Abstract
Background:
Despite the best efforts of pediatricians, healthcare for adult patients with congenital heart disease (ACHD) has proven challenging because of the increased numbers. This study presents the process of establishing an ACHD care system as a collaborative effort between Shinshu University Hospital and Nagano Children’s Hospital.
Methods and Results:
Establishing an outpatient clinic for transition, a cooperation agreement for in-patient care between the 2 hospitals, and quality management of diagnostic imaging and educational meetings for adult cardiologists were the 3 major challenges. Of the 99 patients who visited the transition clinic in the children’s hospital between May 2014 and December 2016, 3 returned to the pediatrician’s clinic. Between June 2013 and December 2017, 273 patients visited the ACHD center in Shinshu University Hospital. Until December 2017, mortality and fatal arrhythmia were noted in 3 and 2 cases, respectively. Catheter ablation for arrhythmia was performed in 12 cases, and 4 cases of pregnancy with moderate/severe ACHD or estimated as high risk were managed with healthy livebirths. Surgical interventions for moderate/severe ACHD were performed in collaboration with the children’s hospital or Sakakibara Heart Institute.
Conclusions:
Patients were successfully transferred to adult cardiology departments. Surgical and nonsurgical interventions for ACHD were provided. Collaboration between adult and pediatric cardiologists assists in the establishment of healthcare systems for ACHD.
Adult patients with congenital heart disease (ACHD) in Japan are facing an urgent issue regarding their healthcare. Because of an underdeveloped system, pediatric cardiologists currently care for these patients with regard to several aspects, including hypertension, diabetes mellitus, pregnancy, and mental health.1–6
Despite their best efforts, the number of patients with ACHD has already exceeded capacity.7
ACHD care is an established subspecialty in the USA and Europe.8,9
In addition to the patient care system, the specialist review boards also work well in those countries. Although Japanese adult cardiologists have started establishing ACHD care systems,10,11
