Abstract
Background:
The clinical significance of concomitant mitral regurgitation (MR) has not been well addressed in patients with severe aortic stenosis (AS).
Methods and Results:
We analyzed 3,815 patients from a retrospective multicenter registry of severe AS in Japan (CURRENT AS registry). We compared the clinical outcomes between patients with moderate/severe MR and with none/mild MR according to the initial treatment strategy (initial aortic valve replacement [AVR] or conservative strategy). The primary outcome measure was a composite of aortic valve-related death or heart failure hospitalization. At baseline, moderate/severe MR was present in 227/1,197 (19%) patients with initial AVR strategy and in 536/2,618 (20%) patients with a conservative strategy. The crude cumulative 5-year incidence of the primary outcome measure was significantly higher in patients with moderate/severe MR than in those with none/mild MR, regardless of the initial treatment strategy (25.2% vs. 14.4%, P<0.001 in the initial AVR strategy, and 63.3% vs. 40.7%, P<0.001 in the conservative strategy). After adjusting confounders, moderate/severe MR was not independently associated with higher risk for the primary outcome measure in the initial AVR strategy (hazard ratio [HR] 1.11, 95% confidence interval [CI] 0.67–1.83, P=0.69), and in the conservative strategy (HR 1.13, 95% CI 0.93–1.37, P=0.22).
Conclusions:
Concomitant moderate/severe MR was not independently associated with higher risk for the primary outcome measure regardless of the initial treatment strategy.
Mitral regurgitation (MR) often coexists with severe aortic stenosis (AS).1,2
The prevalence of concomitant moderate or severe MR has been reported in 13%3
to 33%4
of patients undergoing surgical aortic valve replacement (SAVR) and in 20–30% of patients undergoing transcatheter aortic valve replacement (TAVR).2
In the current American College of Cardiology (ACC)/American Heart Association (AHA) guidelines, concomitant mitral valve repair or replacement is recommended for patients with severe primary MR (Class I) and mitral valve repair is described as a reasonable option for patients with moderate primary MR (Class IIa) when undergoing other cardiac surgery.5
Concomitant moderate functional MR in patients with severe AS is thought to often improve after SAVR without mitral intervention,6
although MR with a rheumatic or degenerative etiology does not improve in most patients undergoing isolated SAVR.7
In patients who underwent isolated SAVR, moderate concomitant MR has been thought to be associated with worse survival rate after surgery.8
With regard to patients undergoing TAVR, concomitant MR is also thought to be associated with worse prognosis.9,10
Nevertheless, the prognostic impact of coexisting MR in severe AS remains controversial.
Editorial p 438
The aim of this study was to describe the clinical characteristics and factors associated with moderate/severe MR in patients with severe AS and to evaluate the prognostic impact of concomitant moderate/severe MR in patients with severe AS who either underwent initial SAVR or were managed conservatively.
Methods
Study Population
The CURRENT AS (Contemporary outcomes after sURgery and medical tREatmeNT in patients with severe Aortic Stenosis) registry is a retrospective multicenter registry that enrolled 3,815 consecutive patients with severe AS from 27 centers in Japan between January 2003 and December 2011 (Supplementary Appendix). Institutional review boards at all participating centers approved the protocol, and this study followed the Declaration of Helsinki and the ethical standards of the responsible committees on human experimentation. The need to obtain informed consent was waived because of the retrospective nature of the study. The details of the study design and primary results of the registry have been previously published.11
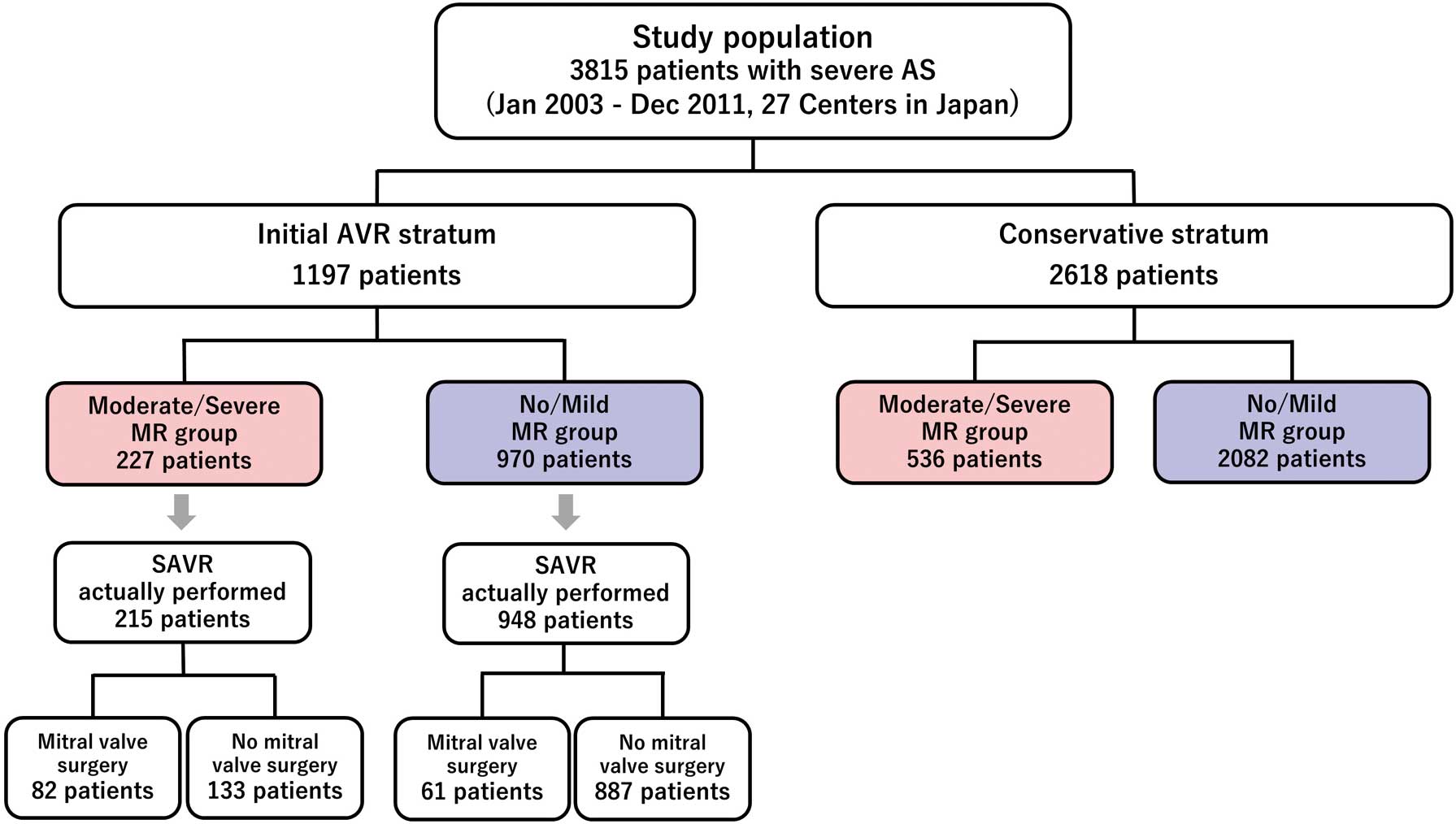
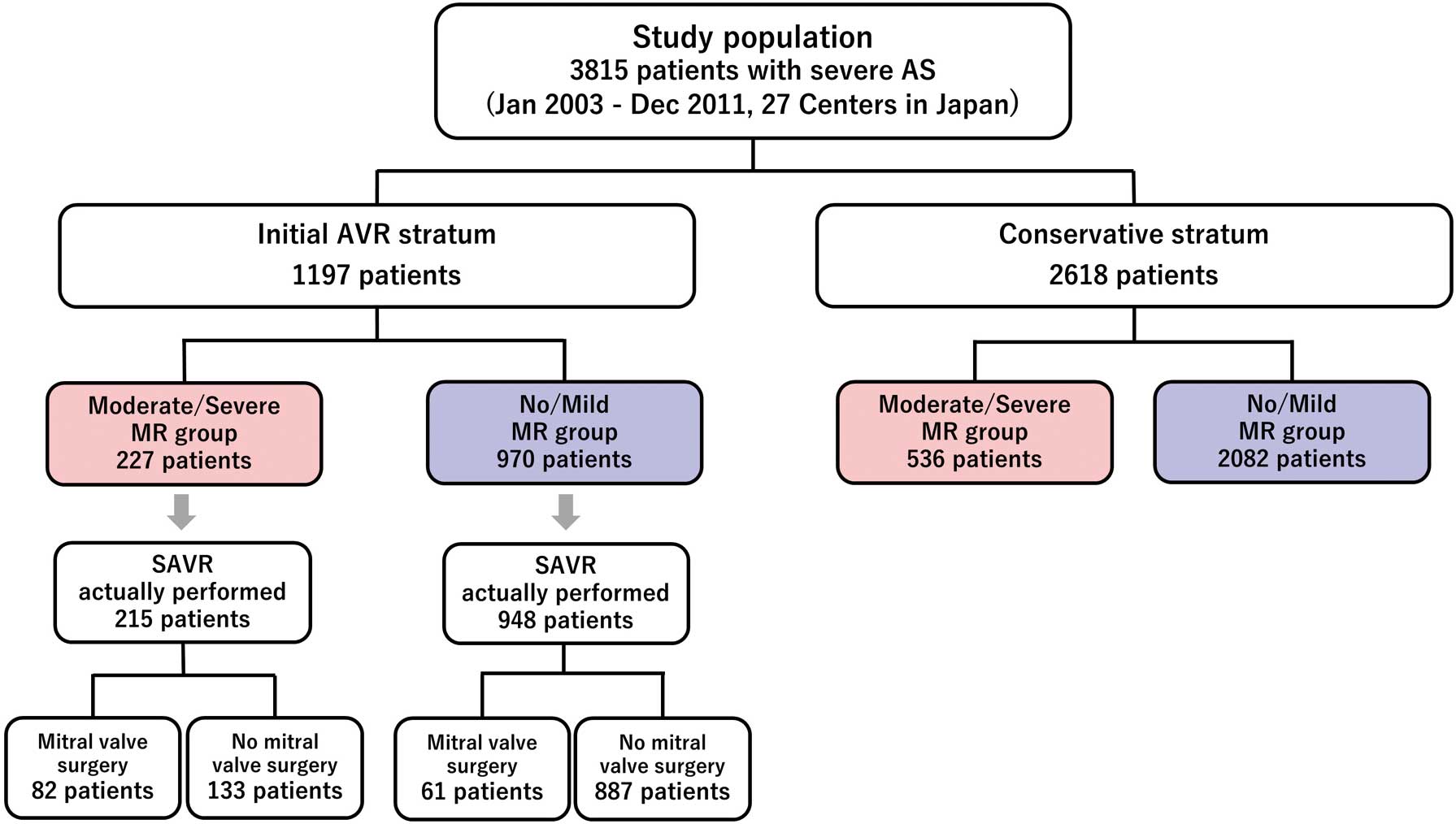
Of the 3,815 patients in the entire cohort, the study population was divided into 2 groups based on the initial treatment strategy after the index echocardiography (initial aortic valve replacement [AVR] group: n=1,197; conservative management group: n=2,618) (Figure 1). During the study period (2003–2011), only surgical AVR was available in Japan except for clinical trials usage. Follow-up data were collected from medical chart review in each participating center or through contact with patients, families and/or referring physicians by mail or telephone.
