2023 年 87 巻 11 号 p. 1672-1679
2023 年 87 巻 11 号 p. 1672-1679
Background: The relationships between preoperative fractional flow reserve (FFR) values of the left anterior descending artery (LAD), FFRLAD, and intraoperative transit time flow measurement (TTFM) variables in coronary artery bypass grafting (CABG) remain unclear.
Methods and Results: We retrospectively collected data for 74 in situ left internal thoracic artery (LITA) grafts and 27 saphenous vein grafts (SVGs) to the LAD that were shown to be patent on postoperative angiography. Spearman correlation coefficients were determined between FFRLAD and TTFM parameters of the LITA graft, as follows: maximum flow (Qmax), −0.22 (P=0.077); minimum flow (Qmin), −0.40 (P=0.014); mean flow (Qm), −0.35 (P=0.039); pulsatility index (PI), 0.33 (P=0.008); diastolic filling (DF): 0.01 (P=0.83); and systolic reverse flow (SRF), 0.37 (P=0.002). Spearman correlation coefficients between FFRLAD and TTFM parameters of the SVG to LAD were: Qmax, −0.65 (P=0.004); Qmin, −0.43 (P=0.044); Qm, −0.75 (P=0.001); PI, 0.53 (P=0.033); DF, 0.14 (P=0.48); and SRF, 0.61 (P=0.009).
Conclusions: Both LITA grafts and SVGs to the LAD show negative correlations for FFRLAD with Qmin and Qm, but positive correlations for FFRLAD with PI and SFR. These relationships between FFRLAD and TTFM variables of CABG grafts to the LAD should be recognized.
Fractional flow reserve (FFR), an index calculated by dividing the distal coronary pressure by the proximal pressure measured under conditions of maximum hyperemia, has been well validated as a determinant of lesion-specific myocardial ischemia from epicardial coronary artery disease.1,2 An FFR threshold ranging from 0.75 to 0.80 is used to distinguish functionally significant coronary artery stenosis.3 The FFR Versus Angiography for Multivessel Evaluation (FAME) study demonstrated the superiority of FFR-guided percutaneous coronary intervention (PCI) to conventional angiography-guided PCI.2 Furthermore, the subsequent FAME-2 trial showed that FFR-guided PCI surpasses medical therapy alone,4 primarily by prudently deferring treatment for lesions that may appear stenotic but do not result in lesion-specific ischemia according to FFR measurements. Therefore, current guidelines recommend the use of FFR to complement coronary angiography.5,6 Under these circumstances, the strategy of coronary artery bypass grafting (CABG) is also shifting to FFR guidance, although its advantage over angiography-guided CABG remains undetermined.3
To validate the roles of FFR in CABG, our investigation aimed to assess the impact of preoperative FFR values of the target left anterior descending artery (LAD), referred to as FFRLAD, on the intraoperative transit time flow measurement (TTFM) of both in situ left internal thoracic artery (LITA) grafts and aortocoronary saphenous vein grafts (SVGs). The aim of this study was to gain a better understanding of TTFM analysis of CABG graft flow, which is recommended in the European guidelines,7,8 as a less invasive, more highly reproducible, and less time-consuming method.
This retrospective study, using clinical data from routine medical practice for CABG patients, was approved by the Fujita Health University Ethics Committee (HM19-323, October 15, 2019), including a waiver for the need for informed consent for the retrospective use of patient data. The study was conducted according to the ethical guidelines for clinical studies published by the Ministry of Health9 and in accordance with the Declaration of Helsinki.
Study PatientsThis study enrolled 101 patients who received CABG grafts to the LAD (74 in situ LITA grants and 27 SVGs; 12.1% of all patients undergoing CABG between 2014 and 2022). Patients were included if they fulfilled the following requirements (Figure 1): preoperative measurements were made of the FFRLAD to determine the indication for CABG; intraoperative TTFM data were obtained; postoperative patency of the graft was confirmed by multislice computed tomography angiography (MSCTA); and no ischemia in the LAD area was identified on postoperative stress myocardial perfusion scintigraphy.

Flowchart showing the inclusion criteria for the study patients. CABG, coronary artery bypass grafting; FFR, fractional flow reserve; LAD, left anterior descending artery; LITA, in situ left internal thoracic artery graft; MSCTA, multislice computed tomography angiography; TTFM, transit time flow measurement.