deciding on the best system for ACHD care in Japan has proven difficult because of the lack of models. In fact, Shinshu University Hospital did not establish an ACHD care system until 2012 and the Nagano Children’s Hospital handled the care of such patients.
Since June 2013 we have operated the ACHD center in Shinshu University in collaboration with Nagano Children’s Hospital. Details of our experience with respect to the running of this center are expected to provide useful information for every adult cardiologist and cardiovascular institute that handles the care of patients with ACHD in daily practice. This report aimed to clarify the issues that were noted during the process of establishing the ACHD care system.
Methods
Nagano Model
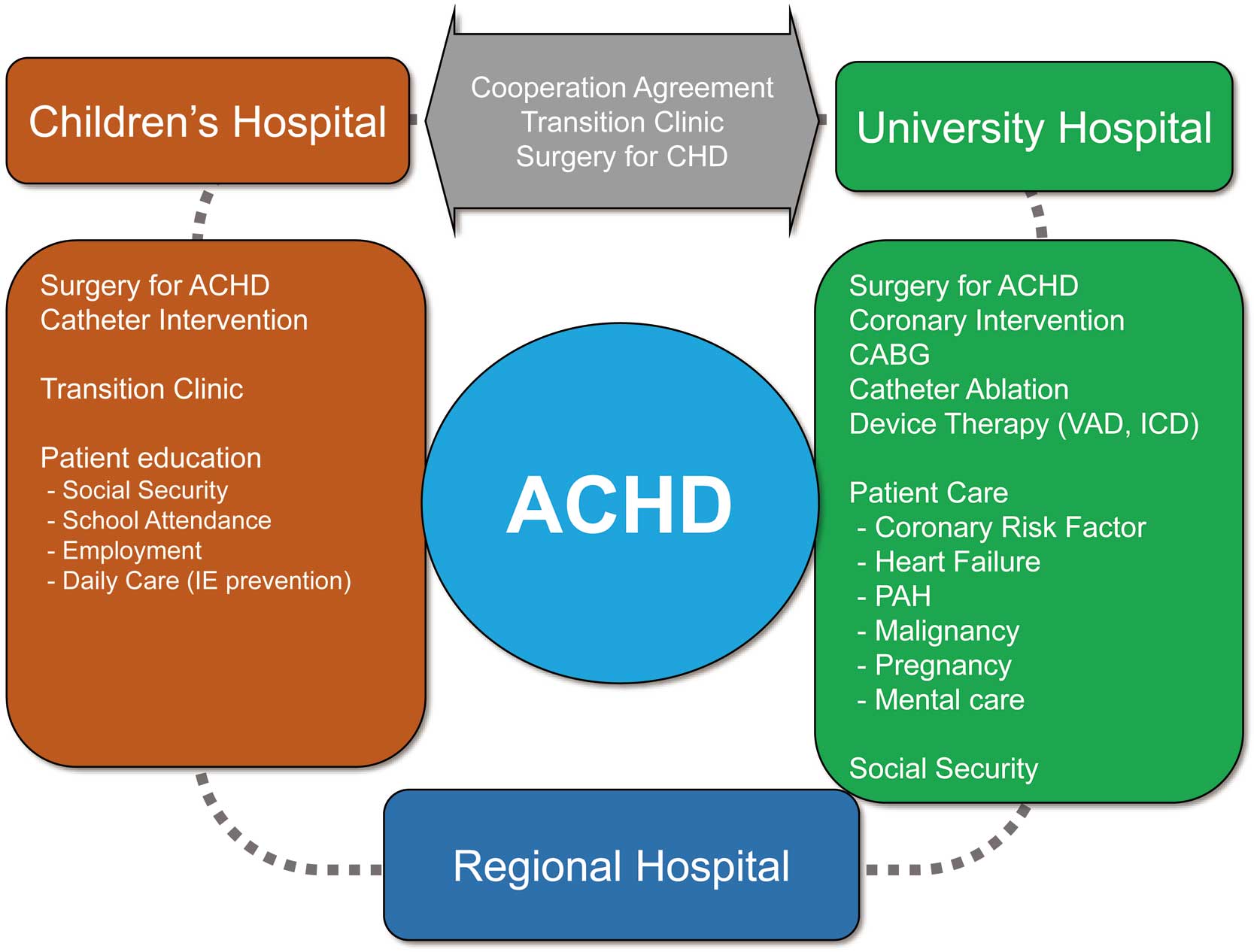
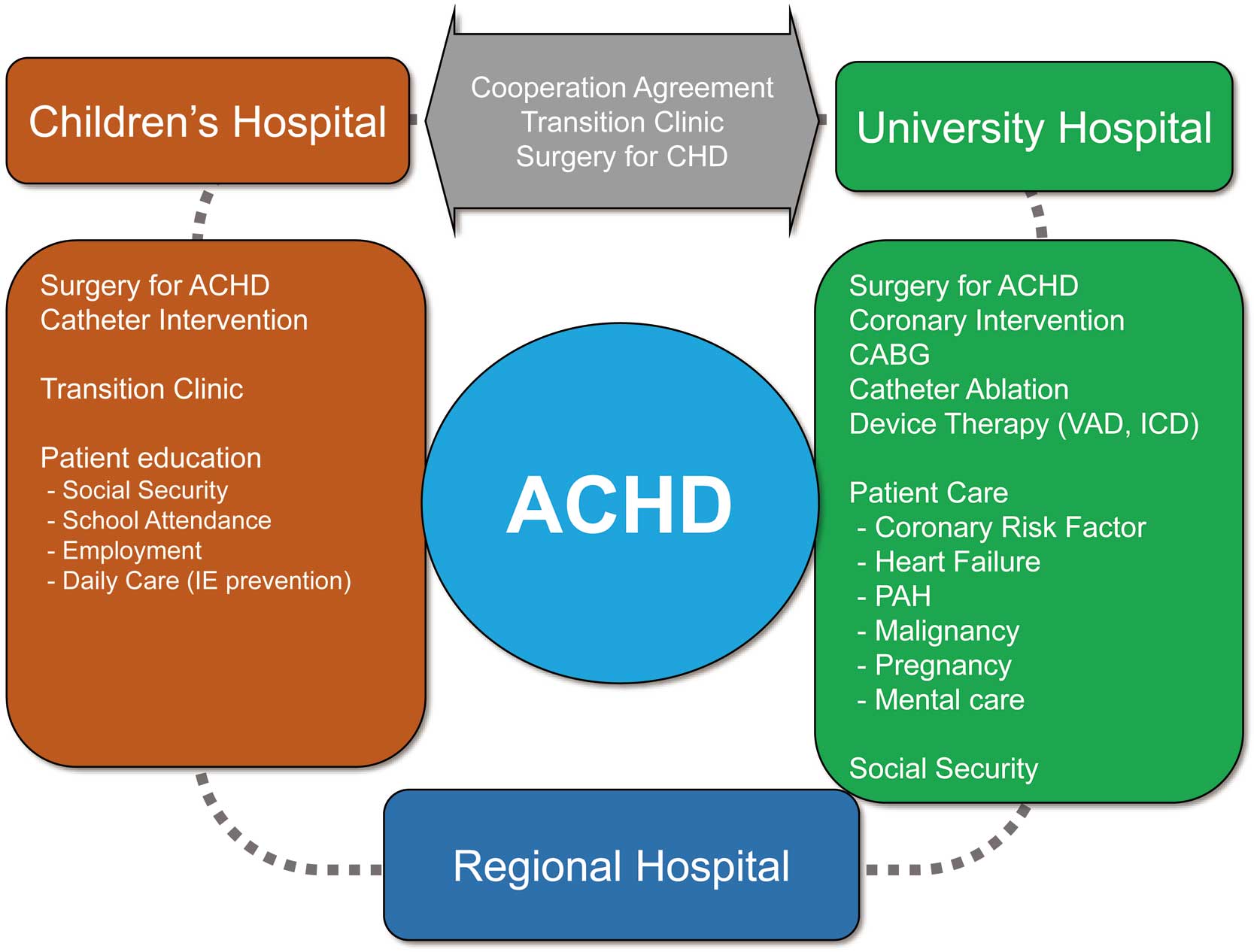
The Nagano model is a regional healthcare system for ACHD in our prefecture. As an ACHD core center, the Nagano Children’s Hospital and Shinshu University hospital provide cardiovascular interventions, including cardiovascular/noncardiovascular surgery and catheter interventions, and also management of pregnancy, and mental care (Figure 1). Regional hospitals and clinics in Nagano provide daily healthcare for ACHD. This model does not require the construction of novel instruments (hardware) for patient care, but rather for the physicians (software) in a university hospital and children’s hospital to collaborate. Shinshu University is located in Matsumoto city and Nagano Children’s Hospital in Azumino city. Thus, the Nagano model is an example of constructing a relationship between 2 distant institutes. The 3 major challenges in this model were: (1) outpatient clinic for transition, (2) cooperation agreement and in-patient care, and (3) quality management of diagnostic imaging and education for adult cardiologists. Patients’ clinical information, including demographics, diagnosis, surgical/nonsurgical interventions, and cardiovascular events, were screened and validated by chart review. Details of conferencing for diagnostic imaging and educational meetings were validated by the records of proceedings. This retrospective review was approved by the Shinshu University and Nagano Children’s Hospital Institutional Review Board.
