論文ID: CJ-14-1088
論文ID: CJ-14-1088
The Annual Congress of the European Society of Cardiology (ESC) was held in Barcelona from 30th August to 3rd September 2014. More than 30,300 attendees from around the world shared the latest original research, including 27 clinical Hot Line studies, 12 basic science Hot Lines, 15 clinical trial updates, 19 registry studies, and 4,597 abstracts. Many important issues were presented, including novel treatment strategies for heart failure, acute coronary syndrome, interventional treatment for structural heart disease, renal denervation, novel anticoagulant therapies, atrial fibrillation and so on. In addition, 5 new ESC clinical practice guidelines (ie, myocardial revascularization, non-cardiac surgery, acute pulmonary embolism, hypertrophic cardiomyopathy, and aortic disease) were launched. It should be noted that Japan has recently been ranked in the top position in terms of the number of abstract submissions. Based on these activities, the ESC Congress has been recognized as the dominant scientific and educational forum for healthcare professionals in cardiology. We report the highlights and several key presentations of the ESC Congress 2014. The scientific activities and growing contributions of Japanese cardiologists or cardiovascular surgeons enhance the favorable relationship between the ESC and the Japanese Circulation Society.
The European Society of Cardiology (ESC) is a non-profit organization that facilitates the improvement and harmonization of diagnostic and therapeutic standards of cardiovascular diseases. The ESC was founded in 1950 and its headquarters are located at Sophia Antipolis in Nice, France. The ESC currently comprises 55 national cardiac societies from across Europe and the Mediterranean region, 6 associations, 18 working groups and 5 councils, covering different subspecialties of cardiology. Activities reach far beyond the boundaries of Europe, and the ESC has approximately 80,000 members worldwide. The ESC also maintains close ties to 36 affiliated cardiac societies worldwide. The official journal of the ESC, the European Heart Journal, has increased its impact factor from 8.9 in 2008 to 14.723 in 2014, which translates into more attention being given to this journal.
The first European Congress of Cardiology was held in London in September 1952, and it has now become the ESC Congress, one of the largest annual medical meetings around the world. This year the ESC Congress was held at Fira Gran Via in Barcelona, Spain from the 30th August to 3rd September 2014 (Figure 1), led by Professor Panos Vardas (President) and Professor Keith Fox (Chair of the Congress Programme Committee). More than 30,300 attendees joined this congress and shared their latest original research, including 27 clinical Hot Line studies, 12 basic science Hot Lines, 15 clinical trial updates, 19 registry studies, and 4,597 abstracts. It should be noted that a total of 1,806 abstracts were submitted from Japan this year, making it the top country in terms of total number of scientific abstract submissions (Figure 2). Herewith we express our sincere appreciation to the Japanese Circulation Society (JCS) members for their tremendous contributions activating the ESC Congress 2014 on behalf of the ESC contact doctors (Professors Hiroaki Shimokawa, Takashi Akasaka, and Yukio Ozaki), the Chairman of the International Committee (Professor Issei Komuro), and The president of the JCS (Professor Hisao Ogawa).

The “Fira Gran Via” congress center venue of the European Society of Cardiology Congress 2014 in Barcelona. (A) Main entrance and (B) reception hall. There were many attractive sessions, including the Hot Line topics (C) and “Meet the Legends” with Professor Eugene Braunwald (D).

Distributions and changes in the number of (abstract submissions) abstract submissions to the European Society of Cardiology Congress from 2009 to 2014. Bar graph shows the number of abstract submissions from the top 10 countries in 2014. A dramatic increase in abstract submissions from Japan, reaching 1,806 abstracts in 2014, is noted.
We report the highlights and several key presentations from the ESC Congress 2014.