Echocardiographic data were not assessed in a central core laboratory, but were assessed in each participating center. MR severity on index echocardiography was graded as none, mild, moderate, or severe according to the American Society of Echocardiography recommendations.12,13
Because of the retrospective nature of the registry, the etiology (e.g., degenerative or functional) of MR was not collected. We also could not collect the multiple quantitative parameters for MR severity assessment. We subdivided the study population into 2 groups according to the semiquantitative measurement of MR severity (no/mild MR group and moderate/severe MR group). We analyzed the clinical impact of moderate/severe MR on prognosis in patients with severe AS stratified by the initial treatment strategy.
Study Outcomes
The primary outcome measure was a composite of aortic valve-related death or hospitalization for heart failure (HF). Aortic valve-related death consisted of aortic procedure-related death, sudden death, and death due to HF considered to be related to the aortic valve. Aortic procedure-related death was defined as any death during the hospitalization for AVR or transcatheter aortic valve implantation. Sudden death was defined as unexplained death in a previously stable patient. HF hospitalization was defined as hospitalization due to worsening HF requiring intravenous drug therapy. Other secondary outcome measures included all-cause death, cardiovascular death, sudden death, and noncardiovascular death. Death was regarded as cardiovascular in origin unless obvious noncardiovascular cause. The causes of death were retrospectively classified according to the Valve Academic Research Consortium definitions, and were adjudicated by a Clinical Event Committee (Supplementary Appendix).14,15
Definitions of the clinical events are given in the
Supplementary Appendix.
Statistical Analysis
Continuous variables are expressed as the mean and standard deviation or median and interquartile range. Categorical variables are expressed as numbers and percentages. We used a t-test or Wilcoxon’s rank sum test for continuous variables, and a Chi-square test or Fisher’s exact test for categorical variables. We conducted a multivariable logistic regression analysis to evaluate the clinical factors associated with concomitant moderate/severe MR, including 15 clinically relevant candidate variables. Survival analysis was performed by Kaplan-Meier, and differences between groups were assessed with a log-rank test. Multivariable Cox proportional hazards models were used to assess the risks of moderate/severe MR relative to none/mild MR for the clinical outcome measures, which were expressed as hazard ratios (HRs) and their 95% confidence intervals (CIs). Consistent with our previous report,11
we incorporated 20 factors in the initial AVR stratum and 19 factors in the conservative stratum as risk-adjusting variables, and the centers were incorporated as the stratification variable in the multivariable Cox proportional hazard models. Continuous risk-adjusting variables were dichotomized using the median or clinically meaningful reference values except for age. Missing values of binary variables were considered to be null because the physicians did not record these variables if there were no pertinent findings. Missing values of continuous variables were not to be imputed and analyses were conducted for the observations without missing variables. Proportional hazard assumptions for the variable included in the Cox proportional hazard models were assessed on the plots of log (time) vs. log [-log (survival)] stratified by the variable. The assumptions were considered acceptable for all the variables. In all analyses, two-tailed P value <0.05 was considered statistically significant. Statistical analyses were performed by physicians (R.M. and T.T.) and a statistician (T. Morimoto) using JMP 11.2.1 (SAS Institute Inc., Cary, NC, USA), R software package version 3.5.2. or SAS version 9.4 (SAS Institute Inc.).
