15.9%. Independent predictors of 1-year post-procedural ISR were long side branch lesions (adjusted odds ratio [aOR] 2.31; 95% confidence interval [CI] 1.02–5.23; P=0.04) and 3-link EES implantation (aOR 2.45; 95% CI 1.07–5.61; P=0.03). The 1-year cumulative incidence of target lesion revascularization was 3.5%.
Conclusions: The 1-year clinical outcomes of non-LMT bifurcation lesions treated with the 2-stent strategy using EES were acceptable. Long side branch lesions and lesions treated with 3-link EES were independent predictors of 1-year post-procedural ISR.
Percutaneous coronary intervention (PCI) for coronary bifurcation lesions using the 2-stent strategy remains a challenging procedure for interventionalists because of the higher incidence of in-stent restenosis (ISR) and adverse events.1–3 However, there are certain situations wherein the 2-stent strategy should be considered, such as the presence of true bifurcation lesions with a side branch (SB) dominating a large area of the myocardium. Previous studies have revealed that the SB ostium was the major site of restenosis that was treated with a 2-stent strategy.4,5 The major reasons for restenosis at the bifurcation site were suggested to be stent jails of the SB ostium and malapposition of the bifurcation area;6–8 however, ISR predictors in lesions treated with newer-generation everolimus-eluting stents (EES) remain unknown. Hence, the aim of this study was to evaluate the angiographic and clinical outcomes of non-left main trunk (LMT) bifurcation lesions treated using the 2-stent strategy with newer-generation EES.
Editorial p 1981
Data for 256 consecutive patients (262 lesions) treated at Kurashiki Central Hospital between 2010 and 2018 using the 2-stent strategy with EES for non-LMT bifurcation lesions were assessed retrospectively. The types of EES implanted were the Xience® (Abbot Vascular, Santa Clara, CA, USA) and the Promus ElementTM (Boston Scientific, Natick, MA, USA). Cases of hybrid stenting using both 2- and 3-link EES were excluded. The decision-making process for 2-stent strategies for patients with bifurcation lesions in Kurashiki Central Hospital is as follows: when the main branch has a relatively larger SB (≥2.5 mm in diameter) that exhibits severe stenosis, a longer lesion length (≥5 mm), and has a large territory, a 2-stent strategy is generally planned. When these criteria are not fulfilled, a provisional 1-stent strategy is selected, even in the case of true bifurcation lesions. When an ischemic condition, such as SB dissection or limited flow due to significant stenosis, occur in the SB after stenting for the main branch, a provisional 2-stent strategy is performed. Final kissing balloon inflation is mandatory for 2-stent strategies .
All procedures were performed in accordance with the Declaration of Helsinki. Informed consent was provided by all patients for both the procedure and subsequent data collection and analysis for research purposes. The study was approved by the Institutional Review Board of Kurashiki Central Hospital (Reference no. 3535).
Outcome Measures and DefinitionsThe primary outcome measure was defined as ISR within 1 year after the procedure. Other outcome measures were major adverse cardiac events (MACE), all-cause death, cardiac death, non-procedural myocardial infarction (MI), definite or probable stent thrombosis (ST), target lesion revascularization (TLR), and bifurcation site restenosis within 1 year after the procedure. Angiographic follow-up was scheduled 8 months after the procedure. The angiographic outcomes measured were ISR and bifurcation site restenosis. Clinical follow-up was censored by death and loss to follow-up within 1 year after the procedure.
ISR was defined as angiographic diameter stenosis ≥50%. MACE was defined as a composite of cardiac death, non-procedural MI, definite or probable ST, and TLR. Cardiac death included death from cardiac causes, unwitnessed death, death of unknown cause, and all deaths related to concomitant treatment. Non-procedural MI was defined as infarction related to ischemia caused by a primary coronary event coupled with elevated cardiac enzymes (troponin or creatine kinase-MB fraction) greater than the upper limit of normal, except MI within 48 h after the procedure. ST was defined as definite or probable ST according to the Academic Research Consortium definitions.9 TLR was defined as any repeat PCI or coronary artery bypass surgery for either: (1) angiographic diameter stenosis ≥50% with symptoms or objective signs of ischemia; or (2) angiographic diameter stenosis ≥70% without symptoms or objective signs of ischemia.