Professor Hiroaki Shimokawa (Tohoku University Graduate School of Medicine, Sendai, Japan) provided an overview of his translational research regarding coronary spasm (Figure 3). He demonstrated his basic research indicating that Rho-kinase plays a crucial role in coronary spasm and downregulates the endothelial nitric oxide synthase, which appears to be responsible for dilating microvascular resistance as an underlying substrate.1,2 In the clinical studies, he showed that a selective Rho-kinase inhibitor (ie, Fasudil) prevented myocardial ischemia in patients with coronary spasm.3,4 Rho-kinase activity in circulating neutrophils could also be a useful biomarker in terms of diagnosis and assessment of disease activity in patients with vasospastic angina.5 He also developed risk models for predicting adverse cardiac events using several predictors found in data from the Japanese Coronary Spasm Association, which included approximately 1,500 patients with coronary spasm.6
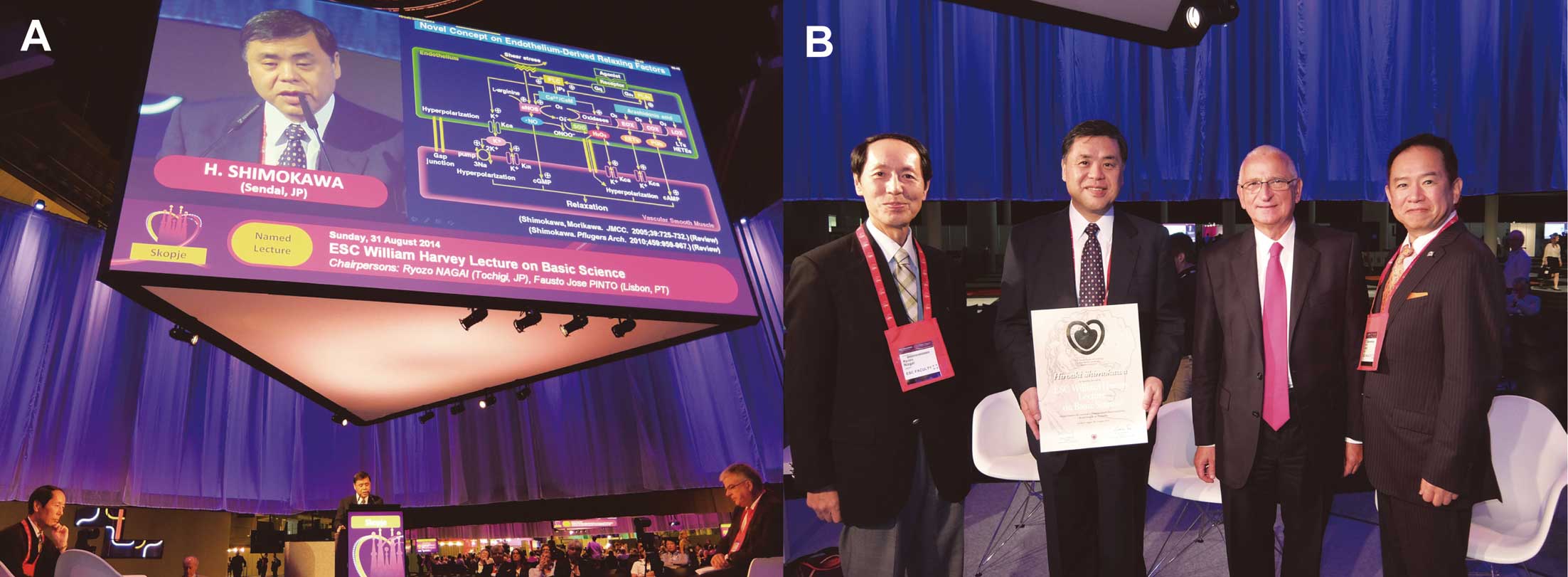
Prosessor Hiroaki Shimokawa (Tohoku University, Sendai, Japan) presenting the importance of coronary vasomotion abnormalities from bench to bedside in the William Harvey Lecture on Basic Science chaired by Professors Ryozo Nagai (left) and Fausto Pinto (right) (A). From left to right, Professors Ryozo Nagai (chair), Hiroaki Shimokawa, Michel Komajda (the former ESC President) and Yukio Ozaki who introduced the outline of Professor Shimokawa’s achievements in advance to his presentation (B).