Results
Baseline Clinical Characteristics and Associated Factors of Moderate/Severe MR
Among the total of 3,815 patients, MR grades on index echocardiography were none (n=787), mild (n=2,265), moderate (n=643) and severe (n=120). Thus, 763 (20%) patients had moderate/severe MR and 3,052 (80%) patients had no/mild MR on index echocardiography. Baseline characteristics were significantly different between the 2 groups (Table 1). Patients with moderate/severe MR were older, and more often had prior myocardial infarction, history of HF, atrial fibrillation, anemia, and renal dysfunction. Regarding the echocardiographic parameters, patients with moderate/severe MR had larger LV end-diastolic and endsystolic diameters, and more often had LV dysfunction, moderate/severe tricuspid regurgitation (TR), and pulmonary hypertension. The clinical factors independently associated with moderate/severe MR were age, low body mass index, prior myocardial infarction, history of HF, history of atrial fibrillation, hemodialysis, and anemia in the multivariable logistic regression analysis (Table 2).
Table 1.
Baseline Characteristics and Echocardiographic Findings in the Entire Study Population According to Significance of MR
| |
Moderate/severe MR
(n=763) |
No/mild MR
(n=3,052) |
P value |
| Clinical characteristics |
| Age, years*, mean±SD |
80.1±9.3 |
77.2±9.8 |
<0.001 |
| ≥80 years, n (%) |
424 (55.6) |
1,305 (42.8) |
<0.001 |
| Men,* n (%) |
254 (33.3) |
1,189 (39.0) |
0.004 |
| BMI <22 kg/m2,* n (%) |
549 (72.0) |
1,777 (58.2) |
<0.001 |
| Hypertension,* n (%) |
513 (67.2) |
2,154 (70.6) |
0.08 |
| Dyslipidemia, n (%) |
214 (28.0) |
1,113 (36.5) |
<0.001 |
| On statin therapy, n (%) |
155 (20.3) |
815 (26.7) |
<0.001 |
| Diabetes, n (%) |
155 (20.3) |
742 (24.3) |
0.02 |
| On insulin therapy,* n (%) |
28 (3.7) |
160 (5.2) |
0.09 |
| Smoking history, n (%) |
147 (19.3) |
683 (22.4) |
0.07 |
| Current smoking,* n (%) |
37 (4.8) |
159 (5.2) |
0.76 |
| Prior MI,* n (%) |
82 (10.7) |
241 (7.9) |
0.01 |
| Prior open heart surgery, n (%) |
48 (6.3) |
268 (8.8) |
0.03 |
| History of HF, n (%) |
217 (28.4) |
428 (14.0) |
<0.001 |
| Prior symptomatic stroke,* n (%) |
114 (14.9) |
389 (12.7) |
0.12 |
| Atrial fibrillation or flutter,* n (%) |
268 (35.1) |
560 (18.3) |
<0.001 |
| Aortic/PVD,* n (%) |
111 (14.5) |
468 (15.3) |
0.63 |
| Serum creatinine, mg/dL, median [IQR] |
1.00 [0.78, 1.55] |
0.86 [0.70, 1.20] |
<0.001 |
| Serum creatinine level >0.83 mg/dL,* n (%) |
478 (62.6) |
1,418 (46.5) |
<0.001 |
| Hemodialysis,* n (%) |
102 (13.4) |
303 (9.9) |
0.007 |
| Anemia,*,† n (%) |
514 (67.4) |
1,603 (52.5) |
<0.001 |
| Liver cirrhosis (Child-Pugh B/C),* n (%) |
8 (1.0) |
30 (1.0) |
1 |
| Malignancy |
96 (12.6) |
421 (13.8) |
0.42 |
| Malignancy currently under treatment* |
30 (3.9) |
119 (3.9) |
1 |
| Chronic lung disease |
85 (11.1) |
315 (10.3) |
0.55 |
| Chronic lung disease (moderate or severe),* n (%) |
24 (3.1) |
88 (2.9) |
0.79 |
| STS score (PROM), median [IQR] |
5.1 [2.9, 8.9] |
3.5 [2.1, 5.9] |
<0.001 |
| Any symptoms at index echocardiography, n (%) |
550 (72.1) |
1,455 (47.7) |
<0.001 |
| HF symptoms at index echocardiography, n (%) |
496 (65.0) |
1,107 (36.3) |
<0.001 |
| NYHA functional class, n (%) |
|
|
<0.001 |
| II |
202 (40.7) |
644 (58.2) |
|
| III |
136 (27.4) |
225 (20.3) |
|
| IV |
151 (30.4) |
222 (20.1) |
|
| Unknown |
7 (1.4) |
16 (1.4) |
|
| Echocardiographic findings |
| Vmax, m/s mean±SD |
4.1±1.0 |
4.1±0.9 |
0.24 |
| Vmax ≥4.0 m/s,* n (%) |
424 (55.6) |
1,761 (57.7) |
0.31 |
| Mean aortic PG, mmHg mean±SD |
39.7±21.5 |
41.1±19.2 |
0.10 |
| AVA (equation of continuity), cm2 mean±SD |
0.67±0.20 |
0.73±0.18 |
<0.001 |
| LV end-diastolic diameter, mm mean±SD |
49.0±7.8 |
45.2±6.6 |
<0.001 |
| LV endsystolic dimeter, mm mean±SD |
34.4±9.4 |
29.2±7.1 |
<0.001 |
| LVEF, % mean±SD |
56.8±15.7 |
64.3±12.4 |
<0.001 |
| LVEF <40%, n (%) |
125 (16.4) |
168 (5.5) |
<0.001 |
Any combined moderate or severe valvular disease
other than MR,* n (%) |
481 (63.0) |
795 (26.0) |
<0.001 |
| AR, n (%) |
277 (36.3) |
514 (16.8) |
<0.001 |
| MS, n (%) |
46 (6.0) |
87 (2.9) |
<0.001 |
| TR, n (%) |
321 (42.1) |
307 (10.1) |
<0.001 |
| TR pressure gradient ≥40 mmHg, n (%) |
266 (34.9) |
340 (11.1) |
<0.001 |
*Risk-adjusting variables selected for the Cox proportional hazard model. †Defined by the World Health Organization criteria (hemoglobin <12.0 g/dL in women and <13.0 g/dL in men). AR, aortic regurgitation; AVA, aortic valve area; AVR, aortic valve replacement; BMI, body mass index; HF, heart failure; IQR, interquartile range; LV, left ventricular; LVEF, left ventricular ejection fraction; MI, myocardial infarction; MR, mitral regurgitation; MS, mitral stenosis; PG, pressure gradient; PROM, predicted risk of mortality; PVD, peripheral vascular disease; SD, standard deviation; STS, Society of Thoracic Surgeons; TR, tricuspid regurgitation; Vmax, peak aortic jet velocity.
Table 2.