Our first choice of a graft to the LAD is an in situ LITA, as recommended by many guidelines. However, we used an SVG to the LAD when competitive flow due to less severe stenosis of the LAD may lead to the occurrence of the “string phenomenon” of a LITA graft to the LAD. In addition, we used an SVG to the LAD when the concomitant surgical procedures were complex, such as aortic arch replacement.
Preoperative FFR MeasurementMeasurements of FFR were made only in patients with moderate coronary luminal stenosis on coronary angiography to decide the indication for CABG. Intracoronary pressure was measured using a 0.014-inch pressure guide wire (PressureWire Aeris; St Jude Medical, Inc., St Paul, MN, USA). The proximal and distal coronary pressures were recorded by the guiding catheter. The FFR was calculated as the mean distal coronary pressure divided by the mean aortic pressure during maximum hyperemia induced by intravenous continuous infusion of adenosine at a rate of 150–180 mg/kg/min. An FFR ≤0.80 indicates an ischemia-producing stenosis that needs revascularization.10
Intraoperative TTFMIsolated or concomitant CABG procedures were performed with or without cardiopulmonary bypass. An in situ LITA graft or aortocoronary SVG was used as a bypass graft to the LAD area. Neither Y nor sequential grafting was used for the graft to the LAD.
A flow probe of 3 or 4 mm was placed around the graft for measurement of intraoperative TTFM (Medi-Stim, Oslo, Norway). We routinely obtain the flow profile with TTFM twice: (1) just after graft anastomosis during off-pump CABG or on-pump beating-heart CABG, or just after the aortic declamp during on-pump cardioplegic arrest CABG, to judge the need for graft revision; and (2) when the hemodynamic condition becomes stable before chest closure, with a mean blood pressure of 70–90 mmHg and a heart rate of 80–100 beats/min.
The following TTFM variables were calculated: maximum flow (Qmax; mL/min); minimum flow (Qmin; mL/min); mean flow (Qm; mL/min); pulsatility index (PI), where PI = (Qmax − Qmin) / Qm; diastolic filling (DF), where DF = 100 × ∫diastolic flow (Qd) / (∫systolic flow (Qs) + ∫Qd) systolic reverse flow (SRF), where SRF=volume of backward flow/volume of forward flow; and the fast Fourier transformation (FFT) ratio.11 The FFT ratio is calculated as F0/H1, where F0 is a power of the fundamental frequency and H1 is a power of the first harmonic on the FFT analysis of the blood flow curve.12 FFT analysis is based upon the principal that all periodic waveforms can be broken down into a series of pure sine waves or harmonics. Harmonics exist at frequencies that are multiplies of the fundamental frequency and are described in terms of an amplitude and phase.13,14
Postoperative EvaluationFor postoperative graft evaluation, every patient underwent cardiac imaging with MSCTA approximately 2 months after CABG as a routine checkup, using a β-blocker and isosorbide mononitrate to ensure the adequacy of images. In addition, every patient routinely underwent adenosine stress and rest myocardial perfusion scintigraphy approximately 2 months after CABG, using adenosine infused at a rate of 0.14 mg/kg/min for 6 min and 111–148 MBq of Thallium-201 administered 3 min before the end of the adenosine infusion. Single photon emission computed tomography images were then acquired 5 min later. Rest-redistribution scans were obtained after 4 h. Six segments, including the anteroseptal area perfused by the LITA graft or SVG to the LAD, were analyzed in the left ventricular short-axis image at the papillary muscle level.
Statistical AnalysisCategorical data are presented as either a number or a percentage; continuous data are presented as the mean±SD. Mann-Whitney tests were used to compare 2 continuous variables. Fisher’s exact tests were used to compare 2 categorical variables. A correlation analysis was performed between the intraoperative TTFM parameters and preoperative FFRLAD using Pearson correlation coefficients, based on the linearity of the relationship between quantitative variables. One-tailed P<0.05 was considered statistically significant. All statistical analyses were performed using SPSS 18 (IBM Corporation, Armonk, NY, USA).
As indicated in the Table, there were no significances in patient characteristics between those receiving LITA grafts and SVGs, except for the following 4 characteristics: diabetes was more prevalent in the LITA-LAD group, peripheral artery disease was more prevalent in the SVG-LAD group, left ventricular end-diastolic dimension was larger in the SVG-LAD group, and isolated CABG was more frequently performed in the LITA-LAD group while concomitant procedures were more frequently performed, especially total arch replacement, in the SVG-LAD group.
