論文ID: CJ-22-0040
論文ID: CJ-22-0040
Background: The coronavirus disease (COVID-19) pandemic may have influenced the prehospital emergency care and deaths of individuals experiencing an out-of-hospital cardiac arrest (OHCA).
Methods and Results: We analyzed the registry data of 2,420 and 2,371 OHCA patients in Osaka City, Japan in 2019 and 2020, respectively, according to the 3 waves of the COVID-19 pandemic. Patient outcomes were compared using multivariable logistic regression analyses with the 2019 data as the reference. Bystander cardiopulmonary resuscitation (CPR) was initiated significantly less frequently in 2020 than in 2019 (2019: 48.0%, 2020: 42.7%, P<0.001), particularly during the first wave (2019: 47.2%, 2020: 42.9%, P=0.046) and second wave (2019: 48.1%, 2020: 41.2%, P=0.010), but not during the third wave (2019: 49.2%, 2020: 44.1%, P=0.066). The public-access automated external defibrillator was less frequently applied during the first wave (2019: 12.6%, 2020: 9.9%, P=0.043), with no significant difference during the second wave (2019: 12.5%, 2020: 12.8%, P=0.863) and third wave (2019: 13.7%, 2020: 13.0%, P=0.722). There was a significant difference in 1-month survival with favorable neurological outcomes (2019: 4.6%, 2020: 3.3%, P=0.018), with a 28% reduction in the adjusted odds ratio in 2020 (0.72; 95% confidence interval: 0.52–0.99, P=0.044).
Conclusions: Bystander CPR and neurologically favorable outcomes after OHCA decreased significantly during the COVID-19 pandemic in Japan.
Out-of-hospital cardiac arrest (OHCA) is one of the major causes of death worldwide, and more than 75,000 cases occur annually in Japan.1 In late 2019, the spread of a new coronavirus disease (COVID-19) became a global public health issue: the number of people infected with COVID-19 is >230 million worldwide2 and was 1,712,649 in Japan as of October 15, 2021.3 In Japan, the COVID-19 pandemic affected prehospital emergency medical service (EMS) systems, as in other countries.4–6
Undoubtedly, early bystander cardiopulmonary resuscitation (CPR) and defibrillation with a public-access automated external defibrillator (AED) provide OHCA patients with the highest likelihood of survival. However, reports from areas severely affected with COVID-19 have indicated a decrease in bystander CPR (from 45.3% to 34.6% in Lombardy, Italy, and from 63.9% to 47.8% in Paris, France) and survival at hospital discharge (from 9.5% to 5.1% in Lombardy and 5.4% to 3.1% in Paris) compared with the pre-pandemic period.4,5
The degree and timing of the COVID-19 epidemic, behavioral restrictions such as lockdowns, and the implementation of preventive measures have varied around the world. Our previous report, which analyzed the first wave of the COVID-19 pandemic in Osaka City, demonstrated that bystander CPR and public-access AED applications were less frequent; however, patient outcomes remained unchanged.7
In Japan, there have been 5 COVID-19 pandemic waves since the first domestic COVID-19 case was confirmed on January 16, 2020, and each wave has been larger than the one before. Therefore, it is possible that patient outcomes have been affected, as in other countries where the number of COVID-19 patients is high. In this study, we compared bystander interventions, EMS activities, and patient outcomes in Osaka City, Japan, between 2019 and 2020.
This population-based cohort study included all OHCA patients treated by EMS personnel in Osaka City, Japan according to the revised Utstein-style guidelines.8 Osaka City is the largest city in Osaka Prefecture, with a population of approximately 2.7 million in a 225.3-km2 area.9 Details of the data collection have been previously published.10,11
During the current study period, 14,143 cases of COVID-19 were documented in Osaka City.12,13 Based on the increase or decrease in the number of COVID-19 patients, Osaka Prefecture defined January 29, 2020 to June 13, 2020 as the first wave, when a state of emergency for Osaka was declared; June 14, 2020 to October 9, 2020 as the second wave; and October 10, 2020 to February 28, 2021 as the third wave.14,15 The Japanese government did not impose a lockdown, as occurred in other countries.