Logistic Regression Analysis for the Predictors of Moderate/Severe MR
| Variables |
Univariate |
Multivariate |
| OR |
95% CI |
P value |
OR |
95% CI |
P value |
| Age ≥80 years |
1.67 |
1.43–1.96 |
<0.001 |
1.41 |
1.17–1.68 |
<0.001 |
| Male |
0.78 |
0.66–0.92 |
0.004 |
0.84 |
0.70–1.01 |
0.06 |
| BMI <22 |
1.84 |
1.54–2.19 |
<0.001 |
1.42 |
1.18–1.71 |
<0.001 |
| Hypertension |
0.85 |
0.72–1.01 |
0.07 |
0.90 |
0.75–1.08 |
0.27 |
| Dyslipidemia |
0.68 |
0.57–0.80 |
<0.001 |
0.81 |
0.67–0.98 |
0.03 |
| Diabetes on insulin |
0.69 |
0.46–1.04 |
0.07 |
0.68 |
0.45–1.05 |
0.08 |
| Current smoking |
0.93 |
0.64–1.34 |
0.69 |
1.39 |
0.94–2.05 |
0.10 |
| Prior MI |
1.40 |
1.08–1.83 |
0.01 |
1.36 |
1.02–1.82 |
0.04 |
| Prior symptomatic stroke |
1.20 |
0.96–1.51 |
0.11 |
0.97 |
0.77–1.24 |
0.82 |
| Atrial fibrillation or flutter |
2.41 |
2.02–2.87 |
<0.001 |
2.10 |
1.75–2.53 |
<0.001 |
| Aortic/PVD |
0.94 |
0.75–1.18 |
0.59 |
0.83 |
0.65–1.06 |
0.14 |
| Hemodialysis |
1.40 |
1.10–1.78 |
0.006 |
1.41 |
1.07–1.84 |
0.01 |
| Anemia† |
1.87 |
1.58–2.21 |
<0.001 |
1.53 |
1.28–1.83 |
<0.001 |
| Chronic lung disease (moderate or severe) |
1.09 |
0.69–1.73 |
0.70 |
0.96 |
0.59–1.55 |
0.85 |
| History of HF admission |
2.44 |
2.02–2.94 |
<0.001 |
1.84 |
1.51–2.25 |
<0.001 |
†Defined by the World Health Organization criteria (hemoglobin <12.0 g/dL in women and <13.0 g/dL in men). BSA, body surface area; CI, confidence interval; OR, odds ratio. Other abbreviations as in Table 1.
Moderate/severe MR was present in 227 patients (19%) of 1,197 in the initial AVR stratum, and in 536 patients (20%) of 2,618 in the conservative stratum. The differences of the baseline clinical characteristics between the moderate/severe MR and no/mild MR group in each treatment strategy were consistent with those in the overall population (Table 3). Among 1,174 patients who actually underwent SAVR in the initial AVR group, 143 (12%) underwent concomitant mitral valve surgery (61 in the no/mild MR group and 82 in the moderate/severe MR group) (Supplementary Table 1).
Table 3.
Baseline Characteristics and Echocardiographic Findings in the Initial AVR and Conservative Treatment Strata According to Significance of MR
| |
Initial AVR stratum |
Conservative stratum |
Moderate/severe MR
(n=227) |
No/mild MR
(n=970) |
P value |
Moderate/Severe MR
(n=536) |
No/mild MR
(n=2,082) |
P value |
| Clinical characteristics |
| Age, years,* mean±SD |
74.7±7.7 |
73.0±9.2 |
0.01 |
82.3±8.9 |
79.1±9.5 |
<0.001 |
| Age ≥80 years, n (%) |
68 (30.0) |
231 (23.8) |
0.07 |
356 (66.4) |
1,074 (51.6) |
<0.001 |
| Men,* n (%) |
94 (41.4) |
413 (42.6) |
0.81 |
160 (29.9) |
776 (37.3) |
0.002 |
| BMI <22 kg/m2,* n (%) |
139 (61.2) |
483 (49.8) |
0.002 |
410 (76.5) |
1,294 (62.2) |
<0.001 |
| Hypertension,* n (%) |
143 (63.0) |
664 (68.5) |
0.13 |
370 (69.0) |
1,490 (71.6) |
0.27 |
| Dyslipidemia, n (%) |
75 (33.0) |
401 (41.3) |
0.03 |
139 (25.9) |
712 (34.2) |
<0.001 |
| On statin therapy, n (%) |
52 (22.9) |
287 (29.6) |
0.054 |
103 (19.2) |
528 (25.4) |
0.004 |
| Diabetes, n (%) |
43 (18.9) |
233 (24.0) |
0.122 |
112 (20.9) |
509 (24.4) |
0.10 |
| On insulin therapy,* n (%) |
9 (4.0) |
49 (5.1) |
0.61 |
19 (3.5) |
111 (5.3) |
0.11 |
| Smoking history, n (%) |
51 (22.5) |
263 (27.1) |
0.18 |
96 (17.9) |
420 (20.2) |
0.27 |
| Current smoking,* n (%) |
12 (5.3) |
71 (7.3) |
0.35 |
25 (4.7) |
88 (4.2) |
0.75 |
| Prior MI,* n (%) |
16 (7.0) |
35 (3.6) |
0.03 |
66 (12.3) |
206 (9.9) |
0.12 |
| Prior open heart surgery, n (%) |
9 (4.0) |
39 (4.0) |
1 |
39 (7.3) |
229 (11.0) |
0.014 |
| History of HF, n (%) |
40 (17.6) |
110 (11.3) |
0.014 |
177 (33.0) |
318 (15.3) |
<0.001 |
| Prior symptomatic stroke,* n (%) |
24 (10.6) |
83 (8.6) |
0.41 |
90 (16.8) |
306 (14.7) |
0.26 |
| Atrial fibrillation or flutter,* n (%) |
70 (30.8) |
137 (14.1) |
<0.001 |
198 (36.9) |
423 (20.3) |
<0.001 |
| Aortic/PVD,* n (%) |
24 (10.6) |
138 (14.2) |
0.18 |
87 (16.2) |
330 (15.9) |
0.88 |
| Serum creatinine, mg/dL, median [IQR] |
0.98
[0.78, 1.43] |
0.80
[0.66, 1.03] |
<0.001 |
1.00
[0.78, 1.64] |
0.90
[0.70, 1.30] |
<0.001 |
| Serum creatinine level >0.83 mg/dL,* n (%) |
143 (63.0) |
422 (43.5) |
<0.001 |
335 (62.5) |
996 (47.8) |
<0.001 |
| Serum creatinine level >2 mg/dL, n (%) |
44 (19.5) |
105 (11.0) |
0.001 |
96 (20.1) |
272 (15.5) |
0.02 |
| Hemodialysis,* n (%) |
39 (17.2) |
96 (9.9) |
0.003 |
63 (11.8) |
207 (9.9) |
0.25 |
| Anemia,*,† n (%) |
140 (61.7) |
489 (50.4) |
0.003 |
374 (69.8) |
1,114 (53.5) |
<0.001 |
| Liver cirrhosis (Child-Pugh B/C),* n (%) |
2 (0.9) |
4 (0.4) |
0.705 |
6 (1.1) |
26 (1.2) |
0.98 |
| Malignancy |
25 (11.0) |
106 (1.9) |
1 |
71 (13.2) |
315 (15.1) |
0.30 |
| Malignancy currently under treatment* |
7 (3.1) |
17 (1.8) |
0.31 |
23 (4.3) |
102 (4.9) |
0.64 |
| Chronic lung disease |
33 (14.5) |
108 (11.1) |
0.19 |
52 (9.7) |
207 (9.9) |
0.93 |
| Chronic lung disease (moderate or severe),* n (%) |
4 (1.8) |
15 (1.5) |
1 |
20 (3.7) |
73 (3.5) |
0.90 |
| STS score (PROM), median [IQR] |
3.8 [2.2, 6.3] |
2.6 [1.7, 4.4] |
<0.001 |
5.8 [3.4, 9.9] |
4.0 [2.4, 6.8] |
<0.001 |
| Any symptoms at index echocardiography, n (%) |
201 (88.5) |
704 (72.6) |
<0.001 |
349 (65.1) |
751 (36.1) |
<0.001 |