Patient Characteristics
| LITA graft to LAD (n=74) |
SVG to LAD (n=27) |
P value | |
|---|---|---|---|
| Age (years) | 68±9 | 71±10 | 0.06 |
| Male sex | 52 (70) | 21 (78) | 0.32 |
| Hypertension | 65 (88) | 23 (85) | 0.47 |
| Hypercholesterolemia | 55 (74) | 15 (56) | 0.06 |
| Diabetes | 46 (62) | 6 (22) | 0.0004 |
| Smoking habit | 38 (51) | 18 (67) | 0.13 |
| Pulmonary disease | 14 (19) | 7 (26) | 0.31 |
| Previous MI | 13 (18) | 3 (11) | 0.33 |
| Chronic kidney disease | 35 (47) | 12 (44) | 0.49 |
| Previous stroke | 10 (14) | 3 (11) | 0.52 |
| Peripheral artery disease | 18 (24) | 12 (44) | 0.045 |
| Left ventricular | |||
| End-diastolic dimension (mm) | 49.6±7.7 | 53.6±9.6 | 0.029 |
| End-systolic dimension (mm) | 36.1±9.8 | 39.3±12.9 | 0.12 |
| Ejection fraction | 0.52±0.12 | 0.51±0.13 | 0.38 |
| Isolated CABG | 51 (69) | 3 (11) | 0.0001 |
| Off-pump | 12 (16) | 0 | |
| On-pump | 39 (53) | 3 (11) | |
| Concomitant CABG with | 23 (31) | 24 (89) | 0.0001 |
| Mitral valve repair | 6 (8.1) | 4 (15) | |
| AVR | 11 (15) | 8 (30) | |
| AVR+hemiarch replacement | 3 (4.1) | ||
| MVR | 1 (1.4) | ||
| AVR+MVR | 1 (1.4) | 2 (7.4) | |
| Aortic root surgery | 1 (1.4) | 2 (7.4) | |
| Total arch replacement | 7 (26) | ||
| Cardiac tumor resection | 1 (3.7) | ||
Unless indicated otherwise, data are given as the mean±SD or n (%). AVR, aortic valve replacement; CABG, coronary artery bypass grafting; LAD, left anterior descending artery; LITA, in situ left internal thoracic artery; MI, myocardial infarction; MVR, mitral valve replacement; SVG, saphenous vein graft.
All patients were free from perioperative myocardial infarction, based on electrocardiographic changes and serum biomarkers. The postoperative course for all patients was uneventful, with a median hospital stay of 14 days. Postoperative MSCTAs demonstrated patent in situ LITA-LAD and SVG-LAD in all study patients. Postoperative myocardial perfusion scintigraphy also demonstrated no ischemia in the LAD area for all study patients.
FFR and TTFM VariablesAs shown in Figure 2, the FFRLAD for the LITA graft to the LAD was significantly negatively correlated with Qmin (r=−0.40; P=0.014) and Qm (r=−0.35; P=0.039), but significantly positively correlated with PI (r=0.33; P=0.008) and SRF (r=0.37; P=0.002). The FFRLAD for the LITA graft to the LAD was not correlated with Qmax, DF, or the FFT ratio.