We evaluated OHCA outcomes and resuscitation processes based on the international standardized Utstein-style guideline.8 Therefore, we excluded cases witnessed by EMS personnel in which no resuscitation attempt was made by EMS personnel, because cases in which no resuscitation attempt is made have quite different confounding factors from other cases, such as time interval from collapse to start of CPR and providing shock using a defibrillator. Cases in which no resuscitation attempt by EMS personnel was made are defined as those obviously unresuscitable and those who showed no signs of circulation when the EMS arrive at the emergency scene. Moreover, we excluded trauma cases, as in previous studies,16–20 because they differ from medical cardiac arrests with respect to the cause, underlying pathophysiology, and emergency situation, and they generally have extremely poor outcomes compared with cardiac arrest of cardiac origin. Thus, this study focused on cases of non-traumatic OHCA resuscitated before EMS arrival as the target population, regardless of the location of the cardiac arrest, occurring between January 1 to December 31, 2020, and the corresponding period in 2019.
EMS System in Osaka CityAs of March 1, 2021, there were 25 fire stations with 69 ambulances and 1 dispatch center in Osaka City.21 The EMS system was operated by the Osaka Municipal Fire Department with life support provided 24 h every day. The annual number of patients transported by EMS personnel is approximately 200,000. Each ambulance has 3 EMS personnel, including at least 1 emergency life-saving technician (ELST), who provides highly trained emergency care in a prehospital setting. They are allowed to insert an intravenous line and an adjunct airway and use an AED in OHCA patients. Specially trained ELSTs are permitted to insert tracheal tubes and administer adrenaline. All OHCA patients were transported to a hospital, because EMS personnel were instructed to initiate resuscitation unless clear signs of death were present.
Although the EMS protocol affecting OHCA patients’ outcomes did not differ before 2019, during the COVID-19 pandemic, in addition to standard precautions, EMS personnel were required to wear N95 face masks and isolation gowns to deal with cardiac arrest patients. The EMS protocol has encouraged paramedics to use supraglottic airway management instead of endotracheal intubation since April 24, 2020. In addition, when the state of emergency was declared, the fire departments suspended the provision of CPR training to the general public.
Data CollectionThe data form included the date of occurrence, sex, age, origin of cardiac arrest, first documented cardiac rhythm, witness status, location of arrest, activities of daily living (ADL) before arrest, time course of resuscitation, bystander CPR, public-access AED use, dispatcher CPR instruction, advanced airway management, epinephrine administration, prehospital return of spontaneous circulation (ROSC), 1-month survival, and neurological status 1 month after the event. When shocks were administered using a public-access AED, ventricular fibrillation (VF) was the first documented rhythm. No data regarding the number of OHCA patients suspected or diagnosed with COVID-19 were available.
All survivors were followed up for up to 1 month after the event by the EMS personnel in charge. Neurological outcome was ascertained by the physician responsible for the care of the patient, using the Cerebral Performance Category (CPC) scale: category 1, good cerebral performance; category 2, moderate cerebral disability; category 3, severe cerebral disability; category 4, coma or vegetative state; and category 5, death. The primary outcome measure was 1-month survival with a neurologically favorable outcome, defined as CPC score of 1 or 2.
Statistical AnalysisIn addition to the definition of the COVID-19 pandemic, we analyzed the data by wave as categorized by Osaka Prefecture. We aimed to assess the change in bystander and EMS personnel interventions by COVID-19 pandemic wave because each successive wave has been larger than the preceding wave. We divided the study period into 3 periods: January–May (first wave), June–September (second wave), and October–December (third wave). The number of COVID-19 cases in each period was 738 (incidence 26.8/100,000) in the first wave; 4,745 (incidence 172.3/100,000) in the second wave; and 8,660 (incidence 314.4/100,000) in the third wave.12,13 The patients’ baseline characteristics and outcomes were compared between 2019 and 2020 for each of the 3 waves.