| HF symptoms at index echocardiography, n (%) |
172 (75.8) |
487 (50.2) |
<0.001 |
324 (60.4) |
620 (29.8) |
<0.001 |
| NYHA functional class, n (%) |
|
|
<0.001 |
|
|
<0.001 |
| II |
75 (43.6) |
322 (66.1) |
|
127 (39.2) |
322 (51.9) |
|
| III |
57 (33.1) |
77 (15.8) |
|
79 (24.4) |
148 (23.9) |
|
| IV |
37 (21.5) |
76 (15.6) |
|
114 (35.2) |
146 (23.5) |
|
| Unknown |
3 (1.7) |
12 (2.5) |
|
4 (1.2) |
4 (0.6) |
|
| Echocardiographic findings |
| Vmax, m/s mean±SD |
4.6±1.0 |
4.7±0.8 |
0.159 |
3.9±1.0 |
3.9±0.8 |
0.95 |
| Vmax ≥4.0 m/s,* n (%) |
173 (76.2) |
821 (84.6) |
0.003 |
251 (46.8) |
940 (45.1) |
0.52 |
| Mean aortic PG, mmHg mean±SD |
50.8±20.5 |
54.4±19.2 |
0.03 |
35.0±20.1 |
35.3±16.2 |
0.68 |
| AVA (equation of continuity), cm2 mean±SD |
0.61±0.20 |
0.66±0.17 |
0.001 |
0.70±0.20 |
0.76±0.17 |
<0.001 |
| LV end-diastolic diameter, mm mean±SD |
51.1±8.0 |
46.2±6.6 |
<0.001 |
48.0±7.5 |
44.7±6.5 |
<0.001 |
| LV endsystolic dimeter, mm mean±SD |
36.5±9.9 |
29.8±7.7 |
<0.001 |
33.5±9.0 |
28.9±6.9 |
<0.001 |
| LVEF, % mean±SD |
55.8±16.0 |
64.4±13.0 |
<0.001 |
57.2±15.6 |
64.2±12.2 |
<0.001 |
| LVEF <40%, n (%) |
42 (18.5) |
61 (6.3) |
<0.001 |
83 (15.5) |
107 (5.1) |
<0.001 |
| Any combined moderate/severe valvular disease except MR,* n (%) |
149 (65.6) |
252 (26) |
<0.001 |
332 (61.9) |
543 (26.1) |
<0.001 |
| AR, n (%) |
101 (44.5) |
193 (19.9) |
<0.001 |
176 (32.8) |
321 (15.4) |
<0.001 |
| MS, n (%) |
18 (7.9) |
33 (3.4) |
0.004 |
28 (5.2) |
54 (2.6) |
0.003 |
| TR, n (%) |
85 (37.4) |
62 (6.4) |
<0.001 |
236 (44.0) |
245 (11.8) |
<0.001 |
| TR pressure gradient ≥40 mmHg, n (%) |
91 (40.1) |
89 (9.2) |
<0.001 |
175 (32.6) |
251 (12.1) |
<0.001 |
*Risk-adjusting variables selected for the Cox proportional hazard model. †Defined by the World Health Organization criteria (hemoglobin <12.0 g/dL in women and <13.0 g/dL in men). Abbreviations as in Table 1.
Among 1,197 patients in the initial AVR group, the crude cumulative 5-year incidence of the primary outcome measure was significantly higher in the moderate/severe MR group than in the no/mild group (25.2% vs. 14.4%, P<0.001) (Figure 2). After adjusting for confounders, moderate/severe MR was no longer associated with excess risk for the primary outcomes measure (HR 1.11, 95% CI 0.67–1.83, P=0.69) or for the secondary outcome measures (Table 4).

Table 4.
Clinical Outcomes in the Initial AVR and Conservative Treatment Strata According to Significance of MR
| Clinical outcomes |
Initial AVR stratum |
Conservative stratum |
Moderate/severe MR
N of patients with event
(Cumulative 5-year incidence)
(n=227) |
No/mild MR
N of patients with event
(Cumulative 5-year incidence)
(n=970) |
P value
(log-rank) |
Adjusted HR
(95% CI) |
P value |
Moderate/severe MR
N of patients with event
(Cumulative 5-year incidence)
(n=536) |
No/mild MR
N of patients with event
(Cumulative 5-year incidence)
(n=2,082) |
P value
(log-rank) |
Adjusted HR
(95% CI) |
P value |
Aortic valve-related death or
HF hospitalization |
47 (25.2%) |
118 (14.4%) |
<0.001 |
1.11 (0.67–1.83) |
0.69 |
257 (63.3%) |
650 (40.7%) |
<0.001 |
1.13 (0.93–1.37) |
0.22 |
| Aortic valve-related death |
22 (10.5%) |
46 (5.1%) |
0.002 |
1.14 (0.53–2.48) |
0.74 |
176 (47.4%) |
365 (23.6%) |
<0.001 |
1.46 (1.13–1.88) |
0.004 |
| HF hospitalization |
27 (17.6%) |
75 (10.1%) |
0.03 |
1.15 (0.60–2.23) |
0.67 |
209 (58.6%) |
501 (33.7%) |
<0.001 |
1.16 (0.93–1.44) |
0.18 |
| All-cause death |
58 (31.4%) |
178 (21.1%) |
0.01 |
0.884 (0.57–1.36) |
0.58 |
338 (69.6%) |
875 (47.2%) |
<0.001 |
1.27 (1.07–1.50) |
0.006 |
| Cardiovascular death |
45 (24.7%) |
106 (12.7%) |
<0.001 |
1.07 (0.62–1.83) |
0.81 |
248 (58.2%) |
553 (33.1%) |
<0.001 |
1.38 (1.12–1.70) |
0.002 |
| Sudden death |
10 (6.2%) |
17 (2.8%) |
0.02 |
|
|
41 (12.0%) |
128 (8.5%) |
0.01 |
1.22 (0.75–1.98) |
0.42 |
| Noncardiovascular death |
13 (8.9%) |
72 (9.6%) |
0.43 |
0.50 (0.22–1.13) |
0.096 |
90 (27.1%) |
322 (21.0%) |
0.008 |
1.02 (0.75–1.38) |
0.91 |
N of patients with event was counted through the entire follow-up period. HR, hazard ratio. Other abbreviations as in Tables 1,2.
Among 227 patients with moderate/severe MR in the initial AVR group, 215 actually underwent SAVR and of them, mitral valve surgery was simultaneously performed in 82 patients (mitral valve replacement: 35 patients; mitral annuloplasty: 28 patients; mitral valve plasty: 17 patients; annuloplasty with mitral valve plasty: 2 patients). Patient who underwent a mitral valve procedure had severe MR more frequently than those who did not (28.0% vs. 7.5%, P<0.001). The 30-day mortality rate was numerically higher in patients with SAVR and concomitant mitral valve surgery than in those without a concomitant mitral valve procedure (2.4% [n=2/82] vs. 0% [n=0/133], P=0.28). Postoperative echocardiography showed that MR improved in all patients who underwent mitral valve surgery, whereas residual moderate/severe MR was present in 22% of patients without a concomitant mitral valve procedure (Table 5). The cumulative 5-year incidence of the primary outcome measure was not significantly different between the 2 groups of patients who underwent SAVR with and without mitral valve surgery (21.6% vs. 22.9%, P=0.86) (Supplementary Table 2).
