2022 年 86 巻 12 号 p. 1941-1942
2022 年 86 巻 12 号 p. 1941-1942
Hypertrophic cardiomyopathy (HCM) is defined by an increase in the thickness of the myocardial wall in one or more of the left ventricular (LV) wall segments that cannot be explained by abnormal loading conditions.1 HCM is a type of cardiomyopathy characterized by a wide variety of clinical manifestations and heterogeneity in both etiology and clinical course. There are many phenotypes of HCM, including differences in the severity and location of LV obstruction, as well as in the geometry of hypertrophy, and different stages, such as the dilated phase with a decline in LV ejection fraction. The clinical consequences are heavily dependent on the phenotypes. Because of these differences, HCM can range from mild to severe, and the seemingly simple question of how to manage it in different medical facilities, ranging from primary care doctors to specialized facilities, remains unsolved.
Article p 1934
The development of heart failure (HF) and arrhythmic events, including sudden cardiac death, is the most serious problem in HCM. HF in HCM is classified into 2 types: HF with preserved ejection fraction (HFpEF), which is caused primarily by obstruction in the LV cavity but can also be induced by diastolic dysfunction, and HF with reduced ejection fraction (HFrEF), which is often caused by progression to the dilated phase of HCM.2 Practically, HF derived from HCM involves more multifaceted factors and is extremely diverse in terms of its clinical course. In a contemporary registry of 1,739 individuals with HCM in Europe, the prevalence of symptomatic HF was 67% (New York Heart Association III–IV symptoms 17.4%).3 However, the clinical profiles of HF development in HCM patients have not been completely explored.
The study of Miyamoto et al in this issue of the Journal provides a profound insight into the risk stratification for HF development in HCM patients in the Japanese population.4 In that study, Miyamoto et al analyzed an HCM cohort, following 293 patients in 9 hospitals for a median follow-up of 6.1 years, focusing on HF development.4 The authors identified significant predictors of HF events: atrial fibrillation (AF), a low percentage of fractional shortening (%FS), and high levels of B-type natriuretic peptide (BNP). In the study, the occurrence rate of HF events, defined as HF death and hospitalization for HF, was approximately 10% during 5 years.4 The authors also established a scoring system for predicting HF events using AF, %FS <40%, and BNP >300 pg/mL.4 This scoring system enabled the accurate prediction of HF events, allowing HCM patients to be classified as either at low (event rate <5% during 5 years) or high (event rate 50% during 5 years) risk for HF events (Figure).
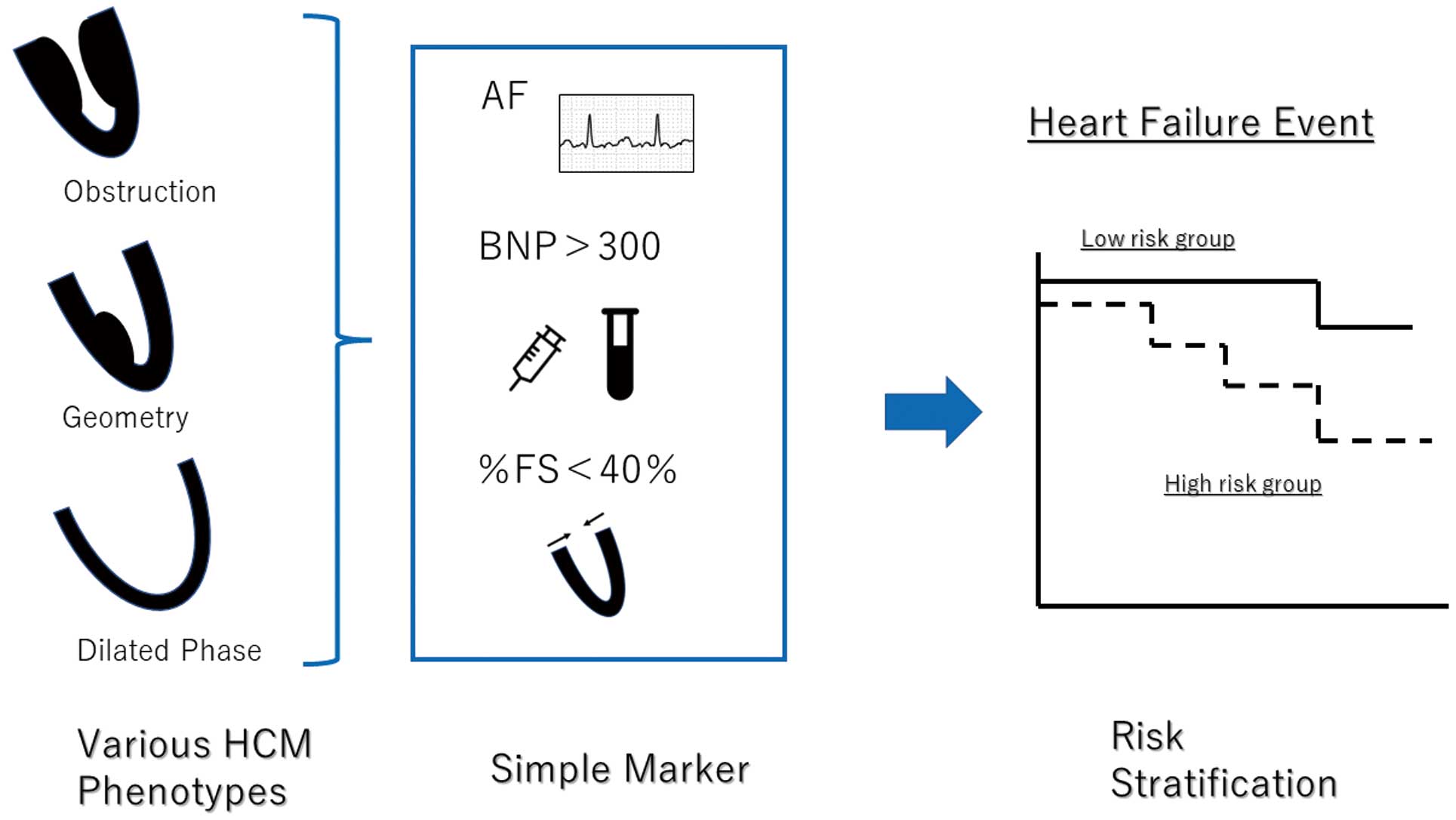
Simple marker for the development of heart failure in hypertrophic cardiomyopathy (HCM). AF, atrial fibrillation; BNP, B-type natriuretic peptide; FS, fractional shortening.