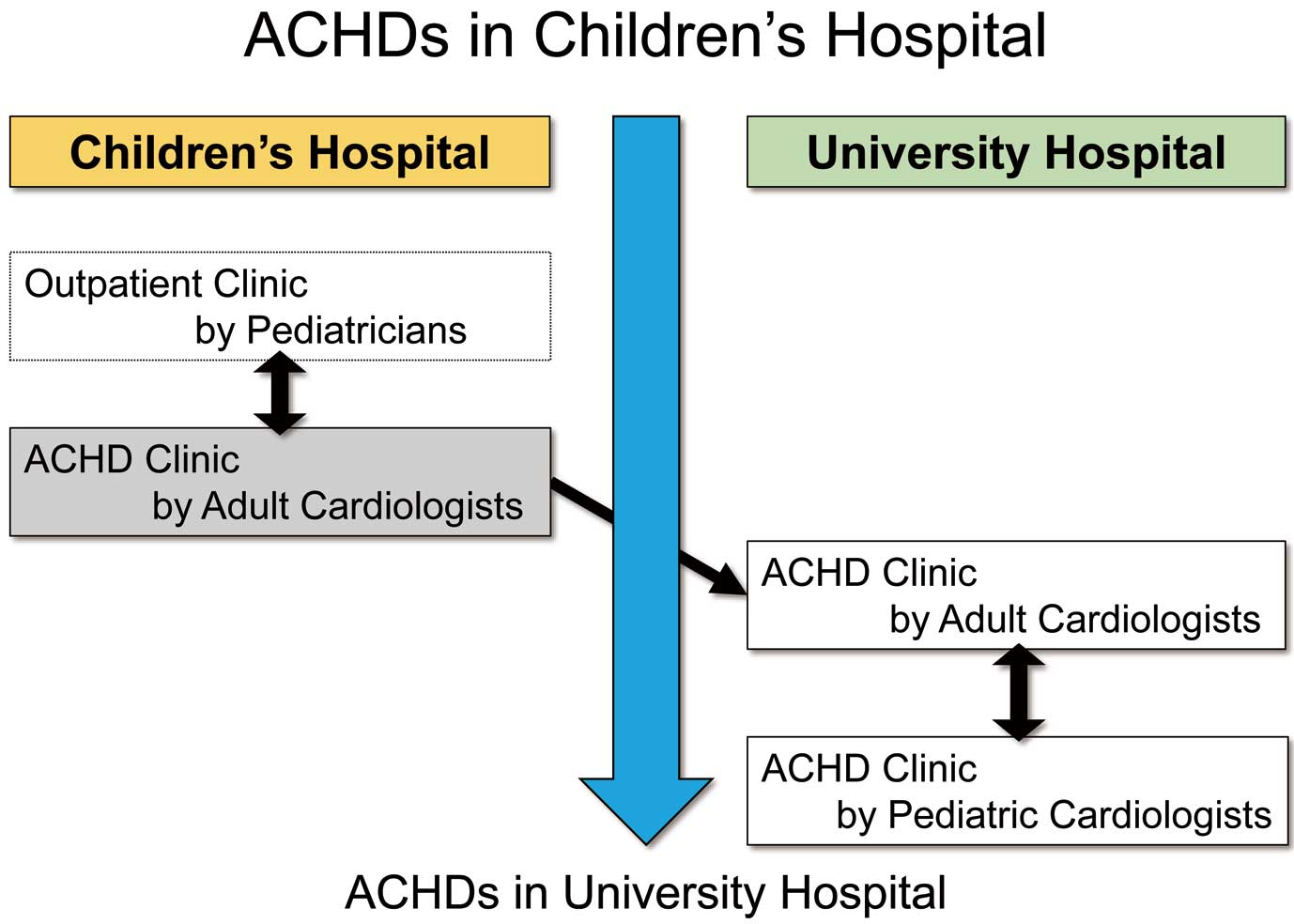
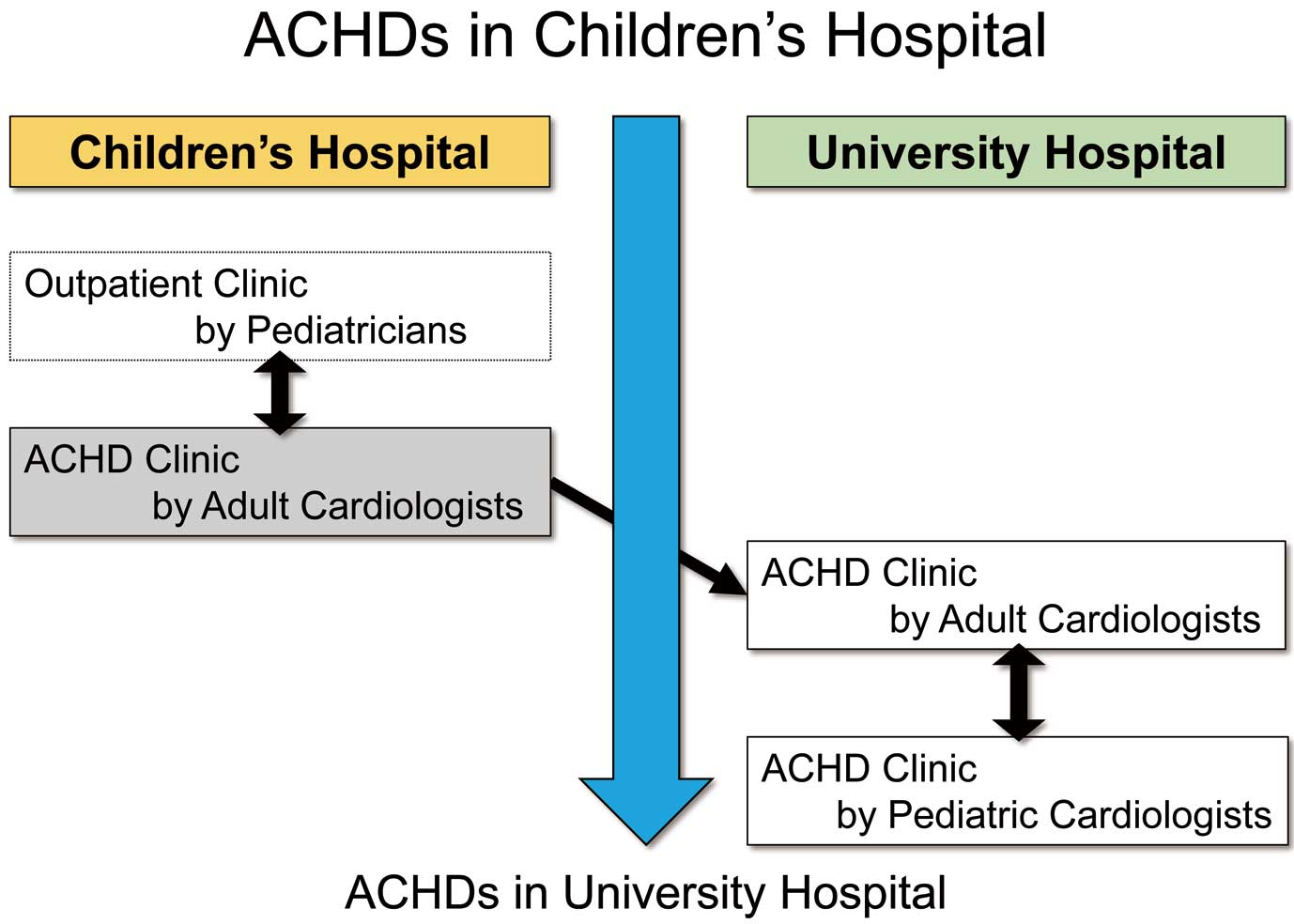
A transition clinic is operated by both adult and pediatric cardiologists in the children’s hospital (Figure 2). Patients aged >18 years are candidates for transition. Education of all patients from 6 years of age is started by pediatric cardiologists at the children’s hospital. Accomplishment of education is defined as follows: (1) be able to tell the name of the disease and surgery by 6th grade, (2) be able to write down the name of the disease and surgery by 9th grade, and (3) be able to draw their own heart anatomy and describe the considerations and issues of their own disease by 12th grade. In terms of transition, patients visit the clinic, which is operated alternately by adult and pediatric cardiologists. During this period, co-medical staff facilitate ACHD self-care. Next, the patients transfer to the university hospital on the 3rd visit to the adult cardiologist. Patients with valvular heart disease, prosthetic valves, cardiomyopathy, or arrhythmia, which adult cardiologists are familiar with managing, are directly transferred to the university hospital without a preparatory period, whereas patients with complex heart anatomy, including single-ventricular heart with or without Fontan palliation, are cared for by both adult and pediatric cardiologists at the children’s hospital for more than 1 year and are then transferred to the university hospital. Patients with mental retardation, such as 21 trisomy, might have a longer preparatory period in the children’s hospital. Electronic medical records are shared by the 2 hospitals over the Internet. Thus, adult cardiologists can refer to the past medical history, laboratory data, and imaging examinations recorded at the children’s hospital and vice versa.