The 2-stent strategy consisted of the deployment of at least 1 stent in both the main branch and SB of a bifurcation lesion. The main branch, in terms of culotte stenting, was defined as the vessel with the larger diameter. In T-stenting, the main branch was defined as the vessel in which a stent was implanted from the proximal stem. In this study, both culotte and T-stenting were used. A long lesion was defined as one measuring ≥20 mm according to the modified American College of Cardiology/American Heart Association lesion morphology criteria.10 Residual restenosis was defined as angiographic diameter stenosis >20% because a previous study revealed that residual restenosis >20% was a risk factor for TLR.11 High balloon inflation pressure in the main branch and SB was defined as a pressure higher than the mean pressure.
Quantitative Coronary AngiographyFor quantitative coronary angiography (QCA), angiograms obtained at baseline, on completion of the intervention, and during the 8-month follow-up were independently analyzed by 2 experienced observers, who were blinded to patients’ clinical characteristics, using the QCA cardiovascular measurement system (CMS; Medis Medical Imaging Systems, Leiden, Netherlands). Bifurcation lesions were defined as main branch lesions in the main branch located between the proximal stem and the distal main branch, with boundaries defined by the segments 5 mm proximal and distal to the stent. SB lesions were those located between the bifurcation carina to the distal SB, with boundaries defined by the carina and the segment 5 mm distal to the stent. The 2-part measurement of bifurcation lesions was performed beginning with the main branch (first part) and ending with the SB (second part). Bifurcation site restenosis was defined as restenosis within 5 mm from a stent-implanted bifurcation lesion in both the main branch and SB. Acute gain was defined as the minimum immediate post-procedural lumen diameter minus the minimum preprocedural lumen diameter.
Statistical AnalysisAll statistical analyses were performed used IBM SPSS Statistics 23 (IBM Corp., Armonk, NY, USA). Discrete variables are reported as counts (percentages) and continuous variables are reported as the mean±SD. For discrete variables, the significance of between-group differences was tested using the χ2 test or Fisher’s exact test.
Predictors of ISR were analyzed using a multivariate logistic regression model. Variables with P<0.05 in the univariate models were selected for multivariate logistic regression. Stepwise multivariate logistic regression analysis was used to obtain the final model to identify independent variables that were predictors of ISR, with results expressed as odds ratios (ORs) and 95% confidence interval (CIs). The cumulative incidence of clinical events was estimated by the Kaplan-Meier method and compared using the log-rank test.
In the lesion-based analysis, multiple lesions in 1 patient treated by the 2-stent strategy were counted on a lesion-by-lesion basis for statistical analysis.
In all cases, 2-tailed P<0.05 was considered significant.
Baseline patient, lesion, and procedural characteristics are summarized in Table 1. The mean age of patients was 69.5 years. The most common target vessel in the bifurcation lesions was the left anterior descending artery and its diagonal branch (63.0%). Nearly all lesions (94.3%) were true bifurcation lesions. Culotte and T-stenting were used in 77.1% and 22.9% of cases, respectively. The mean pressure in the main branch and SB was 18.1 and 13.3 atm, respectively.