Table 5.
Baseline Characteristics, Echocardiographic Findings and Procedural Details, Postoperative Echocardiographic Findings and 30-Day Mortality After AVR in the Initial AVR Stratum According to Concomitant Mitral Valve Surgery
| Variables |
Patients with moderate/severe MR in the
initial AVR stratum (n=215) |
P value |
Mitral valve surgery
(n=82) |
No mitral valve surgery
(n=133) |
| Clinical characteristics |
| Age, years, mean±SD |
72.9±8.1 |
75.9±7.2 |
0.005 |
| Age ≥80 years, n (%) |
17 (20.7) |
48 (36.1) |
0.03 |
| Men, n (%) |
36 (43.9) |
52 (39.1) |
0.58 |
| BMI <22 kg/m2, n (%) |
55 (67.1) |
76 (57.1) |
0.19 |
| Hypertension, n (%) |
51 (62.2) |
82 (61.7) |
1 |
| Dyslipidemia, n (%) |
30 (36.6) |
41 (30.8) |
0.47 |
| On statin therapy, n (%) |
20 (24.4) |
29 (21.8) |
0.79 |
| Diabetes, n (%) |
17 (20.7) |
22 (16.5) |
0.55 |
| On insulin therapy, n (%) |
5 (6.1) |
4 (3.0) |
0.45 |
| Smoking history, n (%) |
20 (24.4) |
29 (21.8) |
0.79 |
| Current smoking, n (%) |
5 (6.1) |
6 (4.5) |
0.85 |
| Prior MI, n (%) |
7 (8.5) |
5 (3.8) |
0.24 |
| Prior open heart surgery, n (%) |
3 (3.7) |
4 (3.0) |
1 |
| History of HF, n (%) |
20 (24.4) |
15 (11.3) |
0.02 |
| Prior symptomatic stroke, n (%) |
10 (12.2) |
12 (9.0) |
0.61 |
| Atrial fibrillation or flutter, n (%) |
33 (40.2) |
33 (24.8) |
0.03 |
| Aortic/PVD, n (%) |
5 (6.1) |
15 (11.3) |
0.30 |
| Serum creatinine, mg/dL, median [IQR] |
0.96 [0.71, 1.23] |
0.98 [0.80, 1.48] |
0.55 |
| Serum creatinine level >0.83 mg/dL, n (%) |
50 (61.0) |
84 (63.2) |
0.86 |
| Hemodialysis, n (%) |
12 (14.6) |
24 (18.0) |
0.64 |
| Anemia,† n (%) |
48 (58.5) |
83 (62.4) |
0.67 |
| Liver cirrhosis (Child-Pugh B/C), n (%) |
1 (1.2) |
1 (0.8) |
1 |
| Malignancy |
5 (6.1) |
19 (14.3) |
0.10 |
| Malignancy currently under treatment |
0 (0.0) |
7 (5.3) |
0.09 |
| Chronic lung disease |
13 (15.9) |
18 (13.5) |
0.78 |
| Chronic lung disease (moderate or severe), n (%) |
2 (2.4) |
2 (1.5) |
1 |
| STS score (PROM), median [IQR] |
3.18 [2.10, 5.76] |
3.83 [2.22, 6.38] |
0.51 |
| Any symptoms at index echocardiography, n (%) |
72 (87.8) |
117 (88.0) |
1 |
| HF symptoms at index echocardiography, n (%) |
66 (80.5) |
94 (70.7) |
0.15 |
| NYHA functional class, n (%) |
|
|
0.28 |
| II |
34 (51.5) |
38 (40.4) |
|
| III |
22 (33.3) |
30 (31.9) |
|
| IV |
9 (13.6) |
24 (25.5) |
|
| Unknown |
1 (1.5) |
2 (2.1) |
|
| Echocardiographic findings |
| Vmax, m/s mean±SD |
4.5±1.0 |
4.8±0.9 |
0.02 |
| Vmax ≥4.0 m/s, n (%) |
56 (68.3) |
109 (82.0) |
0.03 |
| Peak aortic PG, mmHg mean±SD |
84.0±36.7 |
94.9±36.8 |
0.04 |
| AVA (equation of continuity), cm2 mean±SD |
0.65±0.19 |
0.59±0.20 |
0.05 |
| LV end-diastolic diameter, mm mean±SD |
52.1±7.6 |
50.2±8.2 |
0.10 |
| LV endsystolic dimeter, mm mean±SD |
37.7±9.7 |
35.2±9.7 |
0.07 |
| LVEF, % mean±SD |
52.2±15.2 |
59.3±15.1 |
0.001 |
| LVEF <40%, n (%) |
21 (25.6) |
15 (11.3) |
0.01 |
| MR severity, moderate/severe, n (%) |
59 (72.0)/23 (28.0) |
123 (92.5)/10 (7.5) |
<0.001 |
Any combined moderate or severe valvular
disease other than MR, n (%) |
54 (65.9) |
84 (63.2) |
0.80 |
| AR, n (%) |
32 (39.0) |
61 (45.9) |
0.40 |
| MS, n (%) |
15 (18.3) |
3 (2.3) |
<0.001 |
| TR, n (%) |
34 (41.5) |
44 (33.1) |
0.27 |
| TR pressure gradient ≥40 mmHg, n (%) |
43 (52.4) |
43 (32.3) |
0.005 |
| Details of surgery |
| MVR, n (%) |
35 (42.7) |
0 (0.0) |
<0.001 |
| MVP or annuloplasty, n (%) |
47 (57.3) |
0 (0.0) |
<0.001 |
| MVP |
19 (23.2) |
0 (0.0) |
<0.001 |
| Annuloplasty |
30 (36.6) |
0 (0.0) |
<0.001 |
| Bioprosthetic valve, n (%) |
58 (70.7) |
102 (76.7) |
0.42 |
| Mechanical prosthetic valve, n (%) |
24 (29.3) |
30 (22.6) |
0.35 |
| Tricuspid valve surgery, n (%) |
32 (39.0) |
9 (6.8) |
<0.001 |
| CABG, n (%) |
19 (23.2) |
43 (32.3) |
0.20 |
| MAZE operation, n (%) |
18 (22.0) |
9 (6.8) |
0.002 |
| Perioperative IABP use, n (%) |
8 (9.8) |
3 (2.3) |
0.04 |
| Postoperative echocardiography |
n=77 |
n=121 |
|
Echocardiographic assessment timing after
surgery, days median (IQR) |
14 (8–43) |
14 (9–355) |
0.25 |
| MR measurement, n (%) |
62/77 (80.5) |
115/121 (95.0) |
|
| MR moderate-severe after index AVR (%) |
1/62 (1.6) |
25/115 (21.7) |
<0.001 |
| MR change after index AVR (%) |
|
|
<0.001 |
| Improved |
62/62 (100) |
93/115 (80.8) |
|
| No change or worsened |
0/62 (0) |
22/115 (19.1) |
|
| 30-day mortality after AVR, n (%) |
2 (2.4) |
0 (0.0) |
0.28 |
†Defined by the World Health Organization criteria (hemoglobin <12.0 g/dL in women and <13.0 g/dL in men). CABG, coronary artery bypass grafting; IABP, intra-aortic balloon pumping; MVR, mitral valve replacement; MVP, mitral valve plasty. Other abbreviations as in Table 1.