To assess the accomplishment of the transfer, patients who visited the transition clinic between May 2014 and December 2016 at the children’s hospital were screened. Patients were transferred mainly to the university hospital. Patients who deviated from the transition protocol were deemed to have dropped-out. Patients who visited ACHD center in the university hospital were also screened. Age, sex, disease complexity, and sequelae were evaluated in line with the guidelines for ACHD.9
Cooperation Agreement and In-Hospital Care
A cooperation agreement for in-patient care was discussed between the 2 hospitals and concluded in June 2014. The aim of the agreement was to declare a relationship between the 2 hospitals for the establishment of an ACHD care system in Nagano. When patients are indicated for catheter intervention for CHD, such as atrial septal defect or patent ductus arteriosus, they can be admitted to the children’s hospital irrespective of age and sex. If patients are affected by coronary artery disease, arrhythmia, and/or heart failure during their stay in the children’s hospital, they would be transferred and treated in the university hospital so they are not occupying beds primarily for children’s care. In the case of surgery for CHD, surgeons and cardiologists in both hospitals would discuss the procedure and applicable institution for each case.
In this review, patients who visited the ACHD center in the university hospital were tracked. Major adverse cardiovascular events, including all-cause death, fatal arrhythmia, arrhythmic events treated by catheter ablation, and surgical interventions for moderate/severe ACHD, were screened. Pregnancy cases between June 2013 and December 2017 were also reviewed.