| Patient characteristics | |
| Age (years) | 69.5±11.1 |
| Age ≥80 years | 50 (19.1) |
| Male sex | 206 (78.6) |
| Hypertension | 192 (73.3) |
| Diabetes | 110 (42.0) |
| Insulin-treated diabetes | 24 (9.2) |
| Dyslipidemia | 182 (69.5) |
| History of smoking | 176 (67.2) |
| eGFR (mL/min/1.73 m2) | 64.2±25.7 |
| HD | 14 (5.3) |
| eGFR ≤60 mL/min/1.73 m2 and no HD | 70 (26.7) |
| Previous PCI | 92 (35.1) |
| Previous MI | 93 (35.5) |
| Previous CABG | 8 (3.1) |
| Peripheral vascular disease | 11 (4.2) |
| Lesion characteristics | |
| Target lesion | |
| LAD | 165 (63.0) |
| LCX | 55 (21.0) |
| RCA | 42 (16.0) |
| True bifurcation | 247 (94.3) |
| 1,1,1 | 180 (68.7) |
| 1,0,1 | 13 (5.0) |
| 1,1,0 | 5 (1.9) |
| 0,1,1 | 54 (20.6) |
| 1,0,0 | 4 (1.5) |
| 0,1,0 | 3 (1.1) |
| 0,0,1 | 3 (1.1) |
| CTO lesion | 35 (13.4) |
| ISR lesion | 8 (3.1) |
| ACS | 94 (35.9) |
| Procedural characteristics | |
| Rotablator use | 14 (5.3) |
| IVUS assessment | 171 (65.3) |
| Two-stent strategy | |
| Culotte stenting | 202 (77.1) |
| T-stenting | 60 (22.9) |
| Planned 2 stenting | 142 (54.2) |
| Final kissing balloon inflation | 260 (99.2) |
| POT | 102 (38.9) |
| Main branch | |
| Multiple stents | 76 (29.0) |
| Stent size (mm) | 2.8±0.4 |
| Stent length (mm) | 34.2±15.0 |
| Non-compliant balloon use | 244 (93.1) |
| Maximum inflation pressure (atm) | 18.1±5.6 |
| Side branch | |
| Multiple stents | 34 (13.0) |
| Stent size (mm) | 2.5±0.2 |
| Stent length (mm) | 23.0±11.5 |
| Non-compliant balloon use | 175 (66.8) |
| Maximum inflation pressure (atm) | 13.3±4.9 |
| Quantitative coronary angiographic analysis | |
| Preprocedural | |
| Main branch | |
| Reference diameter (mm) | 2.8±0.4 |
| Minimal lumen diameter (mm) | 0.7±0.6 |
| Percent diameter stenosis (%) | 75.3±20.1 |
| Lesion length (mm) | 25.3±12.6 |
| Side branch | |
| Reference diameter (mm) | 2.4±0.4 |
| Minimal lumen diameter (mm) | 0.6±0.4 |
| % Diameter stenosis | 72.8±18.6 |
| Lesion length (mm) | 16.4±8.8 |
| Post-procedural | |
| Main branch | |
| Minimal lumen diameter (mm) | 2.5±0.4 |
| % Diameter stenosis | 16.1±9.3 |
| Acute gain (mm) | 1.8±0.7 |
| Side branch | |
| Minimal lumen diameter (mm) | 2.1±0.3 |
| % Diameter stenosis | 19.6±10.5 |
| Acute gain (mm) | 1.4±0.5 |
| Medication | |
| Aspirin | 260 (99.2) |
| Clopidogrel | 225 (85.9) |
| Prasugrel | 29 (11.1) |
| Other antiplatelet drug | 10 (4.8) |
| Any DAPT | 262 (100) |
| Oral anticoagulation | 28 (10.7) |
| Statin | 224 (85.5) |
| β-blocker | 116 (44.3) |
| ACEI/ARB | 174 (66.4) |
| Calcium channel blocker | 86 (32.8) |
| Nitric acid medicine | 108 (41.2) |
| Proton pump inhibitor | 189 (72.1) |
Data are expressed as n (%) or as the mean±SD. ACEI, angiotensin-converting enzyme inhibitor; ACS, acute coronary syndrome; ARB, angiotensin II receptor blocker; CABG, coronary artery bypass grafting; CTO, chronic total occlusion; DAPT, dual antiplatelet therapy; eGFR, estimated glomerular filtration rate; HD, hemodialysis ; ISR, in-stent restenosis; IVUS, intravascular ultrasound; LAD, left anterior descending artery; LCX, left circumflex artery; MI, myocardial infection; PCI, percutaneous coronary intervention; POT, proximal optimization technique; RCA, right coronary artery.