This year Professor Adnan Kastrati (Deutsches Herzzentrum, Munich, Germany) recalled his scientific contributions to improving stent technologies and the clinical outcomes with respect to restenosis and stent thrombosis. Through the Intracoronary Stenting and Antithrombotic Regimen (ISAR) series of studies launched in 1994,7 he has supervised more than 50 randomized controlled trials involving over 45,000 patients with the overall objective of determining optimal PCI strategies using stents. Having demonstrated the clinical efficacies of drug-eluting stent (DES) technologies, he presented the current PRESTIGE (PREvention of Late Stent Thrombosis by an Interdisciplinary Global European effort) project examining the mechanisms responsible for late and very late stent thrombosis. This project also includes basic research to elucidate the molecular and cellular mechanisms underlying stent thrombosis, a bioengineering approach to assessing new intracoronary imaging techniques, and a clinical approach exploring the risks in predicting stent thrombosis.
René Laënnec LectureProfessor Gaetano Thiene (University of Padua Medical School, Padua, Italy) is an Italian cardiopathologist who gave a lecture about his translational research related to arrhythmogenic right ventricular cardiomyopathy (ARVC) and the discovery of culprit genes encoding proteins at cell junctions. His work was successfully published and led to the establishment of ARVC as a major cause of sudden death in the young.8 He found that cardiomyocytes that are not firmly attached in ARVC results in cell death and their replacement with fibro-fatty tissue, which finally interferes with electrical impulses. He also discovered defective genes and has moved onto new avenues of research, including experiments in mice models.9
This year the ESC Gold Medals were awarded to 3 outstanding cardiologists: Sir Rory Collins, Petr Widimský, and Alain Carpentier (Figure 4).
Gold Medal award presentation at the European Society of Cardiology Congress 2014 (A) and 3 of the awardees (B): from left to right, Professor Sir Rory Collins (Oxford, UK), Professor Alain Carpentier (Paris, France), and Professor Petr Widimský (Prague, Czech Republic).
Professor Collins is a distinguished epidemiologist and has significantly contributed to advances in lipid-lowering therapies. It is now more than a decade since the Heart Protection Study showed that lowering the levels of LDL-cholesterol in a wide range of patients with prior vascular disease or diabetes, irrespective of their index cholesterol level, would lower their risk of subsequent cardiovascular events.10,11 Surprisingly, the vascular mortality rates in middle age have remarkably fallen by more than half in the past 3 decades in the UK. He has been a director of the Clinical Trial Service Unit that has made a substantial contribution to these trends in its major studies of statins as well as blood pressure, aspirin and streptokinase.
Professor Petr Widimský (Prague, Czech Republic)Professor Widimský is an interventional cardiologist who has arguably done more than anyone to promote primary PCI through his series of PRAGUE studies and the ESC’s “Stent for Life” initiative. There is an element of nostalgia in his return to Barcelona, for it was in exactly the same place at the ESC Congress 1999 in which he presented his landmark PRAGUE 1 study, showing the superiority of primary PCI over thrombolysis in acute MI patients. Following studies confirmed this result and thereby fully convinced the community of the benefits of primary PCI as the default perfusion strategy.12 To date, 19 different PRAGUE studies have been launched, with the last one, namely PRAGUE 19, aiming to evaluate the safety and efficacy of the everolimus-eluting bioresorbable vascular scaffold for STEMI patients, also presented at this congress.13
Professor Alain Carpentier (Paris, France)Professor Carpentier is the “father” of modern mitral valve repair, the Carpentier-Edwards heart valve, and more recently the first bioprosthetic artificial heart. His current endeavor is to develop a bioprosthetic artificial heart as a permanent implant not just as a “bridge” to transplant.14,15 The CARMAT device combines animal tissue with sensor technology adapted from guided missiles. The device, which can be totally implanted within the patient’s pericardial sac, has sensors to detect increased pressure, allowing internal control systems to adjust blood flow during exercise. The first-in-human implantation of this device was performed in December 2013.