Continuous variables are presented as median and interquartile range (IQR), and categorical variables are presented as number and proportion. Patient characteristics, bystander intervention, EMS interventions, and outcomes after OHCA were compared between 2019 and 2020 by the 3 waves using a chi-squared test for categorical variables. Numerical variables that were not normally distributed were analyzed using the Kruskal-Wallis test. To assess the temporal changes in outcomes (prehospital ROSC, 1-month survival, and 1-month with neurologically favorable outcome), we conducted univariable and multivariable logistic regression analyses to provide crude and adjusted odds ratios (AORs) with 95% confidence intervals (CIs), using 2019 as the reference. The explanatory variables considered in the analyses included sex (male or female), age, location (home or other), bystander CPR (yes or no), initial rhythm (VF/pulseless VT [ventricular tachycardia] or other), and time interval from call to hospital as potential confounders based on previous studies.11,22,23
We used SPSS ver.24.0J (IBM Corp., Armonk, NY, USA) for all statistical analyses. All tests were two-sided, and P<0.05 was deemed statistically significant.
Overall, 5,721 OHCAs occurred during the study period; among them, we excluded the following: no resuscitation attempt (n=56), traumatic origin (n=476), and EMS witness (n=398). A total of 4,791 patients (2,420 in 2019 and 2,371 in 2020) were included in the present study (Figure).
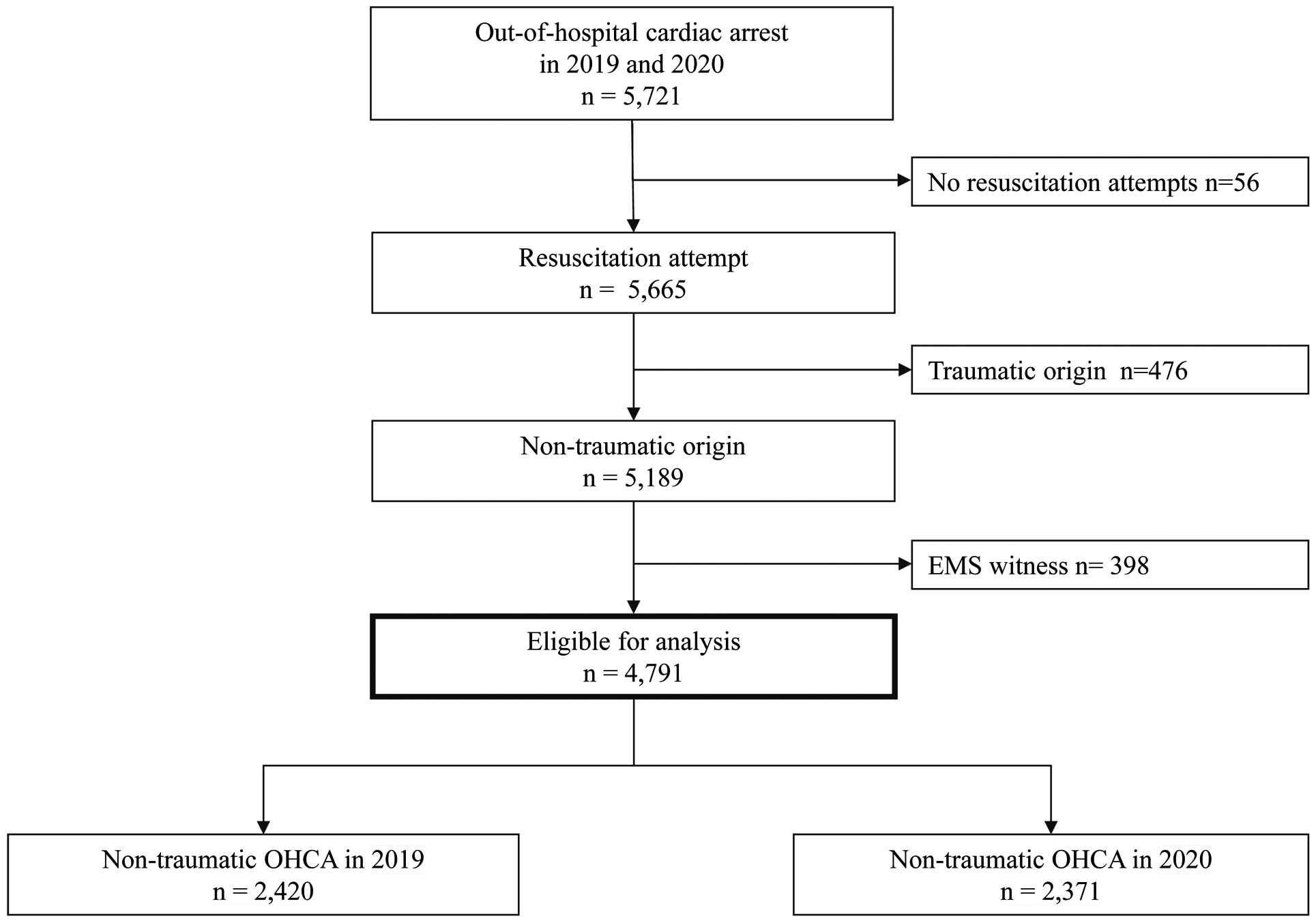
Flowchart showing the selection of patients who experienced an out-of-hospital cardiac arrest (OHCA) between 2019 and 2020.
