論文ID: CJ-21-1008
論文ID: CJ-21-1008
Cardiovascular (CV) disease is the leading cause of morbidity and mortality worldwide.1 Lipid-lowering therapy has been established as the mainstay for primary and secondary prevention of CV disease,2–4 and current guidelines also recommend managing residual CV risk factors, such as smoking, hypertension, diabetes mellitus, and obesity.5 Additionally, the relationship between periodontal disease and risk of CV events has been studied, but there is still not enough evidence.
Article p ????
Periodontal disease may cause transient bacteremia, endothelial dysfunction, and systemic inflammation.6 Chronic inflammation is known to accelerate atherosclerosis and increase the risk of CV events.7 In this issue of the Journal, Fukushima et al8 report that periodontal disease at baseline was associated with an increased risk of major adverse cardiac events (MACEs) in patients with coronary artery disease. In their report, MACEs were defined as a composite of cardiovascular death, non-fatal myocardial infarction, target lesion revascularization (TLR), or non-TLR. Interestingly, among the MACEs, a higher rate was found in the periodontal disease group, primarily due to cardiac deaths and non-TLR, as opposed to TLR, even though baseline and follow-up statin and low-density lipoprotein cholesterol (LDL-c) levels did not differ between the group diagnosed with periodontal disease and the group without. According to previous reports, chronic inflammation may increase the risk of plaque rupture, leading to acute coronary syndrome.7,9,10 These inflammatory mechanisms may help explain the increased occurrence of MACEs in the periodontal disease group (Figure).
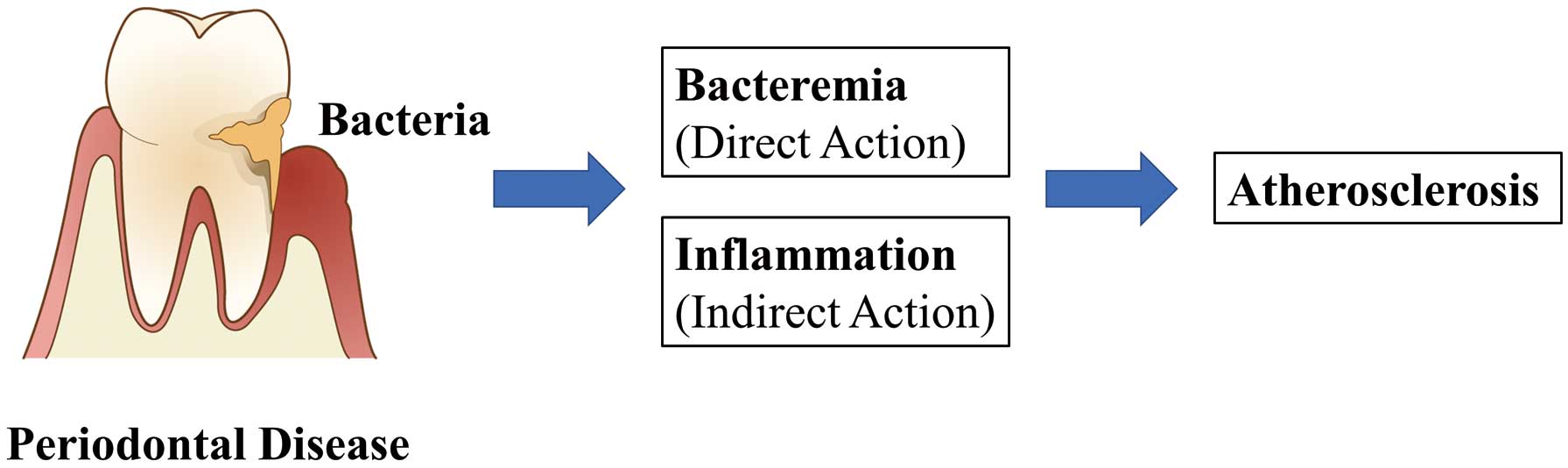
Potential mechanisms of periodontal disease and atherosclerotic cardiovascular disease.
These findings carry implications for treating periodontal disease and preventing future CV events. Increased frequency of tooth brushing has been found to reduce serum concentrations of C-reactive protein and fibrinogen, suggesting that the improvement of periodontal conditions could reduce a patient’s systemic inflammatory status.11–13 Previous observational research suggested that improved oral hygiene care, such as frequent tooth brushing and regular dental visits, may modify adverse atherosclerotic cardiovascular outcomes associated with poor oral health.13 Recently, other reports based on observational studies have suggested that oral hygiene care is associated with a decreased risk of new-onset diabetes, atrial fibrillation, and heart failure.14,15 The involvement of inflammation has also been proposed for these mechanisms. Those reports propose that inflammation promotes arteriosclerotic change, valve injury, and myocardial damage, resulting in heart failure.
Improved oral care and other CV conditions could possibly share a relationship. However, the data are observational. Better oral hygiene might correlate with better control of other cardiovascular risk factors, such as dyslipidemia, hypertension, and diabetes mellitus. Potential interactions need to be considered, warranting further studies to elucidate the mechanism underlying the relationship between periodontal disease and future CV risk.
K.T. is a member of Circulation Journal’s Editorial Team.