Statins have been shown to slightly increase the risk of new-onset diabetes, but few studies have been conducted to investigate their effect on existing diabetes. Lipid lowering with highly potent statins in hyperlipidemia with type 2 diabetes patients (LISTEN) trial was presented by Professor Hisao Ogawa (Kumamoto University Graduate School of Medical Sciences, Kumamoto, Japan) (Figure 5). This study randomized patients with type 2 diabetes and hypercholesterolemia to either rosuvastatin 5 mg daily (n=514) or atorvastatin 10 mg daily (n=504) as the standard doses used in clinical practice in Japan. An increase in each statin dose according to Japanese guidelines was allowed only when the cholesterol level was uncontrollable. The primary endpoint was the change in levels of non-HDL cholesterol and glycosylated hemoglobin between pretreatment and up to 1 year. At the end of the study, both groups revealed a reduction in non-HDL cholesterol level without statistically significant difference (−32.86% in the rosuvastatin group vs. −31.01% in the atorvastatin group, respectively). Similarly, the change in LDL-cholesterol level was not significantly different between the groups at 1 year (−34.79% vs. −32.78%). At 3 months, however, the reduction in LDL-cholesterol level was significantly greater in the rosuvastatin group than in the atorvastatin group (−39.38% vs. −36.39%, P=0.0106). Blood glucose levels increased in both groups without significant difference at 1 year (mean change: 0.11% in the rosuvastatin group, 0.12% in the atorvastatin group). In addition, the initial increase in blood glucose was more abrupt in the atorvastatin group (121.4 and 126.0 mg/dl at 3 and 6 months, respectively) compared with the rosuvastatin group (118.8 and 122.9 mg/dl at 3 and 6 months, respectively), and the difference between groups was statistically significant (P=0.0104). It should be noted that more patients on atorvastatin were given an increase in their diabetic therapy to control their initial abrupt rise in glucose (64 vs. 45 subjects; HR 1.46, P=0.05). Adverse and serious adverse events were similarly observed in both groups (20.7% and 3.7% in the rosuvastatin group; 20.0% and 2.8% in the atorvastatin group), with 4.5% and 5.9% respectively deemed connected to the study drug. These results suggest that rosuvastatin might be preferable to atorvastatin because of its different influence on glucose levels.

Professor Hisao Ogawa (Kumamoto University, Kumamoto, Japan) presenting the different lipid-lowering actions and effects on glucose metabolism between rosuvastatin and atorvastatin in Japanese diabetic patients with hyperlipidemia (the LISTEN study) in a Hot Line session.
The ATLANTIC study included 1,862 patients with an ongoing STEMI of <6 h duration randomized to ambulance (n=909) or in-hospital treatment with ticagrelor or placebo in addition to aspirin and standard patient care.16 The ambulance loading dose was 180 mg ticagrelor before transfer, then a matching placebo in the cardiac catheterization laboratory. The other group received placebo in the ambulance, then a 180 mg ticagrelor loading dose in the catheterization laboratory. All patients subsequently received 90 mg ticagrelor twice daily for 30 days. The median time from randomization to angiography was 48 min and the median time difference between the 2 groups was 31 min. The results showed no difference between the randomized groups for the co-primary endpoints. First, in brief, the absence of ST segment elevation resolution of ≥70% after primary PCI was reported for 42.5% in the ambulance group and 47.5% in the in-hospital group. Second, the cumulative rate of major adverse cardiovascular events did not differ between the 2 groups. Conversely, the incidence of definite stent thrombosis was lower in the ambulance group than in the in-hospital group (0.0% vs. 0.8% in the first 24 h; 0.2% vs. 1.2% at 30 days). In both groups, the rates of major bleeding were generally low and identical. This study indicated that ambulance administration is safe and may even reduce the risk of stent thrombosis in acute phase.