Patients’ characteristics for the three waves in 2019 and 2020 are reported in Table 1. Between 2019 and 2020, and between each of the 3 waves, there were no statistically significant differences in sex, ADL, witness by bystander status, or VF as the first documented rhythm.
| Overall | 1st wave | 2nd wave | 3rd wave | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 (n=2,420) |
2020 (n=2,371) |
P value | 2019 (n=1,068) |
2020 (n=1,054) |
P value | 2019 (n=671) |
2020 (n=678) |
P value | 2019 (n=681) |
2020 (n=639) |
P value | |
| Age, years, median (IQR) | 78.0 (68.0–86.0) |
80.0 (70.0–87.0) |
0.004 | 78.0 (68.0–86.0) |
79.0 (70.0–86.0) |
0.085 | 77.0 (67.0–86.0) |
79. 0 (70.0–87.0) |
0.044 | 79.0 (69.0–86.0) |
80.0 (70.0–87.0) |
0.193 |
| Men, n (%) | 1,403 (58.0) | 1,384 (58.4) | 0.769 | 616 (57.7) | 611 (58.0) | 0.895 | 395 (58.9) | 394 (58.1) | 0.783 | 392 (57.6) | 379 (59.5) | 0.502 |
| Good ADL before arrest, n (%) | 1,442 (59.6) | 1,379 (58.2) | 0.318 | 653 (61.1) | 635 (60.2) | 0.689 | 380 (56.5) | 385 (56.8) | 0.956 | 409 (60.1) | 359 (56.2) | 0.163 |
| Witnessed by bystander, n (%) | 871 (36.0) | 853 (36.0) | 1.000 | 372 (34.8) | 363 (34.4) | 0.855 | 259 (38.6) | 248 (36.6) | 0.465 | 240 (35.2) | 242 (37.9) | 0.331 |
| Location of arrest, n (%) | 0.060 | 0.049 | 0.185 | 0.690 | ||||||||
| Home | 1,420 (58.7) | 1,443 (60.9) | 633 (59.3) | 668 (63.4) | 391 (58.3) | 390 (57.5) | 396 (58.1) | 385 (60.3) | ||||
| Public place | 447 (18.5) | 377 (15.9) | 203 (19.0) | 160 (15.2) | 124 (18.5) | 106 (15.6) | 120 (17.6) | 111 (17.4) | ||||
| Healthcare facility | 553 (22.9) | 551 (23.2) | 232 (21.7) | 226 (21.4) | 156 (23.2) | 182 (26.8) | 165 (24.2) | 143 (22.4) | ||||
| Cause of cardiac arrest, cardiac, n (%) | 2,126 (87.9) | 2,121 (89.5) | 0.084 | 930 (87.1) | 941 (89.3) | 0.122 | 591 (88.1) | 621 (91.6) | 0.038 | 605 (88.8) | 559 (87.5) | 0.495 |
| VF as the first documented rhythm, n (%) | 201 (8.3) | 212 (8.9) | 0.440 | 76 (7.1) | 91 (8.6) | 0.198 | 61 (9.1) | 88 (11.4) | 0.178 | 64 (9.4) | 44 (6.9) | 0.108 |
ADL, activities of daily living; IQR, interquartile range; OHCA, out-of-hospital cardiac arrest; VF, ventricular fibrillation.