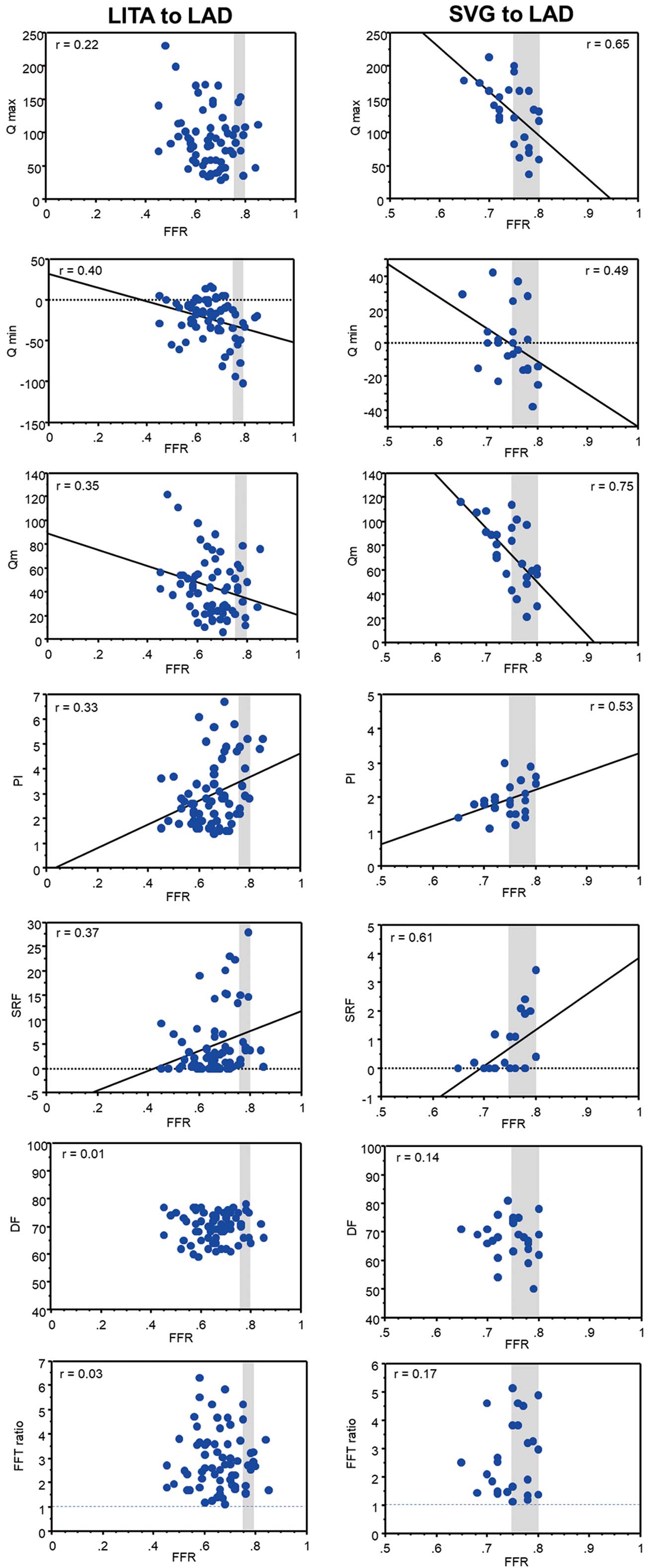
Correlations of the preoperative fractional flow reserve (FFR) of the left anterior descending artery (LAD) and the parameters of intraoperative transit time flow measurement (TTFM) of the in situ left internal thoracic artery (LITA) graft and saphenous vein graft (SVG) to the LAD. DF, diastolic filling; FFT, fast Fourier transformation; PI, pulsatility index; Qmax, maximum flow; Qmin, minimum flow; Qm, mean flow; SRF, systolic reverse flow.
As also shown in Figure 2, the FFRLAD for the SVG to LAD was significantly negatively correlated with Qmax (r=−0.65, P=0.004), Qmin (r=−0.43, P=0.044), and Qm (r=−0.75, P=0.001), but significantly positively correlated with PI (r=0.53; P=0.033) and SRF (r=0.61; P=0.009). The FFRLAD for the SVG to LAD was not correlated with DF and the FFT ratio.
In summary, both LITA grafts and SVGs to the LAD showed negative correlations of FFRLAD with Qmin and Qm, but positive correlations of FFRLAD with PI and SFR.
Representative CasesFigure 3 shows the intraoperative TTFM of the LITA graft to the LAD with an FFRLAD of 0.72 in a 58-year-old male patient undergoing isolated CABG. All TTFM parameters showed good values and the FFT analysis also showed a gradually attenuating waveform with an FFT ratio of 3.6. Postoperative MSCTA showed the patent LITA, and no ischemia was found at the LAD area on stress myocardial scintigraphy.

Upper panels show the intraoperative transit time flow measurement (TTFM) of an in situ left internal thoracic artery (LITA) graft to the left anterior descending artery (LAD) with a preoperative fractional flow reserve (FFR) of 0.72 in a 58-year-old male patient undergoing isolated coronary artery bypass grafting (CABG). All TTFM parameters show good values, including maximum flow (Qm) of 96 mL/min, a pulsatility index (PI) of 1.9, systolic reverse flow (SFR) of 0.2%, diastolic filling (DF) of 75%, and a fast Fourier transformation (FFT) ratio of 3.5. A patent LITA is shown on postoperative multislice computed tomography angiography (MSCTA) and no ischemia is found at the LAD area on stress myocardial scintigraphy. Lower panels show the intraoperative TTFM of an in situ LITA graft to the LAD with a preoperative FFR of 0.79 in a 78-year-old male patient undergoing isolated CABG. The Qmin and Qm are as low as −28 and 13 mL/min, respectively, and PI and SFR are as high as 4.5 and 15%, respectively. However, the FFT analysis showed a gradually attenuating waveform with an FFT ratio of 3.2. Although the postoperative MSCTA shows a patent LITA graft with a narrow diameter, no ischemia was found in the LAD region on stress myocardial scintigraphy.