PARADIGM-HFThe PARADIGM-HF trial kicked off the Hot Line sessions and was perhaps one of the most sensational topics in this congress.17 This study was a prospective comparison of LCZ696 (an experimental combination of the angiotensin-receptor blocker, valsartan, and neprilysin inhibitor) with the ACE inhibitor enalapril to determine the effect on global mortality and morbidity in patients with heart failure. A total of 8,442 patients with NYHA class II, III, or IV heart failure and left ventricular ejection fraction ≤40% were randomly assigned to either LCZ696 (200 mg twice daily) or ACE inhibitor (enalapril 10 mg twice daily) in addition to recommended therapy at 985 sites in 47 countries between December 2009 and January 2013. Although the primary endpoint was a composite of cardiovascular death or hospitalization for heart failure, the sample size was determined by the effect on cardiovascular mortality. This trial reached an early termination because LCZ696 significantly reduced the risk of cardiovascular mortality by 20% as compared with enalapril (HR 0.80, P<0.00004). In addition, the primary endpoint also appeared to favor LCZ696 compared with enalapril (HR 0.80, P<0.0000002). Secondary endpoints were also significantly improved by LCZ696, including all-cause mortality (17% vs. 19.8%; HR 0.84, P<0.001), as well as tolerability, as indicated by the Kansas City Cardiomyopathy Questionnaire. Professor Packer concluded that the PARADIGM-HF results represent a major improvement and reason for LCZ696 to replace ACE inhibitors or angiotensin-receptor blockers.
ODYSSEY StudiesAlirocumab is a fully-human monoclonal antibody and one of investigational lipid-lowering agents known as PCSK9 (protein convertase subtilisin/kexin type 9) inhibitors. In the ODYSSEY LONG TERM study, patients with heterozygous familial hypercholesterolemia or high cardiovascular risk on maximally tolerated statins and other lipid-lowering therapy were randomized to alirocumab 150 mg every 2 weeks (n=1,553) or placebo (n=788). Results at 24 weeks showed that LDL-cholesterol reduction was 61% for patients taking alirocumab in contrast to an increase of 0.8% for those given placebo (P<0.0001). Overall, 79% of patients taking alirocumab achieved LDL-cholesterol level <1.8 mmol/L (70 mg/dl) compared with 8% taking placebo. In comparison with patients taking placebo, a post-hoc analysis revealed that those given alirocumab achieved a 54% reduction in the relative risk of composite cardiovascular events (ie, coronary death, non-fatal MI, fatal and non-fatal ischemic stroke or unstable angina requiring hospitalization) (HR 0.46; 95% CI 0.26–0.82, P<0.01). In the same Hot Line session, the other ODYSSEY studies, namely ODYSSEY FHI/FHII and ODYSSEY COMBO II, were also presented.
NECTOR-HFExperimental augmentation of parasympathetic tone has recently emerged as a potential therapeutic approach to normalizing autonomic imbalance and inhibiting the progression of heart failure. This approach includes vagal nerve stimulation (VNS), which has been shown to achieve improved quality of life, exercise capacity and LV remodeling. The NECTOR-HF trial was the first randomized sham-controlled trial designed to evaluate the safety and efficacy of right-sided VNS.18 A total of 96 patients with heart failure from 24 centers in Europe underwent implantation of the VNS device in their neck near the right vagus nerve, and then connected to a pulse generator under the skin of the chest. After baseline testing of the system, patients were then randomized to either an active VNS group in which the mean stimulation amplitude was 1.24 mA at the initiation of the study and 1.42 mA at 3-month follow-up visit or a control group in which the device remained switched off. The primary endpoint of the study was the change in LV endsystolic diameter at 6 months. The secondary endpoints were other echocardiographic measurements, exercise capacity, quality-of-life assessments, 24 h Holter, and circulating biomarkers. At 6 months, no differences in the primary endpoint or the secondary echocardiographic endpoints, exercise capacity, and levels of NT-proBNP were observed. There were, however, statistically significant improvements in the quality-of-life measures in the treatment group. The safety profile showed an overall infection rate of 7.4%.