Table 2 shows bystander and EMS interventions in 2019 and 2020 and between each of the 3 waves. There were no statistically significant differences in shocks applied by public-access AEDs, or resuscitation time course. Bystander CPR was significantly less frequently initiated in 2020 than in 2019 (48.0% in 2019 vs. 42.7% in 2020, P<0.001), and this tendency was observed during the first (47.2% in 2019 vs. 42.9% in 2020, P=0.046) and second waves (48.1% in 2019 vs. 41.2% in 2020, P=0.010). However, it was not statistically significant during the third wave (49.2% in 2019 vs. 44.1% in 2020, P=0.066). There was no significant difference in public-access AED applications between 2019 and 2020 (12.9% vs. 11.6%, P=0.158). It was significantly less frequently applied during the first wave (12.6% in 2019 vs. 9.9% in 2020, P=0.043), but was not different during the second wave (12.5% in 2019 vs. 12.8% in 2020, P=0.863) or the third wave (13.7% in 2019 vs. 13.0% in 2020, P=0.722).
| Overall | 1st wave | 2nd wave | 3rd wave | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 (n=2,420) |
2020 (n=2,371) |
P value | 2019 (n=1,068) |
2020 (n=1,054) |
P value | 2019 (n=671) |
2020 (n=678) |
P value | 2019 (n=681) |
2020 (n=639) |
P value | |
| Bystander CPR, n (%) | 1,162 (48.0) | 1,013 (42.7) | <0.001 | 504 (47.2) | 452 (42.9) | 0.046 | 323 (48.1) | 279 (41.2) | 0.010 | 335 (49.2) | 282 (44.1) | 0.066 |
| Public-access AED application, n (%) | 312 (12.9) | 274 (11.6) | 0.158 | 135 (12.6) | 104 (9.9) | 0.043 | 84 (12.5) | 87 (12.8) | 0.863 | 93 (13.7) | 83 (13.0) | 0.722 |
| Shocks by public-access AEDs, n (%) | 48 (2.0) | 32 (1.3) | 0.092 | 21 (2.0) | 16 (1.5) | 0.508 | 11 (1.6) | 9 (1.3) | 0.660 | 16 (2.3) | 7 (1.1) | 0.094 |
| Dispatcher instruction, n (%) | 1,443 (59.6) | 1,426 (60.1) | 0.724 | 637 (59.6) | 674 (63.9) | 0.044 | 412 (61.4) | 395 (58.3) | 0.244 | 394 (57.9) | 357 (55.9) | 0.470 |
| Adrenaline administration, (%) | 657 (27.1) | 612 (25.8) | 0.295 | 296 (27.7) | 303 (28.7) | 0.630 | 179 (26.7) | 145 (21.4) | 0.026 | 182 (26.7) | 164 (25.7) | 0.707 |
| Advanced airway management, n (%) | <0.001 | 0.003 | <0.001 | <0.001 | ||||||||
| Endotracheal intubation | 483 (20.0) | 209 (8.8) | 207 (19.4) | 185 (17.5) | 119 (17.7) | 12 (1.8) | 157 (23.1) | 12 (1.9) | ||||
| Supraglottic airway | 940 (38.8) | 1,290 (54.4) | 417 (39.0) | 488 (46.3) | 262 (39.0) | 395 (58.3) | 261 (38.3) | 407 (63.7) | ||||
| No advanced airway management | 997 (41.2) | 872 (36.8) | 444 (41.6) | 381 (36.1) | 290 (43.2) | 271 (40.0) | 263 (38.6) | 220 (34.4) | ||||
| Response time (call to contact with patient), min, median (IQR) |
6.0 (5.0–8.0) |
6.0 (5.0–8.0) |
0.348 | 6.0 (5.0–8.0) |
6.0 (5.0–8.0) |
0.251 | 6.0 (5.0–8.0) |
6.0 (5.0–8.0) |
0.946 | 6.0 (5.0–8.0) |
6.0 (5.0–8.0) |
0.775 |
| On-scene time (arrival at the scene to dispatch at the hospital), min, median (IQR) |
15.0 (11.0–18.0) |
14.0 (11.0–18.0) |
0.885 | 15.0 (11.0–18.0) |
15.0 (11.0–19.0) |
0.639 | 14.0 (11.0–18.0) |
14.0 (11.0–17.0) |
0.355 | 15.0 (11.0–18.0) |
14.0 (11.0–18.0) |
0.908 |
| Hospital arrival time (call to hospital arrival), min, median (IQR) |
26.0 (22.0–31.0) |
26.0 (22.0–32.0) |
0.970 | 27.0 (22.0–32.0) |
27.0 (22.0–32.0) |
0.513 | 26.0 (22.0–31.0) |
26.0 (21.0–31.0) |
0.800 | 26.0 (22.0–31.0) |
27.0 (22.0–32.0) |
0.233 |
AED, automated external defibrillator; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; IQR, interquartile range; VF, ventricular fibrillation.