Figure 3 also shows the TTFM of the LITA graft to the LAD with a higher FFRLAD of 0.79, in a 78-year-old male patient undergoing isolated CABG. The Qmin and Qm are as low as −28 and 13 mL/min, respectively, whereas the PI and SFR are as high as 4.5 and 15%, respectively. However, the FFT analysis provided a gradually attenuating waveform with an FFT ratio of 3.2. Although the postoperative MSCTA showed a patent LITA graft with a narrow diameter, no ischemia was found in the LAD area on stress myocardial scintigraphy.
Figure 4 shows the intraoperative TTFM of an SVG to the LAD with an FFRLAD of 0.72 in a 78-year-old male patient undergoing total arch replacement and CABG. All TTFM parameters showed acceptable values and a gradually attenuating waveform on FFT analysis, with an FFT ratio of 1.8. Postoperative MSCTA showed a patent SVG, and no ischemia was found at the LAD area on stress myocardial scintigraphy.

Upper panels show the intraoperative transit time flow measurement (TTFM) of the saphenous vein graft (SVG) to the left anterior descending artery (LAD) with a preoperative fractional flow reserve (FFR) of 0.72 in a 78-year-old male patient undergoing total arch replacement and coronary artery bypass grafting (CABG). All TTFM parameters show good values, including maximum flow (Qm) of 90 mL/min, a pulsatility index (PI) of 1.1, systolic reverse flow (SFR) of 0%, diastolic filling (DF) of 68%, and a fast Fourier transformation (FFT) ratio of 1.8. Postoperative multislice computed tomography angiography (MSCTA) show a patent SVG, and no ischemia is found at the LAD area on stress myocardial scintigraphy. Lower panels show the intraoperative TTFM of the SVG to the LAD with a preoperative FFR of 0.78 in a 79-year-old male patient undergoing aortic valve replacement and CABG. The Qmin is −25 mL/min, Qm is 43 mL/min, PI is 2.4, and SFR is 3.4%. However, the FFT analysis showed a gradually attenuating waveform with an FFT ratio of 1.1. Postoperative MSCTA shows a patent SVG, and no ischemia is found at the LAD area on stress myocardial scintigraphy.
Figure 4 also shows the TTFM of an SVG to the LAD with a gray-zone FFRLAD of 0.78 in a 79-year-old male patient undergoing aortic valve replacement and CABG. Although reversal flow is larger, because Qmin was −25 mL/min and SFR was 3.4%, the FFT analysis showed a gradually attenuating waveform with an FFT ratio of 1.1.
The main findings of our analysis of the in situ LITA graft and SVG to the LAD are as follows:
1. Most of the TTFM variables of both the LITA graft and SVG are strongly affected by preoperative FFRLAD values, including Qmin, Qm, PI, and SFR, which have been used as good indicators to evaluate the quality of the CABG anastomosis.
2. For both LITA grafts and SVGs, the FFT ratio is an independent TTFM variable that is not influenced by FFRLAD.
FFR-Guided CABGOur main findings may be important in the current era, in which FFR-guided CABG is receiving growing attention, despite no evidence to support improved clinical outcomes.15–21 However, we should keep in mind that the relative benefits of CABG compared with PCI may be lost with the consequences of a shift towards FFR-guided CABG, which reduces the number of vessels grafted and increases the rate of anatomically defined incomplete revascularization.
FFR and TTFM VariablesIn addition to morphological assessment using color Doppler, Qm >15 mL/min, PI <5.0, DF >50%, SRF <4%, and an FFT ratio >1.0 are TTFM variables indicative of a patent graft during CABG.11,22 However, these variables vary with hemodynamic factors, as well as anastomotic quality. Honda et al23 reported significantly lower Qm and higher PI of the LITA graft to the LAD with an FFR ≥0.75 compared with LITA grafts to the LAD with FFR <0.75. We have also reported that most TTFM variables of the LITA graft to the LAD are strongly affected by FFRLAD.24 In the present study, we have revealed similar correlations between FFRLAD values and Qmin, Qm, PI, and SFR of the SVG to the LAD.