Surprisingly, phenotypic variables such as LV obstruction were not included in this scoring system. As a result, the scoring system is quite a simple one, fit for clinical use. Indeed, various studies have showed that the degree of outflow tract obstruction could influence the development of HF in HCM patients.5,6 However, the appropriate measure and decisions regarding treatment options for LV obstruction are complicated and highly specialized issues.7,8 In establishing a simple scoring system fit for clinical use, including a simple risk marker reflecting LV obstruction is favorable. The BNP level is a simple risk marker known to be linked with the severity of LV obstruction.9 Therefore, the inclusion of BNP levels in the scoring system developed by Miyamoto et al4 corresponds, to a certain extent, to taking LV obstruction as a risk for HF development into consideration.
Furthermore, in HCM patients, there has been some controversy regarding the effect of AF on the development of clinical events. According to Rowin et al,10 AF is not an independent determinant of HF morbidity and, rather, is associated with low cardiovascular mortality in terms of HF, arrhythmic sudden death, or thromboembolism. Conversely, another study reported that AF increased the mortality rate in HCM patients,11 with a higher proportion of HF and stroke-related deaths in HCM patients with AF. That report suggested that AF may correspond to the development of the disease towards HF. In addition, HCM patients with an LV ejection fraction <50% exhibited considerable LV remodeling, as indicated by late gadolinium enhancement in cardiovascular magnetic resonance imaging,12 highlighting the association between low %FS and poor prognosis, which is consistent with the findings observed in the study of Miyamoto et al.4 Together, the results indicate that there is a good association of AF, low %FS, and high BNP levels with the progression of disease trajectory and cardiac remodeling in HCM patients; therefore, it would make sense that all these factors were involved in the scoring system established by Miyamoto et al.4
HCM is a disease for which process and prognosis vary greatly depending on whether a patient presents to a facility specializing in the medical management of that disease.13,14 To maximize the effect of appropriate management for each HCM patient, in reference to the user-friendly scoring system predicting HF development, the timing of referral to specialized facilities should be appropriately determined.
None.
E.A. belongs to a department endowed by NIPRO Corp., Terumo Corp., Senko Medical Instrument Mfg., Century Medical, Inc., ONO Pharmaceutical Co., Ltd., Medtronic JAPAN Co., Ltd., Nippon Shinyaku Co., Ltd., Mochida Pharmaceutical Co., Boehringer Ingelheim Pharmaceuticals Inc., Abiomed Inc., AQuA Inc., Fukuda-Denshi Co., Ltd., and Sun Medical Technology Research Corp. E.A. has also received research funds from Bristol Myers Squibb. H.M. is a member of Circulation Journal’s Editorial Board.