The 1-year post-procedural angiographic follow-up rate was 79.4% (Figure 1). The ISR rate within 1 year, the primary outcome measure, was 15.9% (33/208 lesions). The most frequent location of the ISR was in the SB bifurcation site (Table 2). The 1-year post-procedural clinical follow-up rate was 99.6% (Figure 1). The 1-year cumulative incidence of TLR was 3.5% (Figure 2). The incidence of other clinical outcome measures was 5.0% for MACE, 2.7% for all-cause death, 1.2% for cardiac death, 1.9% for non-procedural MI, and 1.5% for definite or probable ST (Table 3). The 4 ST cases are presented in Supplementary Table 1. The incidence of ST was numerically lower in patients undergoing than not undergoing intravascular imaging (1.2% [2/171] vs. 2.2% [2/91], respectively), but the difference did not reach statistical significance (P=0.58).

Study flow chart. EES, everolimus-eluting stent.
| No. events (%) | |
|---|---|
| Angiographic outcomes | |
| In-stent restenosis | 33 (15.9) |
| Restenosis at the bifurcation | 24 (11.5) |
| Restenosis location | |
| Proximal stem | 1 (0.5) |
| Bifurcation in MB | 6 (2.9) |
| Distal or edge in MB | 3 (1.4) |
| Bifurcation in SB | 18 (8.7) |
| Distal or edge in SB | 9 (4.3) |
MB, main branch; SB, side branch.

Cumulative incidence of target lesion revascularization (TLR).
| No. events (%) | |
|---|---|
| Clinical and angiographic outcomes | |
| MACE | 13 (5.0) |
| All-cause death | 7 (2.7) |
| Cardiac death | 3 (1.2) |
| Non-procedural MI | 5 (1.9) |
| Definite/probable ST | 4 (1.5) |
| TLR | 9 (3.5) |
Major adverse cardiac events (MACE) were defined as the composite of cardiac death, non-procedural myocardial infarction (MI), definite/probable stent thrombosis (ST), and target lesion revascularization (TLR).
In the univariate analysis, the 1-year post-procedural risk factors for ISR were previous PCI, non-acute coronary syndrome, long SB lesion, main branch residual restenosis, maximum balloon pressure in the SB ≥14 atm, and 3-link EES implantation (Table 4). Multivariate analysis showed that long SB lesions (adjusted [a] OR 2.31; 95% CI 1.02–5.23; P=0.04) and lesions with a 3-link EES (aOR 2.45; 95% CI 1.07–5.61; P=0.03) were independent predictors of ISR 1 year after the procedure (Figure 3). Long SB lesions were predictive of ISR, whereas long main branch lesions were not (Table 4).
| Ratio of factors | Univariate analysis | |||
|---|---|---|---|---|
| ISR− (n=175) | ISR+ (n=33) | Odds ratio | P value | |
| Patient characteristics | ||||
| Age ≥80 years | 29 (16.6) | 6 (18.2) | 1.12 | 0.82 |
| Male sex | 140 (80.0) | 28 (84.8) | 1.40 | 0.64 |
| Hypertension | 125 (71.4) | 27 (81.8) | 1.80 | 0.22 |
| Diabetes | 66 (37.7) | 13 (39.7) | 1.07 | 0.86 |
| Insulin-treated diabetes | 12 (6.9) | 3 (9.1) | 1.36 | 0.71 |
| Dyslipidemia | 124 (70.9) | 27 (81.8) | 1.85 | 0.29 |
| History of smoking | 121 (69.1) | 23 (69.7) | 1.03 | 0.95 |
| HD | 4 (2.3) | 1 (3.0) | 1.34 | 0.58 |
| eGFR ≤60 mL/min/1.73 m2 and no HD | 42 (24.0) | 9 (27.3) | 1.19 | 0.69 |
