論文ID: CJ-23-0177
論文ID: CJ-23-0177
Background: Little is known about how to effectively increase bystander cardiopulmonary resuscitation (CPR), so we evaluated the 10-year trend of the proportion of bystander CPR in an area with wide dissemination of chest compression-only CPR (CCCPR) training combined with conventional CPR training.
Methods and Results: We conducted a descriptive study after a community intervention, using a prospective cohort from September 2010 to December 2019. The intervention consisted of disseminating CCCPR training combined with conventional CPR training in Toyonaka City since 2010. We analyzed all non-traumatic out-of-hospital cardiac arrest (OHCA) patients resuscitated by emergency medical service personnel. The primary outcome was the trend of the proportion of bystander CPR. We conducted multivariate logistic regression models and assessed the adjusted odds ratio (AOR) using a 95% confidence interval (CI) to determine bystander CPR trends. Since 2010, we have trained 168,053 inhabitants (41.9% of the total population of Toyonaka City). A total of 1,508 OHCA patients were included in the analysis. The proportion of bystander CPR did not change from 2010 (43.3%) to 2019 (40.0%; 1-year incremental AOR 1.02 [95% CI: 0.98–1.05]).
Conclusions: The proportion of bystander CPR did not increase even after wider dissemination of CPR training. In addition to continuing wider dissemination of CPR training, other strategies such as the use of technology are necessary to increase bystander CPR.
Out-of-hospital cardiac arrest (OHCA) is a public health concern in many countries,1,2 and bystander cardiopulmonary resuscitation (CPR) plays a key role in increasing survival after an OHCA.3 However, the proportion of bystander CPR varies widely and is insufficient in many areas.4 In addition, the importance of high-quality CPR is emphasized to improve survival,5 and therefore initiatives to increase performance of high-quality CPR by bystanders in the community are needed.
The core intervention to increase bystander CPR is public education.6 In Japan, CPR education has been provided mainly by fire departments, but conventional CPR training programs require significant labor, time, and cost, which can be burdensome for both instructors and trainees.7,8 Several clinical studies have highlighted the effectiveness of chest compression-only CPR (CCCPR) compared with chest compression plus rescue breathing (conventional CPR) in most cardiac arrest situations.9,10 In addition, CCCPR training is easier to learn and perform, and accurate chest compression can be taught in a shorter training course.11–14 This simplified version may aid wider dissemination of CPR by expanding educational opportunities and overcoming barriers to bystanders performing CPR.
In Toyonaka City, Osaka Prefecture, we have been providing CPR training for residents by offering CCCPR training in conjunction with conventional CPR training since 2010. We have previously reported an increase in the proportion of high-quality bystander CPR, but not in the proportion of bystander CPR over a 5-year period.15 There are some possible explanations for the lack of increase in bystander CPR performance during the first 5 years, including insufficient spread of CPR training in the community. There are few reports to evaluate and verify the effect of these community initiatives over a longer period. The purpose of this study was to describe how the proportion of CPR and high-quality CPR by bystanders changed over a 10-year period when CCCPR training combined with conventional CPR training was provided.
This descriptive study was conducted using a prospective cohort from September 2010 to December 2019. The data from October 2013 to September 2014 were not available and were treated as excluded.
Toyonaka City in Osaka Prefecture, Japan, is a part of the Osaka metropolitan area, with an increasing population of 400,496 residents as of December 2019.16 The population density is high at 10,492 persons/km2 in December 2019.16
Emergency Medical Service (EMS) System in Toyonaka CityThe EMS system in Toyonaka City is the same as that across Japan. Toyonaka City has 9 fire stations with 12 ambulances and 1 dispatch center, which provide 24-h emergency services. In the event of an OHCA, anyone may call for an ambulance using the emergency number (119), and the dispatcher provides CPR instructions until EMS arrival. The average time from call to EMS arrival at the scene in Toyonaka City is 6.1 min, which is less than the national average of 8.7 min.1,17 Each ambulance has 3 personnel, including at least 1 emergency life support technician (ELST), who is highly trained for emergency care in the prehospital setting. The ELST is authorized to administer adrenaline (epinephrine) and advanced airway management. Currently, the Japanese system prohibits paramedics from terminating or not performing resuscitation. Therefore, all OHCA patients are transported to the hospital while being resuscitated, except when obviously unresuscitable (dead) or exhibiting no signs of circulation when the EMS arrives at the emergency scene.
