論文ID: CJ-19-0220
論文ID: CJ-19-0220
Heart failure (HF) is a progressive disease (Figure).1 Physical function represented by New York Heart Association functional class gradually decreases with repeated exacerbation of HF, and patients with HF become refractory to treatment, eventually leading to death. Various treatments, including disease management, drug therapy, and non-drug therapy, are available for each stage of HF, and thus it is crucial to select an optimal treatment at the appropriate time. Clarifying the surrogate markers of high-risk patients is also an important goal. Although it is known that a history of HF hospitalization is a high risk factor,2 there have been no studies focusing on the clinical significance of the number of hospitalizations in patients with a history of HF hospitalization.
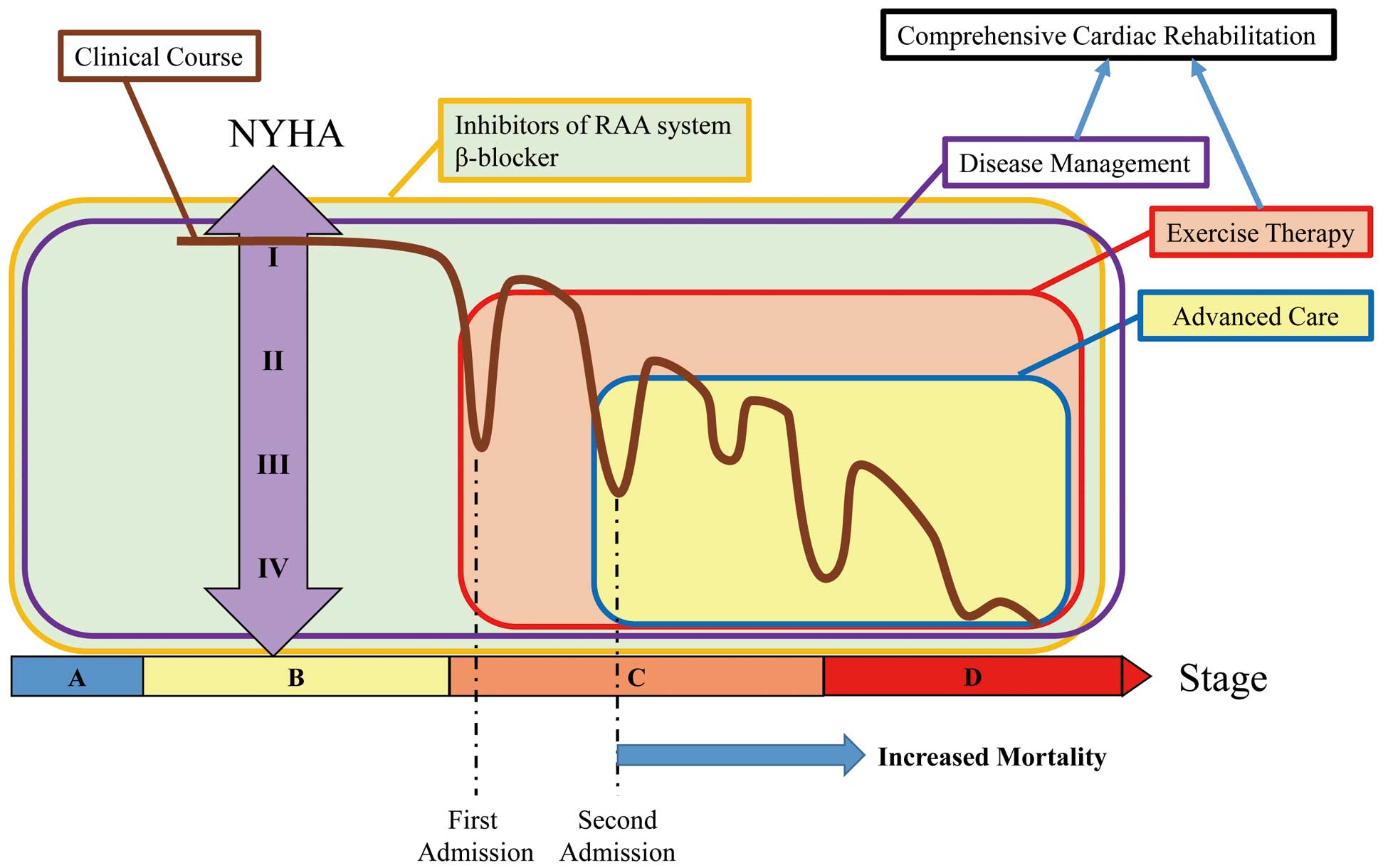
Clinical course of patients with heart failure and optimal treatment at each stage. Early introduction of appropriate and maximum drug therapy and comprehensive cardiac rehabilitation (disease management, exercise therapy) is needed to prevent repeated hospitalization. High-risk patients who have had multiple admissions should be considered candidates for advanced care. NYHA, New York Heart Association; RAA, renin-angiotensin-aldosterone. (Based on Goodlin SJ with permission.1)
Article p ????