There were significant differences in 1-month survival with favorable neurological outcome between 2019 and 2020 (4.6% vs. 3.3%, P=0.018) (Table 3). After adjustment for factors affecting patient outcomes, 1-month survival with favorable neurological outcome was reduced by 28% in 2020 (AOR: 0.72; 95% CI: 0.52–0.99, P=0.044). Although there was a trend toward fewer patients with favorable neurological outcomes in 2019 than in 2020, regardless of the 3 waves, these differences did not reach statistical significance.
| Overall | 1st wave | 2nd wave | 3rd wave | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 (n=2,420) |
2020 (n=2,371) |
P value | 2019 (n=1,068) |
2020 (n=1,054) |
P value | 2019 (n=671) |
2020 (n=678) |
P value | 2019 (n=681) |
2020 (n=639) |
P value | |
| Prehospital ROSC, n (%) | 267 (11.0) | 208 (8.8) | 0.009 | 112 (10.5) | 92 (8.7) | 0.185 | 87 (13.0) | 56 (8.3) | 0.006 | 68 (10.0) | 60 (9.4) | 0.780 |
| Crude OR (95% CI) | Ref. | 0.78 (0.64–0.94) |
0.009 | Ref. | 0.82 (0.61–1.09) |
0.170 | Ref. | 0.60 (0.42–0.86) |
0.005 | Ref. | 0.93 (0.65–1.35) |
0.715 |
| Adjusted OR (95% CI)* | Ref. | 0.77 (0.63–0.95) |
0.012 | Ref. | 0.81 (0.60–1.11) |
0.186 | Ref. | 0.61 (0.41–0.89) |
0.011 | Ref. | 1.00 (0.67–1.49) |
0.998 |
| 1-month survival, n (%) | 181 (7.5) | 149 (6.3) | 0.110 | 77 (7.2) | 73 (6.9) | 0.800 | 52 (7.7) | 38 (5.6) | 0.127 | 52 (7.6) | 38 (5.9) | 0.231 |
| Crude OR (95% CI) | Ref. | 0.83 (0.67–1.05) |
0.115 | Ref. | 0.96 (0.69–1.34) |
0.799 | Ref. | 0.71 (0.46–1.09) |
0.707 | Ref. | 0.78 (0.51–1.21) |
0.781 |
| Adjusted OR (95% CI)* | Ref. | 0.85 (0.66–1.10) |
0.209 | Ref. | 0.93 (0.63–1.37) |
0.717 | Ref. | 0.71 (0.43–1.19) |
0.191 | Ref. | 0.90 (0.55–1.45) |
0.657 |
| Neurologically favorable outcome, n (%) | 112 (4.6) | 78 (3.3) | 0.018 | 49 (4.6) | 35 (3.3) | 0.148 | 34 (5.1) | 25 (3.7) | 0.233 | 29 (4.3) | 18 (2.8) | 0.182 |
| Crude OR (95% CI) | Ref. | 0.70 (0.52–0.94) |
0.018 | Ref. | 0.71 (0.46–1.12) |
0.136 | Ref. | 0.72 (0.42–1.22) |
0.217 | Ref. | 0.65 (0.36–1.19) |
0.161 |
| Adjusted OR (95% CI)* | Ref. | 0.72 (0.52–0.99) |
0.044 | Ref. | 0.65 (0.39–1.08) |
0.096 | Ref. | 0.73 (0.40–1.31) |
0.293 | Ref. | 0.75 (0.40–1.45) |
0.391 |
*Adjusted factors included sex, age, location (home or other), bystander CPR (yes or no), initial rhythm (VF/pulseless VT or other), time interval from call to hospital arrival. CI, confidence interval; OR, odds ratio; ROSC, return of spontaneous circulation.