| Previous PCI | 53 (30.3) | 17 (51.5) | 2.45 | 0.02 |
| Previous MI | 55 (31.4) | 13 (39.4) | 1.42 | 0.37 |
| Previous CABG | 6 (3.4) | 1 (3.0) | 0.88 | 1.00 |
| Peripheral vascular disease | 6 (3.4) | 1 (3.0) | 0.88 | 1.00 |
| Lesion characteristics | ||||
| Target lesion | ||||
| LAD | 112 (64.0) | 18 (54.5) | 0.68 | 0.30 |
| LCX | 36 (20.6) | 11 (33.3) | 1.93 | 0.11 |
| RCA | 27 (15.4) | 4 (12.1) | 0.76 | 0.63 |
| True bifurcation | 165 (94.3) | 30 (90.9) | 0.61 | 0.44 |
| CTO lesion | 21 (12.0) | 4 (12.1) | 1.01 | 1.00 |
| ISR lesion | 5 (2.9) | 1 (3.0) | 1.06 | 1.00 |
| ACS | 74 (42.3) | 7 (21.2) | 0.37 | 0.02 |
| Main branch | ||||
| Reference diameter ≤2.5 mm | 36 (20.6) | 11 (33.3) | 1.93 | 0.11 |
| Lesion length ≥20 mm | 100 (57.1) | 24 (72.7) | 2.00 | 0.09 |
| Side branch | ||||
| Reference diameter ≤2.5 mm | 112 (64.0) | 23 (69.7) | 1.29 | 0.53 |
| Lesion length ≥20 mm | 51 (29.1) | 16 (48.5) | 2.29 | 0.03 |
| Procedural characteristics | ||||
| Rotablator use | 6 (3.4) | 1 (3.3) | 0.88 | 0.91 |
| IVUS assessment | 109 (62.3) | 23 (69.7) | 1.39 | 0.42 |
| Culotte stenting | 135 (77.1) | 27 (81.8) | 1.33 | 0.55 |
| Planned 2 stenting | 92 (52.6) | 20 (60.6) | 1.39 | 0.40 |
| Final kissing inflation | 174 (99.4) | 32 (97.0) | 0.45 | 0.18 |
| POT | 68 (38.4) | 10 (30.3) | 0.70 | 0.38 |
| 3-link EES: Xience | 68 (38.9) | 20 (60.6) | 2.42 | 0.02 |
| Main branch | ||||
| Multiple stent | 45 (25.7) | 14 (42.4) | 2.13 | 0.05 |
| Stent size ≤2.5 mm | 75 (42.9) | 17 (51.5) | 1.42 | 0.36 |
| Stent length ≥20 mm | 150 (85.7) | 30 (90.9) | 1.67 | 0.58 |
| Residual stenosis ≥20% | 20 (12.7) | 13 (25.5) | 2.34 | 0.03 |
| Non-compliant balloon use | 163 (93.1) | 30 (90.9) | 0.74 | 0.71 |
| High-pressure balloon inflation | 101 (57.7) | 20 (60.6) | 1.13 | 0.85 |
| Side branch | ||||
| Multiple stent | 24 (13.7) | 3 (9.1) | 0.63 | 0.58 |
| Stent size ≤2.5 mm | 155 (88.6) | 28 (84.8) | 0.72 | 0.56 |
| Stent length ≥20 mm | 89 (50.9) | 22 (66.7) | 1.93 | 0.10 |
| Residual stenosis ≥20% | 16 (13.7) | 17 (18.7) | 1.45 | 0.33 |
| Non-compliant balloon use | 114 (65.1) | 22 (66.7) | 1.07 | 0.87 |
| High-pressure balloon inflation | 74 (42.2) | 7 (26.9) | 0.37 | 0.03 |
| Medication | ||||
| Aspirin | 173 (98.9) | 33 (100) | 1.19 | 0.54 |
| Clopidogrel | 152 (86.9) | 27 (81.8) | 0.68 | 0.44 |
| Prasugrel | 21 (12.0) | 3 (9.1) | 0.73 | 0.63 |
| Other antiplatelet drug | 4 (1.1) | 3 (9.1) | 4.28 | 0.08 |
| Oral anticoagulation | 17 (9.7) | 0 (0.0) | 0.83 | 0.08 |
| Statin | 152 (86.9) | 30 (90.9) | 1.51 | 0.52 |
| β-blocker | 80 (45.7) | 10 (30.3) | 0.52 | 0.10 |
| ACEI/ARB | 118 (67.4) | 20 (60.6) | 0.74 | 0.45 |
| Calcium channel blocker | 55 (31.4) | 11 (33.3) | 1.09 | 0.83 |
| Nitric acid medicine | 72 (41.1) | 17 (51.5) | 1.52 | 0.27 |
| Proton pump inhibitor | 133 (76.0) | 23 (69.7) | 0.73 | 0.44 |
Unless indicated otherwise, data are presented as n (%). EES, everolimus-eluting stent. Other abbreviations as in Table 1.