In this issue of the Journal, Akita et al investigate the prognostic impact of previous hospitalization by analyzing data from the prospective and multicenter WET-HF registry of patients hospitalized for acute HF.3 They divided 1,580 patients into 3 groups based on the number of previous HF admissions: no previous admission, single previous admission, and multiple previous admissions. HF patients with multiple previous admissions had lower blood pressure, lower hemoglobin level, and poorer kidney and cardiac function than the other groups. Multiple previous admissions was an independent risk factor for all-cause death and HF readmission compared with the other 2 groups. This result was similar in all subgroup analyses and could be widely applied to every HF population. On the other hand, a single previous admission was an independent risk factor for HF readmission, but not all-cause death, compared with no previous admission. The most important point of the study is that the authors focused on the significance of the number of previous admissions rather than the mere presence of previous admission. They argue that this extremely simple factor can identify high-risk HF patients and determine the timing of the introduction of advanced care (Figure). In this way, the proposal of the surrogate marker in this study is highly significant.
It is important to prevent readmission for exacerbation of HF. In cases of HF with reduced or preserved ejection fraction, inhibitors of the renin-angiotensin-aldosterone system and β-blockers are effective for suppressing readmission for HF exacerbation. Data on admission of patients with a single previous admission in this study showed that the prescription rate of angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers was 52%, and that of β-blockers was 50%. Even patients with multiple previous admissions were in the 60% range for both classes of agents. The finding that a history of multiple previous admissions confers a high risk suggests the importance of the early introduction of basic drug therapy for HF (Figure). In a study investigating precipitating factors for readmission because of HF worsening, the influence of patient-related factors (non-adherence with diet, drugs, or restriction of activity, and physical and emotional stress) was greater than the influence of medical factors.4 Therefore, comprehensive patient education and counseling are necessary. In fact, home-based intervention and general patient management have been reported to be effective for preventing readmission of HF patients.5,6 Appropriately prescribed exercise therapy is effective not only for the prognosis of patients with HF but also for preventing readmission.7 General patient management and exercise therapy are themselves comprehensive cardiac rehabilitation programs, and their early introduction for HF patients is essential (Figure).
The unresolved question is how a history of multiple admissions becomes a surrogate marker of HF. That is, what does admission because of exacerbation of HF adversely affect? Excessive heart load from hemodynamic instability or myocardial injury secondary to treatment for HF may cause deterioration of cardiac function.8 Readmission may cause exacerbation of renal dysfunction because of congestion and anemia.9 Each of these conditions is known to be prognostic factors for HF.10,11 Indeed, cardiac and kidney function and hemoglobin levels were lower in patients with multiple admissions in this study. However, it is not clear whether an increased number of hospitalizations exacerbates these organ failures, or whether the number of admissions is simply higher in patients who have poor organ function to begin with. Conversely, it has been suggested that repeated admissions for HF exacerbation progressively decrease physical function. Bed rest is required in the acute phase of exacerbation of HF, but prolonged bed rest decreases skeletal muscle strength and mass. Recently, attention has been focused on sarcopenia and frailty, and these complications are more frequent in HF patients than in healthy elderly people. Moreover, long-term bed rest exacerbates sarcopenia and frailty, which further reduces physical function. In Japan, the length of hospital stay for patients admitted for exacerbation of HF is markedly longer than in other countries. Moreover, it has been reported that the longer the number of days to ambulation is, the worse the prognosis after discharge will be.12 By elucidating the target of multiple admissions, it will become clear which intervention method is most appropriate.
Another problem is whether the prognosis is affected by the interval between successive admissions. Pocock et al reported that previous admission for HF within 6 months, but not beyond 6 months, was an independent predictor of all-cause death in chronic HF.13 Whether there is a difference in the interval until rehospitalization in the case of multiple admissions is unknown. Also, is there a difference in prognosis not only according to the number of admissions but also in terms of the length of stay? Analysis taking this point into consideration is also necessary.
In conclusion, the number of admissions is a simple surrogate marker of prognosis for HF and readmission. Early introduction of a comprehensive set of interventions to prevent readmission because of HF is crucial.
The authors declare no conflicts of interest.