SOLID-TIMI 52Darapladib is a direct inhibitor of lipoprotein-associated phospholipase A2, which has been in development as a drug for the treatment of atherosclerosis. Previously the IBIS-2 trial showed that darapladib in stable coronary artery disease did not modify coronary atheroma volume but did appear to halt the progression of necrotic core assessed by IVUS-VH as compared with placebo on background statin therapy.19 Investigators were thus encouraged that darapladib might benefit ACS patients. The SOLID-TIMI 52 trial enrolled 13,026 patients who had been hospitalized for ACS within the past 30 days.20 Patients had at least 1 additional predictor of cardiovascular disease such as prior MI or polyvascular disease. Subjects were randomized to receive either 160 mg darapladib daily (n=6,504) or placebo (n=6,522). The primary endpoint was a composite of death from coronary artery disease, non-fatal MI, or urgent coronary revascularization for myocardial ischemia. After a median follow-up of 2.5 years, darapladib did not reduce the risk of the primary endpoint. In fact, after 3 years, the primary endpoint occurred in 16.3% of subjects in the darapladib group and 15.6% in the placebo group (HR 1.00, P=0.93). Similarly, darapladib failed to reduce the risk of the secondary endpoints (ie, cardiovascular death, MI, or stroke) (HR 0.99, P=0.78).
CvLPRITCurrent ESC and AHA/ACC guidelines recommend treating the infarct-related artery (IRA) only in MI patients. Nevertheless, it has been a big argument whether to treat angiographically significant stenoses in the non-IRA on admission for MI. The bottom line is that the findings from the PRAMI study showed a 65% reduction in MACE with complete revascularization (not only IRA but also non-IRA) at the time of primary PCI.21 Researchers have criticized the study design, the result of which is that PRAMI did not lead to widespread changes in clinical practice. In contrast to PRAMI, the complete versus lesion-only primary PCI trial (CvLPRIT) compared IRA-only treatment with complete revascularization during the index admission for MI. A total of 296 MI patients from 7 centers in UK were randomized before PCI to either IRA-only revascularization (n=146) or complete revascularization (n=150). For the complete revascularization group, the IRA was treated first followed by the non-IRAs. At 1 year following the index procedure, patients in the complete revascularization group had a more significantly reduced risk of MACE than those in the IRA-only revascularization group (10.0% vs. 21.1%; HR 0.45, P=0.009). Not surprisingly, procedure time and contrast volume load were significantly higher in the complete revascularization group than in the IRA-only group (55 vs. 41 min, P=0.0001; 250 vs. 190 ml, P<0.0001, respectively). Despite these findings, however, the patients with complete revascularization had no increased risk of stroke, major bleeding or contrast-induced nephropathy.
IBIS-4Although statins are known to reduce cardiovascular events, STEMI patients have not been included in intravascular ultrasound (IVUS) regression studies despite their high risk of recurrence and high frequency of vulnerable plaques extending beyond the culprit lesion. In the Integrated Biomarkers and Imaging Study (IBIS-4) study, 103 STEMI patients from 5 centers in Switzerland underwent IVUS investigations in the proximal part of the 2 non-IRAs immediately after primary PCI and received rosuvastatin 20 mg for 2 weeks, which was increased to 40 mg over 13 months.22 At 13 months follow-up, atheroma volume was reduced from 43.95 mm3 post-procedure to 43.02 mm3 (P=0.007), but there was no change in the volume of necrotic core (P=0.93). In order to detect statin-mediated alterations of the vessel wall, the investigators have already moved onto the subsequent study using optical coherence tomography (OCT) in the same population.
STAR AF 2Catheter ablation of the pulmonary veins can improve outcomes in around half of the patients with persistent atrial fibrillation (AF), and pulmonary vein isolation (PVI) is considered the cornerstone of catheter ablation in AF patients. In order to improve outcomes, current therapeutic guidelines suggest that more extensive ablation is required in addition to PVI. The STAR AF 2 study was the largest trial to assess the optimal ablation strategy for patients with persistent AF. Subjects were randomized to receive PVI alone, PVI plus ablation of complex fractionated electrograms, or PVI plus linear ablation in the left atrium. The results showed that successful PVI was achieved in 97% of all patients without any differences among the 3 groups, however, procedural time was significantly shorter for the PVI alone group (167 min) compared with the PVI plus electrograms and PVI plus linear ablation groups (229 and 223 min, respectively, P<0.001). The primary endpoint defined as freedom from documented AF episodes (>30 s) was not statistically different among the groups at 18 months follow-up. The authors concluded by saying that these results may force a change in the guidelines and a shift in practice to shorter and more effective PV ablation without any additional ablation for persistent AF patients.