Predictors of in-stent restenosis (ISR) within 1 year after the procedure (multivariate analysis). ACS, acute coronary syndrome; CI, confidence interval; EES, everolimus-eluting stent; MB, main branch; SB, side branch; PCI, percutaneous coronary intervention.
The baseline characteristics of 3- and 2-link EES groups were shown in Supplemetary Table 2. There was no significant difference between the 3- and 2-link EES groups in terms of the 1-year cumulative incidence of TLR (Figure 4A). The 1-year post-procedural ISR rates in the 3- and 2-link groups were 22.7% (20/88 lesions) and 10.8% (13/120 lesions), respectively (P=0.02), and the rates of bifurcation site restenosis were 18.2% (16/88 lesions) and 6.7% (8/120 lesions), respectively (P=0.01). There was also a significant difference in bifurcation site restenosis rates of the SB between the 3- and 2-link EES groups (14.5% [12/88 lesions] and 5.0% [6/120 lesions], respectively; P=0.03). However, the rates of restenosis in other portions after the use of the 2-stent strategy were similar between the 3- and 2-link EES groups (Figure 4B,C; Table 3).
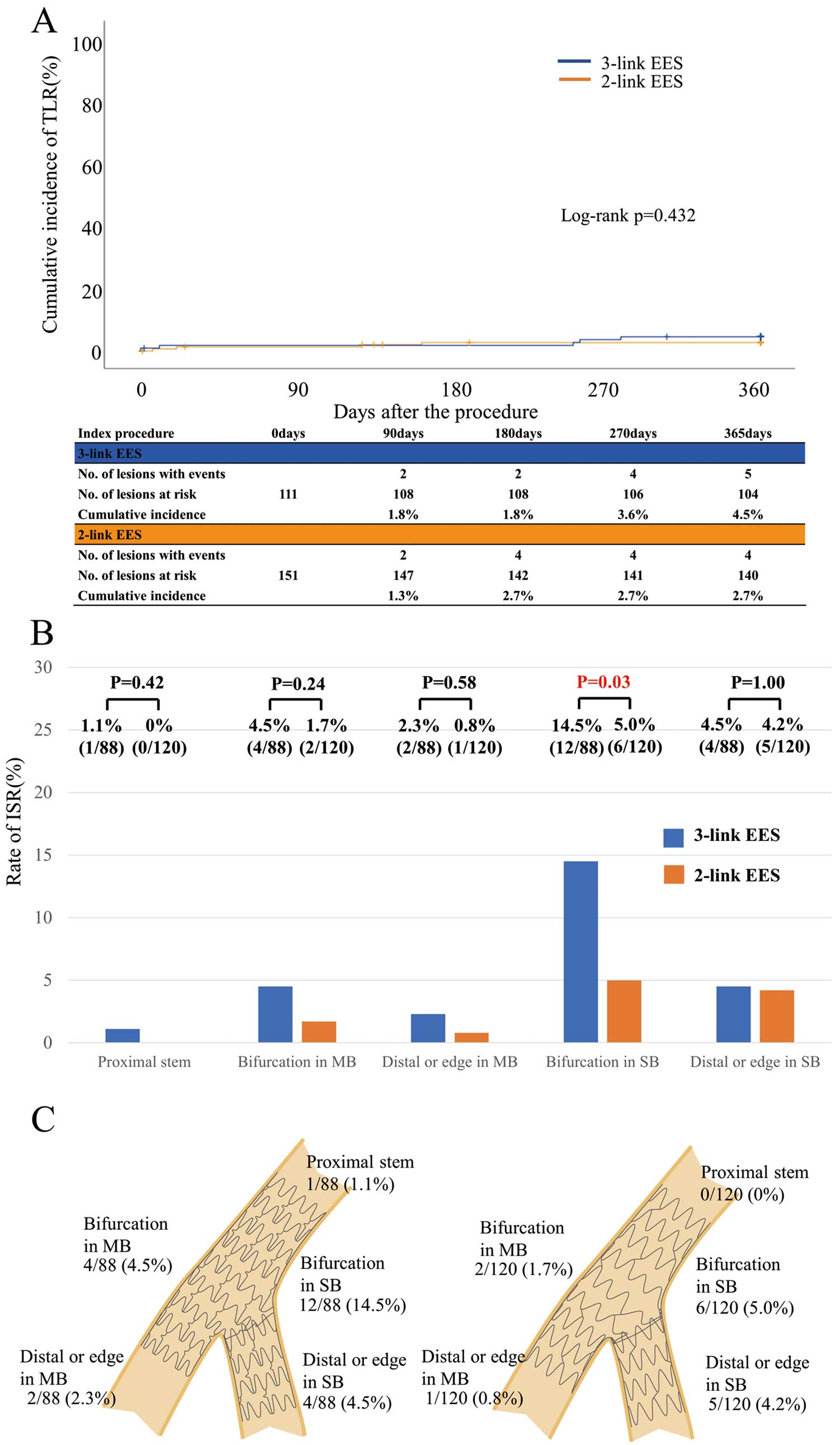
(A) Cumulative incidence of target lesion revascularization (TLR) in 3- and 2-link everolimus-eluting stents (EES), (B) in-stent restenosis (ISR) rates according to location for 3- and 2-link EES, and (C) restenosis location for 3- and 2-link EES. MB, main branch; SB, side branch.
There was no significant difference between the long and non-long lesions in the SB groups in terms of the 1-year cumulative incidence of TLR (Supplementary Figure A). The 1-year post-procedural ISR rates were 23.9% (16/67 lesions) and 12.1% (17/141 lesions) in the long and non-long lesion groups, respectively (P=0.03). However, there were no significant between-group differences in bifurcation site restenosis and in the restenosis location (Supplementary Table 2; Supplementary Figure B,C).
The main findings of this study were that: (1) the cumulative 1-year clinical outcomes of non-LMT coronary bifurcation lesions treated with the 2-stent strategy using EES were acceptable; (2) long SB lesions and lesions treated with 3-link EES were independent predictors of ISR 1 year after the procedure; and (3) the stent link design may be associated with 1-year post-procedural restenosis, mainly in the SB ostium.