Quality Management of Diagnostic Imaging and Education
For the quality management of echocardiography, a sonographer learned the morphological and functional assessments of CHD in the children’s hospital. In terms of cardiovascular imaging examinations, including cardiac magnetic resonance imaging, cardiac computed tomography, catheter examinations, and echocardiography, the information browsing system was used to learn the sequence of examinations for precise assessment of cardiac anatomy and function in each case. Case conferences are held every 2 months in the university hospital. Strategies of medical management, indications for catheter intervention for ACHD, and indications for surgery are discussed in the conference. Imaging techniques of echocardiography and cardiac MRI are also discussed, and improvements raised by the pediatric cardiologists to the staff of the imaging technician and adult cardiologist.
Educational meetings are held every 6 months for adult cardiologists, fellows, and co-medical staff. Issues, including patient care systems, pregnancy management, arrhythmia, and mental health, are discussed. On the basis of these meetings, building up of the relationship among adult cardiologists for ACHD care is expected.
Results
Transition Clinic
A total of 105 patients visited the clinic between May 2014 and December 2016. The goals of the visit were transfer in 99 patients and others in 6 patients; 87 patients agreed to be transferred to the university hospital, 2 to other adult cardiovascular institutes, 7 were under preparation, and 3 went back to the pediatrician’s clinic.
Table 1
shows the details of the 3 patients who returned to the pediatrician’s clinic. Symptomatic status or moving away from Nagano prefecture was the major reason for returning to the pediatrician’s care. Of the 87 patients, only 1 had not yet visited the university hospital, 6 months after the planned date. That patient’s profile is also shown in
Table 1.
Table 1.
Profiles of the Patients Who Deviated From the Transition Protocol of the Nagano Model
| Age (years) |
Sex |
Diagnosis |
Details |
| Patients who returned to the pediatric clinic |
| 30 |
F |
DIRV, DORV, PS, MAPCAs, AT, p-APC Fontan |
TCPC conversion under discussion |
| 22 |
M |
Asplenia, AVSD, TGA, PS, TAPVC(III),
CA, Bil SVC, p-Fontan |
Moving away from Nagano |
| 29 |
M |
Criss-Cross Heart, DORV, p-APC Fontan,
p-TCPC+MAZE+CRT |
Moving away from Nagano |
| Patient who “dropped-out” of transition protocol |
| 24 |
M |
VSD (perimembranous) |
|
APC, aortopulmonary connection; AT, atrial tachycardia; AVSD, atrioventricular septal defect; Bil SVC, bilateral superior vena cava; CA, common atrium; CRT, cardiac resynchronization therapy; DIRV, double-inlet right ventricle; DORV, double-outlet right ventricle; MAPCAs, major aortopulmonary collateral artery; PS, pulmonic stenosis; TAPVC, total anomalous pulmonary venous connection; TCPC, total cavopulmonary connection; VSD, ventricular septal defect.
Figure 3
shows monthly cumulative number of patients referred to the ACHD center in the university hospital between June 2013 and December 2017. A total 273 patients visited the outpatient clinic. The mean age was 36±16 years, and 114 (42%) patients were male.
Figure 4
shows the complexity of the patients’ heart disease: 84 (31%) patients were moderate/severe ACHD; Fontan-type palliation was performed in 18 (atriopulmonary connection in 4, total cavopulmonary connection in 14) patients. One and one half repair in was performed in 2 patients. A history of protein-losing enteropathy and atrial tachycardia was noted in 2 and 7 patients, respectively.
Cooperation Agreement and In-Hospital Care
The Cooperation Agreement for ACHD was concluded between the hospitals in June 2014. The agreement allowed ACHD patients to be admitted to the children’s hospital irrespective of their age and sex and the collaboration was made widely known to the patients in Nagano. This agreement also stated that the ACHD care system would not solely be maintained by some motivated cardiologists but by 2 major public institutions in Nagano. Patients would be provided with a seamless medical service as a result of this agreement.
In terms of in-hospital care,
Table 2
shows the major adverse cardiovascular events. There were 3 cases of death, and fatal arrhythmia occurred in 2 cases. Catheter interventions for arrhythmia were performed in the university hospital: radiofrequency catheter ablation for atrial tachycardia in 8 cases (5 Fontan cases), atrial flutter in 2 cases, atrial fibrillation in 1 case (Fontan case), and paroxysmal supraventricular tachycardia in 1 case. A permanent pacemaker and subcutaneous implantable cardioverter defibrillator were implanted in 6 and 3 cases, respectively. Catheter interventions for structural heart disease (i.e., atrial septal defect and patent ductus arteriosus) were performed in the children’s hospital in 16 and 4 cases, respectively.
Table 3
lists the pregnancy cases in which there was moderate/severe ACHD or estimated high-risk status. All cases were successfully managed with healthy livebirths.
Table 4
shows the surgical interventions for moderate/severe ACHD. Of these, pulmonary valve replacement for tetralogy of Fallot and the David procedure were performed in the university hospital without major adverse cardiovascular events. Other surgeries for ACHD were performed in the children’s hospital or Sakakibara Heart Institute.
Table 2.