Among 2,618 patients in the conservative management group, 569 patients (69 [13%] of 536 patients in the moderate/severe MR group and 500 [24%] of 2,082 patients in the no/mild MR group) underwent SAVR (540 patients) or TAVR (29 patients) during the follow-up period. Among these 2618 patients, the crude cumulative 5-year incidence of the primary outcome measure was significantly higher in the moderate/severe MR group than in the no/mild MR group (63.3% vs. 40.7%, P<0.001) (Figure 2). However, after adjusting confounders, moderate/severe MR on index echocardiography was no longer independently associated with excess risk for the primary outcome measure (HR 1.13, 95% CI 0.93–1.37, P=0.22). The adjusted excess risk of moderate/severe MR relative to no/mild MR remained significant for aortic valve-related death, cardiovascular death and all-cause death (Table 4).
We also conducted a sensitivity analysis to reduce the therapeutic bias of the conservative management stratum. We assessed the excessive risk of concomitant MR in the population who censored at the time of undergoing AVR. In this analysis, moderate/severe MR did not show excess risk of the primary outcome measure (cumulative 5-year incidence 69.9% vs. 47.3%, adjusted HR 1.18, 95% CI 0.96–1.44, P=0.11).
Discussion
The main findings of this study evaluating the clinical features and outcomes of severe AS patients with concomitant MR were as follows. (1) The clinical factors associated with moderate/severe MR by multivariable logistic regression analysis included age, low body mass index, prior myocardial infarction, history of HF, history of atrial fibrillation, hemodialysis, and anemia. (2) Concomitant moderate/severe MR was not independently associated with higher risk for the composite endpoint of HF hospitalization and aortic valve-related death regardless of the initial treatment strategy. (3) Among patients with initial AVR strategy, MR improved in all patients who underwent mitral valve surgery, but residual moderate/severe MR was present in 22% of patients who underwent isolated SAVR. However, long-term clinical outcomes were not significantly different between the 2 groups of patients who underwent AVR with and without mitral valve surgery.
The incidence of moderate/severe MR (20%) in our cohort was consistent with previous studies reporting an incidence of 13–33% in patients undergoing SAVR or TAVR.2,3,6
The clinical factors associated with moderate/severe MR by univariate analysis included age, low body mass index, prior myocardial infarction, history of HF, history of atrial fibrillation and renal impairment, which was consistent with our multivariable logistic regression results. Regarding the echocardiographic findings, impaired LV ejection fraction, combined aortic regurgitation, combined TR and higher TR pressure gradient were associated with concomitant moderate/severe MR, in line with the previous reports,16,17
suggesting that the major etiology of concomitant MR was functional.
In the subanalysis of the PARTNER trial, moderate or severe MR coexisted in about 20% of symptomatic severe AS patients. Baseline moderate/severe MR significantly affected mortality at 2 years (HR 1.96, 95% CI 1.26–3.06; P<0.01) in the SAVR population, but baseline moderate/severe MR did not affect mortality at 2 years (HR 1.14, 95% CI 0.72–1.78, P=0.58) in the TAVR population.18
From another meta-analysis including 13 TAVR population studies, preoperative moderate or severe MR was associated with a worse survival rate after TAVR.9
In our study, preoperative moderate/severe MR was not independently associated with worse outcomes in the initial AVR population. In our cohort, 38% of significant MR patients in the initial AVR group underwent a concomitant mitral valve procedure. In contrast, only 5.8% of the PARTNER SAVR cohort underwent mitral valve surgery and residual moderate/severe MR was observed in 30% of that population. Consequently, these differences in therapeutic management might be one of the reasons for the difference between the 2 studies.
On the other hand, little is known about the natural history of severe AS complicated by moderate or severe MR. One retrospective cohort study that included 453 severe AS patients managed medically, reported that patients with concomitant significant (grade 3–4+) MR had worse prognosis, although the multivariate Cox-hazard model did not show a statistically significant difference in mortality.19
We did not find significant excess adjusted risk of moderate/severe MR relative to no/mild MR for the primary outcome measure (composite of aortic valve-related death or hospitalization for HF), suggesting that the worse crude outcomes in patients with moderate/severe MR were not related to the presence of MR per se, but were related to comorbidities associated with MR. The cumulative 5-year incidence of aortic valve-related death was as high as 47% in patients with concomitant moderate/severe MR.
As suggested in the new staging classification of AS, the stage of cardiac damage with extra-aortic valvular conditions strongly affects all-cause death or cardiac death.20
In this classification, left atrial or mitral valve extension of disease is classified as “Cardiac damage stage 2”. A retrospective study showed that cardiac damage stage greater than stage 1 was associated with a significantly higher risk for adverse events (stage 0 vs. stage 2: HR 1.456, 95% CI 1.002–2.118, P=0.049) in symptomatic severe AS.21
Another study reported that cardiac damage stage greater than stage 1 was associated with higher risk for all-cause death (stage 0 vs. stage 2: HR 2.27, 95% CI 1.25–4.12, P=0.007) or for cardiovascular death (stage 0 vs. stage 3–4: HR 5.24, 95% CI 1.79–15.4, P=0.003) in asymptomatic patients with severe AS.22
The association of moderate/severe MR and aortic valve-related death or all-cause death in the present study seems to be in line with this new staging classification of AS severity.
The clinical benefit of routine intervention for the mitral valve at the time of SAVR is still controversial. The operative mortality of combined aortic and mitral valve surgery is about twice as high compared with isolated SAVR.23
Therefore, careful consideration is important for the indications of concomitant mitral valve surgery. A meta-analysis including 17 studies reported that moderate/severe concomitant MR remaining after SAVR affected survival after surgery, but in about 60% of patients who underwent SAVR, untreated concomitant MR improved after isolated SAVR.24
In this setting, residual significant MR might negatively affect patient outcomes. In our study, a relatively high proportion (80%) of patients in whom moderate/severe MR was left untreated had none–mild MR after SAVR without a mitral valve procedure. However, the surgeons in our study decided to perform mitral valve surgery for selected younger patients who had worse cardiac conditions. In addition, there was a relatively higher proportion of moderate MR cases in the moderate/severe MR group (72% in concomitant mitral valve surgery group and 92.5% in no mitral valve surgery group) in our study population. This might be one of the reasons why concomitant mitral valve surgery apparently did not show a significant impact on patients’ outcomes. In general, imaging assessment of the etiology of MR (primary or secondary), the hemodynamic effect of MR, and the patient’s and surgical risks are thought to be important factors in deciding the indication of mitral valve surgery.25
To determine the indication of concomitant mitral valve surgery, the possibility of MR improvement after SAVR is important. In patients undergoing SAVR, degenerative severe MR, preserved LV function, presence of atrial fibrillation, and/or pulmonary hypertension also might be important determinants for concomitant mitral surgery.26
The current study results might have implications for the indications of mitral valve surgery at time of SAVR in patients with severe AS and concomitant MR. This subgroup analysis included a small number of patients, and thus we could not make adjusted comparison between those with and without MV surgery. Moreover, patients who underwent MV surgery had more severe MR than those who did not undergo MV surgery, and the decision to perform MV surgery was left to the experienced cardiovascular surgeon. Therefore, we could not deny serious selection bias in the comparison of outcomes between those with and without MV surgery. Concomitant mitral valve surgery might be beneficial in a specific population that is still to be debated.