The new guidelines on myocardial revascularization were jointly developed and published by the ESC and European Association for Cardio-Thoracic Surgery (EACTS). There are substantial changes from the previous version published in 2010 on the method of revascularization. This is mainly because of the longer-term outcome data generated by the SYNTAX trial and because more evidence is available for newer generation DES. Consequently, PCI is now regarded as equivalent to CABG in several lesion subsets that previously were recommended as preferably treated by surgery. The new guidelines also cover in great detail adjunctive pharmacotherapy and medical treatment after revascularization. This includes those clinically challenging cases in which dual antiplatelet therapy may be required in addition to oral anticoagulation (eg, AF). In patients with high bleeding risk, for instance, the guidelines make a class IIa-level C recommendation to limit triple therapy to 1 month, followed by a combination of oral anticoagulant plus either aspirin or clopidogrel after bare-metal stent or DES implantation.

Pocket clinical practice guidelines newly launched at the European Society of Cardiology (ESC) Congress 2014.
The new 2014 guidelines on cardiovascular assessment and management in non-cardiac surgery focus on patients in whom heart disease is a potential source of complications during surgery. The guidelines are generated by the ESC in collaboration with the European Society of Anesthesiology (ESA), involving several associations, councils, and working groups. The acceleration in population aging over the next 20 years will have a major effect on perioperative patient management. The total number of surgical procedures will thus increase even faster because of the rising frequency of interventions with age. The new guidelines offer a practical, stepwise evaluation of the patient that integrates clinical risk factors and test results with the estimated stress of the planned procedure. This means an individual cardiac risk assessment, with the opportunity to initiate medical therapy, coronary interventions, and specific surgical and anesthetic techniques to optimize the patient’s perioperative condition. Similar to the 2009 guidelines, emphasis is placed on the restricted use of prophylactic coronary revascularization, as this is rarely indicated simply to ensure that the patient survives surgery. The vast majority of patients with stable heart disease undergo low and intermediate-risk surgery without additional evaluation. Selected patients require an integrated multidisciplinary approach from anesthesiologists, cardiologists, and surgeons. The new guidelines present in algorithmic form an evidence-based, stepwise approach to determining which patients benefit from cardiac testing, coronary revascularization, and cardiovascular therapy before surgery.
Acute PEThere are 3 substantial changes in the clinical recommendations in the currently released guidelines. First, the case for risk stratification in the selection of a patient-centered treatment strategy is strengthened, and it is much clearer about who the intermediate-risk pulmonary embolism (PE) patients are. Secondly, the guideline committee evaluated outcome data from several recent trials and proved recommendations on the use of thrombolytics in normotensive PE patients. A third change reflects the great number of studies with new oral anticoagulants from the past few years. As a result, the guidelines include an expanded section on these drugs in both the acute and long-term setting. Furthermore, this guideline also includes for the first time recommended risk-adjusted therapeutic strategies on the basis of the aforementioned classification. Decisions for further treatment are based on balancing the risk of recurrence, determined by the etiology of PE (eg, transient risk factors, unprovoked or cancer-associated), against the risk of major hemorrhage from treatment. Experience with the new oral anticoagulants as acute, long-term, and extended therapy options is limited as yet, but as a class they appear to be safe and effective for all phases of treatment.
HCMThe guidelines on the diagnosis and management of hypertrophic cardiomyopathy (HCM) were presented for the first time at this congress. This guideline underscores the multidisciplinary approach to the disease, including imaging, genetics, percutaneous and surgical interventions, device implantation, and pharmacology. A new risk score to predict sudden cardiac death (SCD) as a continuous rather than dichotomous value is advocated. HCM Risk-SCD is based on maximal wall thickness, left atrial diameter, maximal LV outflow pressure gradient, family history of SCD, non-sustained ventricular tachycardia, unexplained syncope, and age. It is recommended that the 5-year risk of SCD should be assessed at first evaluation and re-evaluated at 1–2-yearly intervals or whenever there is a change in clinical manifestation. In addition, defibrillator implantation should be considered in patients with an estimated 5-year risk of SCD ≥6% and life expectancy >1 year.