We observed no correlations of FFRLAD with DF defined by the equation DF = 100 × ∫Qd / (∫Qs + ∫Qd), although DF may be an independent predictor of failed anastomosis.25 By identifying changes in the diastolic-delivered blood volume vs. total delivered blood volume, DF can quantify the gradual shift from diastolic to systolic dominance with increasing occlusion observed in the CABG flow rate waveform.26 However, when systolic reversal graft flow to the LAD with higher FFRLAD occurs, ∫Qs is negative, therefore leading to an inaccurate DF value on the TTFM machine. To obtain accurate DF values, the negative ∫Qs should be substituted with its absolute value, ∫|Qs |.
Unaffected TTFM VariablesIt is noted that the FFT ratio11–14,24 is an independent TTFM index unaffected by FFRLAD. Mao et al14 demonstrated the application of FFT analysis in assessing CABG flow using multiscale models of a 3-dimensional LITA-LAD graft with varying degrees of stenosis in the LAD, resulting in different magnitudes of competitive flows. Their in vitro findings indicated that an FFT ratio >1.0 is maintained for patent LITA-LAD grafts regardless of the degree of stenosis, as shown in the present study. Therefore, FFT analysis of the TTFM flow curve may be recommended for grafts to the LAD with a higher FFRLAD (>0.75). When the FFT ratio is ≥1.0, even if other TTFM variables are suboptimal, the graft anastomosis can be considered satisfactory, and the surgical indication for revascularization is not adequate. Conversely, an FFT ratio <1.0 suggests a potential issue with the anastomosis, necessitating consideration of graft revision.
Clinical PerspectivesThe following perspectives are derived from the close relationships between FFRLAD and TTFM variables of grafts to the LAD, as shown in the present study:
1. When judging the CABG anastomosis by intraoperative TTFM, as recommended in the guidelines,5 the influence of the preoperative FFR should be taken into account to avoid inadvertent re-anastomosis or revision of the grafts due to a poor TTFM variable.
2. As shown in Figure 2, SVGs show more beneficial TTFM variables, higher Qm, lower PI, and lower SFR, than LITA grafts to the LAD with the gray-zone FFRLAD. Although the long-term patency is limited, SVGs may be better as a conduit to the gray-zone LAD with 0.75<FFRLAD<0.80. As Sabik et al reported, grafting moderately stenosed coronary arteries with an SVG does not affect long-term mortality.27 In addition, we expect long-term patency of the SVG to the LAD with gray-zone FFR with the no-touch harvesting technique, as reported by Samano et al.28
Study LimitationsThe present study has several limitations. First, we retrospectively collected the data of a small number of patients from a single center, meaning that the study was susceptible to potential sources of bias. Second, this study included a highly selected portion of CABG patients with patent grafts and the patients undergoing CABG using SVGs with concomitant aortic valve replacement. Although the effect of the turbulence of downstream prosthetic aortic valves on SVGs anastomosed to the ascending aorta has not been adequately studied, Hassanein et al reported that the flow in SVGs in patients with biological valves was higher than in those with the mechanical valve.29 Third, we used MSCTA for postoperative graft assessment, which cannot evaluate “to and fro” flow competition of the LITA graft when compared with coronary angiography. Intraoperative epicardial ultrasound or indocyanine green angiography may be an alternative to check the anastomosis site. Fourth, because graft flow is sensitive to many parameters, including hemodynamics, diabetes and female sex, endothelial dysfunction and altered resistance distal to the coronary lesions, efforts to control for these variables in a regression model rather than a simple linear correlation may help clarify the nature and strength of the relationship. Fifth, most TTFM variables analyzed showed a relatively low intensity of correlation with FFR, although the correlation was statistically significant.
Most TTFM variables of both in situ LITA grafts and SVGs to the LAD during CABG are strongly affected by preoperative FFRLAD values, including Qmin, Qm, PI, and SFR, which have been used as good indicators to evaluate the quality of the anastomosis. Because the FFT ratio is not influenced by FFR, FFT analysis of the TTFM results may be recommend for both the in situ LITA graft and SVG to the LAD. It is imperative to recognize such relationships between FFRLAD and TTFM variables of CABG grafts to the LAD.
The authors have received no financial support for the research, authorship, and publication of this article.
The authors have no conflicts of interest to disclose.
This study was approved by the Ethics Committee of Fujita Health University (No. HM19-323; date of approval, October 15, 2019).