Profiles of Patients Who Had Major Adverse Cardiovascular Events
| MACE |
Age
(years) |
Sex |
Diagnosis |
| Sudden death |
36 |
M |
ToF, p-ICR, p-PVR, p-Bentall |
| HF death |
55 |
M |
ToF, p-ICR, p-TVR, p-reTVR, p-PVR |
| |
47 |
M |
SRV, CAF, NSVT, p-PAB |
| VF |
23 |
M |
ccTGA, VSD, Ebstein’s anomaly, TR, p-PAB, p-Senning/Jatene,
p-TVP, p-VSD closure |
| |
18 |
M |
ToF, PA, p-ICR |
CAF, chronic atrial fibrillation; ccTGA, congenitally corrected transposition grate arteries; HF, heart failure; ICR, intracardiac repair; MACE, major adverse cardiovascular event; NSVT, non-sustained ventricular tachycardia; PA, pulmonary atresia; PAB, pulmonary artery banding; PVR, pulmonary valve replacement; SRV, single right ventricle; ToF, tetralogy of Fallot; TR, tricuspid regurgitation; TVP/R, tricuspid valvoplasty/replacement; VF, ventricular fibrillation. Other abbreviations as in Table 1.
Table 3.
Profiles and Maternal Outcomes of Patients With High Maternal Cardiac Risk Factors
| Main diagnosis |
Age
(years) |
Sex |
Delivery |
Complications |
Fetal status |
| Bicuspid AV, AS |
36 |
F |
C/S |
None |
Healthy |
| ToF, p-ICR |
26 |
F |
|
None |
Healthy |
| MA, DORV, p-TCPC |
25 |
F |
C/S |
None |
Healthy |
| MR, p-MVR |
30 |
F |
C/S |
Hemorrhage |
Healthy |
AS, aortic stenosis; AV, aortic valve; MA, mitral atresia; MR, mitral regurgitation; MVR, mitral valve regurgitation. Other abbreviations as Tables 1,2.
Table 4.
Profiles of Patients Who Underwent Surgical Interventions
| Surgery |
Age
(years) |
Sex |
Diagnosis |
Institute |
| PVR |
54 |
F |
ToF, p-ICR, PR severe |
Shinshu Univ. Hosp. |
| PVR |
18 |
F |
ToF, p-ICR, PR severe |
Shinshu Univ. Hosp. |
| PVR |
47 |
M |
ToF, p-ICR, PR severe |
Sakakibara Heart Institute |
| Coronary angioplasty |
28 |
M |
TGA, p-Jatene, LMT stenosis |
Sakakibara Heart Institute |
| David procedure |
25 |
M |
ccTGA, p-DS, AAE, AR severe |
Shinshu Univ. Hosp. |
| TCPC conversion |
38 |
M |
Criss-Cross Heart, DORV, p-APC |
Nagano Children’s Hosp. |
AAE, annuloaortic ectasia; AR, aortic regurgitation; LMT, left main trunk; DS, double switch operation. Other abbreviations as Tables 1–3.
Multimodality imaging plays an essential role in the evaluation of the patients’ cardiac anatomy and function in CHD. Sonographers in the university hospital studied echocardiography for CHD at the children’s hospital for 6 months. Adult cardiologists can learn the protocols of echocardiography, cardiac magnetic resonance imaging, and angiography for CHD through the information browsing system between the 2 hospitals. By following the imaging techniques, patients were evaluated systematically under the same protocols in either hospital. In detail, imaging techniques of transesophageal echocardiography for discussion of the indication of transcutaneous closure in patients with atrial septal defect, the techniques of transthoracic echocardiography for evaluation of right ventricular function in patients with repaired tetralogy of Fallot and the affinities, and the methodology and results of cardiac MRI of patients who underwent Fontan-type palliation were major discussion points in the conferences.
Educational meetings held every 6 months for adult cardiologists, fellows, and co-medical staff discussed issues including patient care systems, pregnancy, arrhythmia, heart failure, and mental health. Lectures on ACHD management, including arrhythmia, pregnancy, and Fontan circulation, were given by several ACHD specialists. Adult cardiologists who are interested in ACHD are brought together in these meetings, thus fostering relationships among adult cardiologists.
Discussion
A patient healthcare system for ACHD was started in Nagano, with 3 initial challenges: (1) a transition clinic, (2) cooperation agreement and in-hospital care, and (3) multimodality imaging and education. These 3 issues were well covered in the relationship between the adult and pediatric cardiologists. The Nagano model did not require the construction of any new institutions for the patients’ care. Thus, there was no need to share expenses, but there was a need for adult and pediatric cardiologists to share time between the 2 hospitals.
Transitional Care for ACHD
The growing number of ACHD patients reflects the urgent issue of a healthcare system for ACHD in Japan. However, a shortage of physicians, especially in regional university hospitals, makes it difficult to develop ACHD specialists.5
In the Nagano model, adult cardiologists could learn about the management of ACHD by visiting the children’s hospital and taking care of them alongside pediatric cardiologists in the transition clinic. A previous report suggested that a nurse-led transition intervention improved self-management,12
total knowledge level, and better understanding of deterioration symptoms.13,14
Our model provided an additional approach by adult cardiologists: a transition clinic in the children’s hospital.