Aortic DiseasesAortic diseases are within the scope of interest of not only cardiologists, but also radiologists, cardiac or vascular surgeons, and acute care professionals. This is the first European document to address comprehensively the acute and chronic diseases of the thoracic and abdominal aorta in adult patients. To emphasize the importance of differential diagnosis and decision-making for the treatment, this guideline includes several imaging techniques (eg, ultrasound, computed tomography, and magnetic resonance imaging) as well as prognosis in patients with acute aortic syndromes. The broad spectrum of aortic diseases, including congenital and inflammatory aortic diseases, and aortic tumors, is also addressed in the current document.
On the 31st August, the ESC and the JCS had a joint scientific session chaired by Professor Toyoaki Murohara (Nagoya University Graduate School of Medicine, Nagoya, Japan) and Dr Koen Nieman (Thoraxcenter, Erasmus Medical Center, Rotterdam, The Netherlands). This session focused on current computed tomography angiography (CTA) for ACS and the guidance of PCI. Dr Marc Dweck (Edinburgh, Scotland) introduced CT-PET fusion imaging to detect coronary artery diseases, followed by Dr Klaus Kofoed (Copenhagen, Denmark) presenting a novel subtraction technique to improve diagnostic ability specifically for calcified coronary arteries. Professor Yukio Ozaki (Fujita Health University Hospital, Toyoake, Japan) demonstrated his extensive research on CTA and vulnerable plaques.23,24 He also emphasized that OCT facilitates discrimination of ACS with ruptured fibrous cap (ACS-RFC) from ACS with intact fibrous cap (ACS-IFC) because of its high image resolution, and thus we should use the OCT-based clinical term “ACS-IFC” rather than the pathological term “OCT erosion”, as this can only be determined from pathological examinations (Figure 7).25,26 Finally, Dr Bjarne Norgaard (Aarhus, Denmark) shared his experience with Heart Flow FFRCT technology, and suggested the possibilities of global assessment of coronary artery diseases by a fully non-invasive approach.
ESC-JCS joint session entitled “Current Computed Tomography Angiography for the Mechanism of Acute Coronary Syndrome and the Guidance of PCI”. (A) Professor Yukio Ozaki (Fujita Health University Hospital, Toyoake, Japan). (B) Chairpersons and presenters of the ESC-JCS joint session. From left to right: Drs Klaus Kofoed, Marc Dweck, Yukio Ozaki, Koen Nieman (Chair), Bjarne Norgaard, and Toyoaki Murohara (Chair). ESC, European Society of Cardiology; JCS, Japanese Circulation Society.
The ESC Congress has grown rapidly to become the largest cardiology meeting in the world in terms of the number of attendees. The ESC Congress offers the latest clinical evidence and many scientific sessions are attractive not only for cardiologists or cardiovascular surgeons but also global healthcare professionals. Considering the substantial contribution of Japanese researchers, the JCS is becoming an important partner with the ESC.27 Thus the JCS and the ESC will organize 3 sessions, including a joint session and “Meet the ESC” session, in the upcoming 79th Annual Scientific Meeting of the JCS 2014 in Osaka.
Finally, we hope this report gives a brief summary of the latest knowledge, reminds attendees of the highlights of this congress, and also encourages young Japanese cardiologists to submit their abstracts to the next ESC Congress to be held from 29th August to 2nd September 2015 in London.
We thank Professor Toyoaki Murohara (Nagoya University Graduate School of Medicine, Nagoya, Japan) for the image used in Figure 5.
The authors (T.M. and Y.O.) are Fellows of the European Society of Cardiology (FESC). They report no conflicts of interest relevant to any content of this report.