In this study, the 1-year post-procedural ISR rate was 15.9%, which is relatively higher than that in other studies.12,13 The ISR rate in the Bifurcations Bad Krozingen (BBK) II study, including culotte and T–and-protrusion stenting, was 10.7%,12 whereas that in the CELTIC Bifurcation study, with culotte stenting alone, was 10.8%.13 The BBK II study excluded lesions with severe calcification or tortuosity and the CELTIC Bifurcation study excluded patients on hemodialysis because both were randomized studies. Conversely, the present study included patients on hemodialysis (5.3%) and lesions with chronic total occlusion (13.4%), which may account for the higher ISR rate in this study. Despite the higher incidence of 1-year post-procedural restenosis, the 1-year cumulative incidence of TLR in the present study was low, similar to that in the BBK II study.12 Functional ischemic examinations using a pressure wire and precise clinical assessment may prevent TLR.
A meta-analysis showed that clinical outcomes of the 2-stent strategy with second-generation drug-eluting stents (DES) were comparable to those of the single-stent strategy.14 In the Korean Coronary Bifurcation Stenting (COBIS) II registry, which compared 2- and single-stent strategies for bifurcation lesions, clinical outcomes (cardiac death, MI, ST, and TLR) were not significantly different in non-LMT bifurcation lesions.4 Comparing the clinical outcomes of the present study and with those of the single-stent strategy in the COBIS II registry revealed similarly low rates of cardiac death and MI in both studies. In contrast, early ST was detected in 4 cases in the present study (Supplementary Table 3). The bifurcation lesion is a predictive factor for early ST after PCI,15 and complex procedures such as the 2-stent strategy may lead to a higher risk of early ST in bifurcation lesions because of more overlapping stents and a higher risk of undersizing or malapposition. A more meticulous approach using intravascular imaging, robust dual antiplatelet therapy, and close follow-up should be used for patients treated with the 2-stent strategy, particularly in the early phase.