Reid et al reported in 2004 that only 48% of adolescents with CHD underwent successful transition to adult care.15
Moons et al reported suboptimal provision of care in Europe for ACHD,16,17
warranting preparation for the transfer.18
As a result, a person-centered transition program was provided19
in 2017. Thus, physicians and co-medical staff could follow this program for better transition in Japan as well. Indeed, Goossens et al reported in 2011 that a substantially lower proportion of lost-to-follow-up was achieved by such patient-centered care.20
A multidisciplinary approach might enable achievement of successful transition to an adult cardiologist in the Nagano model. From the viewpoint of successful transition, introducing adult cardiologists in the children’s hospital would ease the experience of stepping into this new area of ACHD. Adult cardiologists can take time to learn each patient’s profile and to build up the relationship among physicians, patients, and their relatives in the transition clinic. Visits to the children’s hospital by adult cardiologists enabled patients to easily access the transition protocol and this protocol should minimize the number of patients “lost to follow-up” from outpatient care.
Various factors should be considered for successful transfer/transition. A doctor-patient relationship is needed. Attachment to the pediatric setting and pediatric providers and lack of confidence in the care given to the patient by an unknown provider are 2 major issues affecting adolescent transition. The more complex the heart anatomy or the more severe the mental retardation, the longer and more careful the observation period needed at the children’s hospital. Essentially, in our model the timing of complete transfer was the 3rd visit by an adult cardiologist; however, it depends on each patient’s condition. In the transition clinic the cardiologist would ask the patient whether they hoped to be transferred to the university hospital. When they accepted the transfer, that was the right time. If they asked to stay at the children’s hospital, they could stay there. For patients with mental retardation or those who needed help to make decisions, a parent may achieve as their deputy.
Parents could affect the success of the transitional care. They could: (1) act as the patient’s deputy, (2) support the patient by accompanying them, (3) wait for the patient in the hospital’s lobby, or (4) entrust them completely. These behaviors might depend on the degree of autonomy of their children. In types (2)–(4), parents supported their children’s self-reliance in various ways that did not annoy care givers. Unstable disease condition, mental retardation, or high dependence on their parents might lead to less autonomy and type 1 parental behavior. Transfer should be delayed if the patients’ condition is unstable. Repeated educational interventions for the patient might be also needed in cases of a low degree of autonomy. In patients with mental retardation, parents are essential in disease management. Physicians would be able to assess the patients’ medical and social condition from the parents’ behavior. In type 1, attention should be paid to not moving quickly to the university hospital.
Collaboration Between Institutions for ACHD Care
Collaboration not only with a children’s hospital but also with a high-volume center is necessary for the management of ACHD. Diagnostic evaluation and medical management would proceeded by adult cardiologists in collaboration with pediatric cardiologists. However, perioperative care for ACHD should be carried out in an adult cardiovascular institute, because it might need a longer hospital stay than in pediatric cases, and ACHD patients should not occupy beds required for children. Furthermore, surgery for moderate/severe CHD should be performed in experienced hospitals or in collaboration with experienced ACHD surgeons and surgeons for adult heart disease. Thus, Shinshu University collaborated with surgeons at both the children’s hospital and the Sakakibara Heart Institute, which is known as a high-volume center for ACHD care.
Education for ACHD Care
A patient education program is essential to facilitate transition.16–20
Some patients tend to rely on their parents or pediatricians with respect to the determination of medical care planning. Understanding their own heart anatomy, operations, and sequelae would increase treatment adherence and make the transfer easier as a result. Supporting the independence of young adult patients is necessary to operate a transition protocol not only in the field ACHD but also in other areas of pediatrics.
In terms of education for medical staff, electronic medical records are convenient for sharing patients’ information. Moreover, adult cardiologists can learn and follow the imaging techniques and sequences to evaluate the cardiac anatomy and function of CHD. However, the number of patients will not decrease from now on. In the university hospital, 1 adult cardiologist conducts ACHD care and manages the patients in the outpatient clinic. Other physicians (n=20) take care of ACHD patients who are admitted to the university hospital. Cardiologists who are interested in heart failure, cardiovascular imaging, or arrhythmia as a subspecialty are the candidates who commit to ACHD care. The importance, necessity, and worthiness of ACHD care should be promoted more. Certificate board and additional rewards for ACHD medical care would facilitate the accomplishment of an ACHD care system in Japan. Specialized nurses for ACHD care are not available in our hospitals. They would be helpful for both the patients and physicians. Participation of adult cardiologists and establishment of a regional medical network for ACHD would also be extremely helpful. In this regard, politicians and organizations should facilitate the accomplishment of an ACHD care system in Japan by additional rewards for transitional care.
Study Limitations
First, the Nagano model was based on collaboration by 2 distant institutes. Some children’s hospitals or children’s medical centers that are distant from medical centers for adults could be candidates for a similar Nagano model. However, in-hospital or neighborhood collaboration might be easier to build up between adult and pediatric departments, especially in urban areas. Various models of in-hospital, hospital-hospital, and hospital-clinic collaborations for ACHD care should be introduced. Second, our cohort was relatively small, and a short follow-up period was obvious. Indeed, redo-Rastelli procedure has not been indicated so far. Although it is known that referral to specialized ACHD care is associated with a significant reduction in mortality, we did not have enough numbers of cardiovascular events to discuss the association between specialized ACHD care and mortality reduction. Finally, our transition protocol was unable to completely prevent “lost to follow-up”. Thus, periodic confirmation of transfer achievement is mandatory. Nevertheless, our experience provides useful information for potential candidates of the counterpart of a pediatric cardiovascular institute to build up a healthcare system for ACHD.
Conclusions
The ACHD care system has been launched in Nagano. Partnership between adult cardiologists in a university hospital and pediatric cardiologists in a children’s hospital would be a helpful collaboration to establish a system for ACHD, but political support is mandatory to facilitate the establishment of a nationwide ACHD care system.