Study Limitations
First, due to the retrospective observational nature of this study, selection bias might have affected the choice of initial treatment strategy. Also, there were no formal criteria for surgical intervention for severe AS and concomitant MR, which was left to the discretion of the surgeons. Second, echocardiographic data were site reported, and we did not have a core echocardiography laboratory. Therefore, we cannot deny the possibility of measurement error and variations in the echocardiographic measurement of MR severity. However, echocardiographic measurements were performed according to guidelines by experienced cardiologists and/or ultrasonographers at each participating center. Moreover, the etiology of concomitant MR was not assessed in the present study. Third, serial echocardiographic data after the index assessment were not fully available, so changes in MR severity during the follow-up period were not considered in this study.
Conclusions
Concomitant moderate/severe MR was not independently associated with higher risk for a composite endpoint of HF hospitalization and aortic valve-related death regardless of the initial treatment strategy.
Disclosures
T. Kimura and S. Miyazaki are members of
Circulation Journal’s Editorial Team. The other authors declare no related conflicts of interest.
Sources of Funding
This work was supported by an educational grant from the Research Institute for Production Development (Kyoto, Japan).
IRB Information
This study was approved by the Ethics Committee, Kyoto University, Kyoto, Japan. ID: E1916.
Data Availability
The deidentified participant data will not be shared.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-21-0054
References
- 1.
Iung B, Vahanian A. Epidemiology of valvular heart disease in the adult. Nat Rev Cardiol 2011; 8: 162–172.
- 2.
Nombela-Franco L, Ribeiro HB, Urena M, Allende R, Amat-Santos I, DeLarochelliere R, et al. Significant mitral regurgitation left untreated at the time of aortic valve replacement: A comprehensive review of a frequent entity in the transcatheter aortic valve replacement era. J Am Coll Cardiol 2014; 63: 2643–2658.
- 3.
Alghamdi AA, Elmistekawy EM, Singh SK, Latter DA. Is concomitant surgery for moderate functional mitral regurgitation indicated during aortic valve replacement for aortic stenosis?: A systematic review and evidence-based recommendations. J Card Surg 2010; 25: 182–187.
- 4.
Moazami N, Diodato MD, Moon MR, Lawton JS, Pasque MK, Herren RL, et al. Does functional mitral regurgitation improve with isolated aortic valve replacement? J Card Surg 2004; 19: 444–448.
- 5.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017; 70: 252–289.
- 6.
Wan CK, Suri RM, Li Z, Orszulak TA, Daly RC, Schaff HV, et al. Management of moderate functional mitral regurgitation at the time of aortic valve replacement: Is concomitant mitral valve repair necessary? J Thorac Cardiovasc Surg 2009; 137: 635–640.e631.
- 7.
Vanden Eynden F, Bouchard D, El-Hamamsy I, Butnaru A, Demers P, Carrier M, et al. Effect of aortic valve replacement for aortic stenosis on severity of mitral regurgitation. Ann Thorac Surg 2007; 83: 1279–1284.
- 8.
Barreiro CJ, Patel ND, Fitton TP, Williams JA, Bonde PN, Chan V, et al. Aortic valve replacement and concomitant mitral valve regurgitation in the elderly: Impact on survival and functional outcome. Circulation 2005; 112: I443–I447.
- 9.
Sannino A, Losi MA, Schiattarella GG, Gargiulo G, Perrino C, Stabile E, et al. Meta-analysis of mortality outcomes and mitral regurgitation evolution in 4,839 patients having transcatheter aortic valve implantation for severe aortic stenosis. Am J Cardiol 2014; 114: 875–882.
- 10.
Nombela-Franco L, Eltchaninoff H, Zahn R, Testa L, Leon MB, Trillo-Nouche R, et al. Clinical impact and evolution of mitral regurgitation following transcatheter aortic valve replacement: A meta-analysis. Heart 2015; 101: 1395.
- 11.
Taniguchi T, Morimoto T, Shiomi H, Ando K, Kanamori N, Murata K, et al. Initial surgical versus conservative strategies in patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol 2015; 66: 2827–2838.
- 12.
Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003; 16: 777–802.
- 13.
Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: A report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr 2017; 30: 303–371.
- 14.
Leon MB, Piazza N, Nikolsky E, Blackstone EH, Cutlip DE, Kappetein AP, et al. Standardized endpoint definitions for transcatheter aortic valve implantation clinical trials: A Consensus Report from the Valve Academic Research Consortium. J Am Coll Cardiol 2011; 57: 253–269.
- 15.
Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: The Valve Academic Research Consortium-2 consensus document. J Am Coll Cardiol 2012; 60: 1438–1454.
- 16.
Caballero-Borrego J, Gómez-Doblas JJ, Cabrera-Bueno F, García-Pinilla JM, Melero JM, Porras C, et al. Incidence, associated factors and evolution of non-severe functional mitral regurgitation in patients with severe aortic stenosis undergoing aortic valve replacement. Eur J Cardiothorac Surg 2008; 34: 62–66.
- 17.
Gómez-Doblas JJ, López-Garrido MA, Becerra-Muñoz VM, Orellana-Figueroa HN, Carro Hevia A, García de la Villa B, et al. Significant mitral regurgitation worsens the prognosis and favors the decision of conservative treatment in octogenarians with severe symptomatic aortic stenosis. Eur J Intern Med 2018; 55: 40–46.
- 18.
Barbanti M, Webb John G, Hahn Rebecca T, Feldman T, Boone Robert H, Smith Craig R, et al. Impact of preoperative moderate/severe mitral regurgitation on 2-year outcome after transcatheter and surgical aortic valve replacement. Circulation 2013; 128: 2776–2784.
- 19.
Varadarajan P, Kapoor N, Bansal RC, Pai RG. Clinical profile and natural history of 453 nonsurgically managed patients with severe aortic stenosis. Ann Thorac Surg 2006; 82: 2111–2115.
- 20.
Généreux P, Pibarot P, Redfors B, Mack MJ, Makkar RR, Jaber WA, et al. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur Heart J 2017; 38: 3351–3358.
- 21.
Vollema EM, Amanullah MR, Ng ACT, van der Bijl P, Prevedello F, Sin YK, et al. Staging cardiac damage in patients with symptomatic aortic valve stenosis. J Am Coll Cardiol 2019; 74: 538–549.
- 22.
Tastet L, Tribouilloy C, Maréchaux S, Vollema EM, Delgado V, Salaun E, et al. Staging cardiac damage in patients with asymptomatic aortic valve stenosis. J Am Coll Cardiol 2019; 74: 550–563.
- 23.
Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003; 24: 1231–1243.
- 24.
Harling L, Saso S, Jarral OA, Kourliouros A, Kidher E, Athanasiou T. Aortic valve replacement for aortic stenosis in patients with concomitant mitral regurgitation: Should the mitral valve be dealt with? Eur J Cardiothorac Surg 2011; 40: 1087–1096.
- 25.
O’Gara PT, Grayburn PA, Badhwar V, Afonso LC, Carroll JD, Elmariah S, et al. 2017 ACC Expert Consensus Decision Pathway on the Management of Mitral Regurgitation: A report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol 2017; 70: 2421–2449.
- 26.
Khan F, Okuno T, Malebranche D, Lanz J, Praz F, Stortecky S, et al. Transcatheter aortic valve replacement in patients with multivalvular heart disease. JACC Cardiovasc Interv 2020; 13: 1503–1514.