In the present study, the number of links seemed to be associated with the 1-year post-procedural angiographic ISR rate. Some studies have shown that the stent jails of the SB ostium and malapposition of the bifurcation area are associated with restenosis at the SB ostium.6–8 Stents with a lower number of links may have larger cell areas when adequately dilated and this can reduce the proportion of stent jails of the SB ostium.16 In fact, a previous bench test showed that the 2-link stent had a wider SB ostium and lower stent strut jail.17 Furthermore, optical coherence tomography analysis showed that a lower number of links reduced the incidence of the link-connecting configuration.18 For these reasons, a lower number of links may have improved the angiographic outcomes in the bifurcation lesions. The CELTIC Bifurcation study was the only study in which the angiographic and clinical outcomes were compared between patients with 3- and 2-link DES and treated with a 2-stent strategy.13 There were no differences in angiographic outcomes between the 2 groups; however, the 2-link DES was numerically superior to the 3-link DES in terms of ISR (7.7% and 13.9%, respectively; P=0.32). The present study had a larger sample size than the CELTIC Bifurcation study and so may have allowed us to identify that the 2-link design is associated with better angiographic outcomes in patients who undergo treatment with a 2-stent strategy. If the 2-stent strategy is indicated for patients with true bifurcation lesions, stent selection based on stent link design may contribute to favorable outcomes.
Prior studies demonstrated that a longer lesion length and/or the use of longer stents are associated with a higher incidence of restenosis.19,20 Longer coronary stenotic lesions may represent greater progression of atherosclerosis. This may be why lesion length longer than usual is generally a risk factor for ISR in patients after PCI. It is also true that the efficacy of the 2-stent strategy has been demonstrated in cases of lesions >10 mm in length in the SB.21,22 It may not be necessary to avoid the 2-stent strategy just because the lesion length of the SB is longer than usual. Indications for the 2-stent strategy should be judged on the basis of vessel diameter and lesion morphology.
Diabetes and end-stage renal failure are generally known to be risk factors for ISR, but not in the present study. The primary outcome measure of this study was angiographic results. The risk of ISR in patients treated with 2-stent strategies may be more strongly associated with procedural rather than patient characteristics, such as diabetes.23 In addition, patients with renal failure may not always receive follow-up coronary angiography. Because of the small number of patients, the results of the present study are inconclusive with regard to whether patients undergoing hemodialysis are at a higher risk of ISR.
The present study has some limitations. First, this was a retrospective observational study, and selection bias possibly existed because of each operator’s preference for the type of stent or procedure. Second, due to the small sample size, we could not assess the difference between patients treated with 3- and 2-link EES in terms of hard clinical endpoints, such as cardiac death, MI, and ST. Therefore, we defined angiographic outcomes as the primary outcome measure. Third, other 2-stent strategies, such as a double kissing crush technique, were not performed and the findings in this study cannot be extrapolated to all cases of two stenting. Fourth, we cannot rule out effects of the study period, operators’ preferences, link design (peak-to-bottom connection in Xience vs. peak-to-peak connection in Promus) and stent material (cobalt-chromium in Xience vs. platinum-chromium in Promus) on the results. Finally, we used single-vessel QCA software instead of dedicated bifurcation QCA software. Moreover, the QCA studies were not performed in an independent core laboratory. Instead, a well-validated in-hospital system was used.
The 1-year cumulative clinical outcomes of patients with non-left main coronary bifurcation lesions treated with the 2-stent strategy using EES were acceptable. Some specific characteristics were independent predictors of ISR within 1 year after the use of the 2-stent strategy for non-left main coronary bifurcation lesions.
The authors appreciate the staff members of the cardiac catheterization laboratory, and Miho Kobayashi, Makiko Kanaike, Yoshimi Akashi, and Takako Yukiyoshi for their assistance with the manuscript.
This study did not receive any specific funding.
H.T. recieved honorarium from Abbot Vascular. K.K. recieved honorarium from Abbot Vascular and Boston Scientific.
This study was approved by the Institutional Review Board of Kurashiki Central Hospital (Reference no. 3535).
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-20-1281