Using a population-based cohort study in Osaka City, a large metropolitan city in Japan where COVID-19 spread rapidly, we compared patient outcomes, characteristics, bystander interventions, and EMS interventions between 2019 (control period) and 2020 (COVID-19 period) according to the 3 waves of COVID-19 infection. We demonstrated a significant decrease in neurologically favorable outcomes after OHCA and in bystander CPR in the COVID-19 period compared with the control period, but public-access AED application and shocks delivered by a member of the general public were unchanged.
Consistent with previous studies, we demonstrated a negative change in neurological outcomes after OHCA during the COVID-19 period. Previous studies have indicated that during the COVID-19 pandemic many factors, such as an increase in non-shockable rhythm, arrest at home, non-witnessed arrests, less intubation, and delays in emergency response time (call answer to arrival) were associated with worse outcomes.4–6,24–26 In line with many previous reports,4–6,27–29 bystander CPR significantly decreased in 2020 compared with 2019. Contrary to that finding, an online survey carried out by Howell et al indicated that the Australian public’s willingness to perform bystander CPR on a stranger did not change,30 but an international social media survey conducted by Grunau et al in 2020 suggested peoples’ willingness to perform bystander CPR had decreased compared with the pre-pandemic period.31 As a previous study showed a hesitation in rescue breathing among the Japanese general public and healthcare providers;32 people might be hesitant to perform CPR due to a perception that direct patient contact increases the risk of personal harm. As of October 2021, the vaccination rate in Japan was 75.8%;33 however, vaccination had not yet started during the study period. Vaccines are the most effective protection against COVID-19; therefore, the willingness to perform CPR may improve after vaccination has progressed. It is important to reinforce the message to citizens to perform CPR and use an AED to save the life of OHCA patients. Moreover, there is insufficient evidence on whether CPR or AED use is associated with transmission of COVID-19.34,35 Given the proven effectiveness of CPR and AEDs by bystanders, we need to encourage people to assist OHCA patients, as well as ensure rescuer safety.
Although the AED applications decreased in the first wave, usage improved thereafter, and there was no difference between the second and third waves. In the first wave of 2020, when the first state of emergency was declared, bystanders might have been confused about how to perform CPR and use an AED during the COVID-19 pandemic, even if they knew their application was essential for improving survival. Following the international consensus on science and treatment recommendations for resuscitation,36 the Fire and Disaster Management Agency (FDMA) announced the importance of bystander CPR and use of an AED and recommended the general public perform chest compressions and use an AED without rescue breathing on May 22, 2020.37 This updated guidance from the FDMA might be a possible explanation for improved citizen attitudes toward AED use, while their attitude toward CPR did not change. This discrepancy between CPR and AED use may have occurred because it is relatively easier to use an AED than to provide CPR.
Our data showed a significant decrease in 1-month survival with favorable neurological outcome, even after adjusting for prehospital confounding factors. This suggests the existence of unmeasured factors that worsen outcomes. Changes in the quality of CPR performed by EMS personnel or medical staff (e.g., interruption of chest compressions during potentially aerosolizing maneuvers or delay in starting CPR by the precaution process) and the lack of appropriate treatment due to a shortage of intensive care unit (ICU) beds and human resources because of the large number of COVID-19 patients disrupting the capability of the hospital system may have influenced the outcome. In addition, ICU management may have changed since the start of the COVID-19 pandemic, and this may have affected the prognosis during the COVID-19 period.
Study LimitationsFirst, because our data were from a single city in Japan, our findings may not be generalizable to other areas. Further study is needed to evaluate outcomes in Japan using the All-Japan Ustein Registry of the FDMA. Second, our dataset did not include data on hospital treatment. To further evaluate the effect of prehospital interventions, additional studies are needed to combine with data on in-hospital treatment.
In Osaka City, Japan, both neurologically favorable outcomes after OHCA and bystander CPR decreased significantly during the COVID-19 pandemic period, but AED use improved during later waves of the disease.
The study was conducted according to the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects of Japan. This study was approved by the Ethics Committee of Kyoto University (R0416). Personal identifiers of members of the Osaka Fire Department were removed. The requirement for informed consent was waived because of the Personal Information Protection Law and the National Research Ethics Guidelines of Japan.
The operational expenses of this study were met by Kyoto University.
The authors declare that there are no conflicts of interest.
We are greatly indebted to all EMS personnel and concerned physicians in Osaka City for their cooperation in collecting the data and maintaining the quality of data.
The deidentified participant data will not be shared.