Sources of Funding
Establishment of ACHD care system project was supported by the Shinshu University “chi-no-mori” foundation and the Model project to support transitional care for adult patients with childhood-onset chronic disease.
References
- 1.
Negishi J, Ohuchi H, Miyazaki A, Tsuda E, Shiraishi I, Kurosaki K. Clinical characteristics of adult patients with congenital heart disease hospitalized for acute heart failure. Circ J 2018; 82: 840–846.
- 2.
Miyazaki A, Sakaguchi H, Matsumura Y, Hayama Y, Noritake K, Negishi J, et al. Mid-term follow-up of school-aged children with borderline long QT interval. Circ J 2017; 81: 726–732.
- 3.
Kuwabara M, Niwa K, Toyoda T, Shirai T, Tateno S, Ohuchi H, et al. Liver cirrhosis and/or hepatocellular carcinoma occurring late after the Fontan procedure: A nation wide survey in Japan. Circ J 2018; 82: 1155–1160.
- 4.
Ochiai R, Kato H, Akiyama N, Ichida F, Yao A, Inuzuka R, et al. Nationwide survey of the transfer of adults with congenital heart disease from pediatric cardiology departments to adult congenital heart disease centers in Japan. Circ J 2016; 80: 1242–1250.
- 5.
Ochiai R, Murakami A, Toyoda T, Kazuma K, Niwa K. Opinions of physicians regarding problems and tasks involved in the medical care system for patients with adult congenital heart disease in Japan. Congenit Heart Dis 2011; 6: 359–365.
- 6.
Ochiai R, Yao A, Kinugawa K, Nagai R, Shiraishi I, Niwa K. Status and future needs of regional adult congenital heart disease centers in Japan. Circ J 2011; 75: 2220–2227.
- 7.
Toyoda T, Tateno S, Kawasoe Y, Shirai T, Shiina Y, Matsuo K, et al. Nationwide survey of care facilities for adults with congenital heart disease in Japan. Circ J 2009; 73: 1147–1150.
- 8.
Baumgartner H, Bonhoeffer P, De Groot NM, de Haan F, Deanfield JE, Galie N, et al; Task Force on the Management of Grown-up Congenital Heart Disease of the European Society of Cardiology (ESC); Association for European Paediatric Cardiology (AEPC); ESC Committee for Practice Guidelines (CPG). ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 2010; 31: 2915–2957.
- 9.
Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2008; 52: e143–e263.
- 10.
Ishizaki U, Nagao M, Shiina Y, Fukushima K, Takahashi T, Shinomiya Y, et al. Prediction of Fontan-associated liver disease using a novel cine magnetic resonance imaging “Vortex Flow Map” in the right atrium. Circ J 2018; 82: 2143–2151.
- 11.
Marume K, Fukui S, Shimamoto K, Ohuchi H, Tsuji A, Ogo T, et al. Coexistence of a double-chambered right ventricle with Ebstein-like anomaly and right ventricular apical hypoplasia. Circ J 2018; 82: 1215–1217.
- 12.
Mackie AS, Islam S, Magill-Evans J, Rankin KN, Robert C, Schuh M, et al. Healthcare transition for youth with heart disease: A clinical trial. Heart 2014; 100: 1113–1118.
- 13.
Goossens E, Fieuws S, Van Deyk K, Luyckx K, Gewillig M, Budts W, et al. Effectiveness of structured education on knowledge and health behaviors in patients with congenital heart disease. J Pediatr 2015; 166: 1370–1376.
- 14.
Janssens A, Goossens E, Luyckx K, Budts W, Gewillig M, Moons P; i-DETACH investigators. Exploring the relationship between disease-related knowledge and health risk behaviors in young people with congenital heart disease. Eur J Cardiovasc Nurs 2016; 15: 231–40.
- 15.
Reid GH, Irvine MJ, McCrindle BW, Sananes R, Ritvo PG, Siu SC, et al. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics 2004; 113: e197–e205.
- 16.
Moons P, Engelfriet P, Kaemmerer H, Meijboom FJ, Oechslin E, Mulder BJ; Expert Committee of Euro Heart Survey on Adult Congenital Heart Disease. Delivery of care for adult patients with congenital heart disease in Europe: Results from the Euro Heart Survey. Eur Heart J 2006; 27: 1324–1330.
- 17.
Moons P, Scholte op Reimer W, De Geest S, Fridlund B, Heikkila J, Jaarsma T, et al. Nurse specialists in adult congenital heart disease: The current status in Europe. Eur J Cardiovasc Nurs 2006; 5: 60–67.
- 18.
Moons P, Pinxten S, Dedroog D, Van Deyk K, Gweillig M, Hilderson D, et al. Expectations and experiences of adolescents with congenital heart disease on being transferred from pediatric cardiology to an adult congenital heart disease program. J Adolesc Health 2009; 44: 316–322.
- 19.
Acuna Mora M, Sparud-Lundin C, Bratt EL, Moons P. Person-centred transition programme to empower adolescents with congenital heart disease in the transition to adulthood: A study protocol randomized controlled trial (STEPSTONES project). BMJ Open 2017; 7: e014593.
- 20.
Goossens E, Stephani I, Hilderson D, Gewillig M, Budts W, Van Deyk K, et al. Transfer of adolescents with congenital heart disease from pediatric cardiology to adult health care: And analysis of transfer destinations. J Am Coll Cardiol 2011; 57: 2368–2374.