Dissemination of CPR Training in the Community Since 2010Prior to 2010, the Toyonaka City Fire Department was offering 3- or 8-h conventional CPR training courses, including chest compressions, rescue breathing, and automated external defibrillator (AED) use, to citizens, including businesses, government organizations, and nursing facilities. Approximately 2% of the total population participated annually.15 In addition to conventional CPR training, a 45-min CCCPR training program with chest compressions and AED use was launched in 2010. (Details of the training program have been previously described.15) In Japan, CPR training program have been comprehensively administered in schools in only a few areas. In cooperation with Toyonaka City, we systematically provided the 45-min CCCPR training to all 5th and 6th-grade elementary school students and junior high school students to provide CPR training to 4–5% of the local population annually. The content of the community intervention did not change throughout the study period.
Study ParticipantsTo analyze the relationship between the dissemination of CPR training in the community and the performance of bystander CPR, we included all OHCA patients with a medical origin that were resuscitated by EMS personnel. Based on the international standardized Utstein-style guidelines,18 we excluded patients with cardiac arrest witnessed by EMS personnel and those occurring in nursing facilities, because potential confounding factors for outcomes such as time interval from collapse to starting CPR and providing shock using a defibrillator are different from other cases. Because cases of traumatic cardiac arrest differ from those of medical etiology, underlying pathophysiology, and emergency, we also excluded trauma cases.
Data Collection and DefinitionAs CPR training data, we collected the following: date of CPR training, type of CPR training program, number of participants, and participant attributes (elementary school students, junior high school students, high school students, university students, schoolteachers and parents, local community organizations, corporate employees, nursing/hospital facility employees, government employees, and others). We collected the following OHCA patient data based on the Utstein-style guidelines:18 sex, age, activities of daily living (ADL), witness, location of arrest, dispatcher CPR instruction, shocked by public access AED, first documented cardiac rhythm, cause of cardiac arrest, time from call to CPR by EMS personnel, bystander CPR, 1-month survival, and 1-month survival with favorable neurological outcomes defined as a cerebral performance category of 1 or 2 when measured.
We also collected the quality of bystander CPR by EMS personnel who observed the bystanders performing CPR in the field and evaluated the following 3 points: hand positions (correct: midpoint of nipples, incorrect: others, not assessable), chest compression rates (too slow: <100/min, correct: 100–120/min, too fast: ≥120/min, not assessable), and compression depth (correct: ≥4 cm, incorrect: others, not assessable). Cases in which all 3 points were correct were defined as high-quality bystander CPR.
To maintain the accuracy of the assessment of bystander CPR, the EMS personnel took an assessment test after studying 11 different CPR cases via video. The test was a multiple-choice exam using the above assessment criteria for 24 different CPR cases and they required a kappa statistic >0.8. Details of the training program have been previously described.15
OutcomesThe primary outcome was the trend of the proportion of bystander CPR. The secondary outcomes were the trend of the proportion of high-quality bystander CPR, 1-month survival, and 1-month survival with favorable neurological outcomes.
Statistical AnalysisWe described the patients’ characteristics by year from 2010 to 2019. Continuous variables are presented as the median and interquartile range, and categorical variables are presented as numbers and proportions.
The proportions of bystander CPR and high-quality bystander CPR were calculated for each year. We used logistic regression analysis to calculate the odds ratio (OR) (95% confidence interval [CI]) and adjusted OR (AOR) (95% CI) to assess 1-year increment changes, using data in 2010 as the base year when the community intervention started. We adjusted for covariates considered clinically associated with outcome based on previous studies,19–21 including sex, age, ADL (good/poor), witness (yes/no), and location (public place/other). Of the variables used for estimation, only the location variable had 25 missing values. Therefore, the estimation was performed using multiple imputation by “mice” package.
We considered two-sided P<0.05 to be statistically significant. All statistical analyses were performed using JMP (version 15.1; SAS Institute Inc., Cary, NC, USA), R (version 4.0.3; The R Foundation for Statistical Computing, Vienna, Austria), and EZR (version 1.41; Saitama Medical Center, Jichi Medical University, Saitama, Japan).
Ethical ApprovalThe study was conducted according to the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects of Japan. This study was approved by the Ethics Committee of the Graduate School of Medicine, Kyoto University (R2790). The data were already anonymized at the Toyonaka City Fire Department, and consent was not able to be obtained from participants.
From September 2010 to December 2019, the Toyonaka City Fire Department trained a cumulative total of 168,053 trainees: 95,043 in the 45-min CCCPR training and 73,010 in the conventional CPR training, which accounted for 41.9% of the Toyonaka City population (400,496 residents as of December 2019) (Figure 1). The demographics of the participants in the CCCPR training program are shown in Figure 2. In the CCCPR training program, most trainees were 5th- and 6th-grade elementary school students (29,785 [30.5%]), followed by junior high school students (22,286 [22.8%]).

Cumulative number of trainees as a proportion of the total population of Toyonaka City. CPR, cardiopulmonary resuscitation.
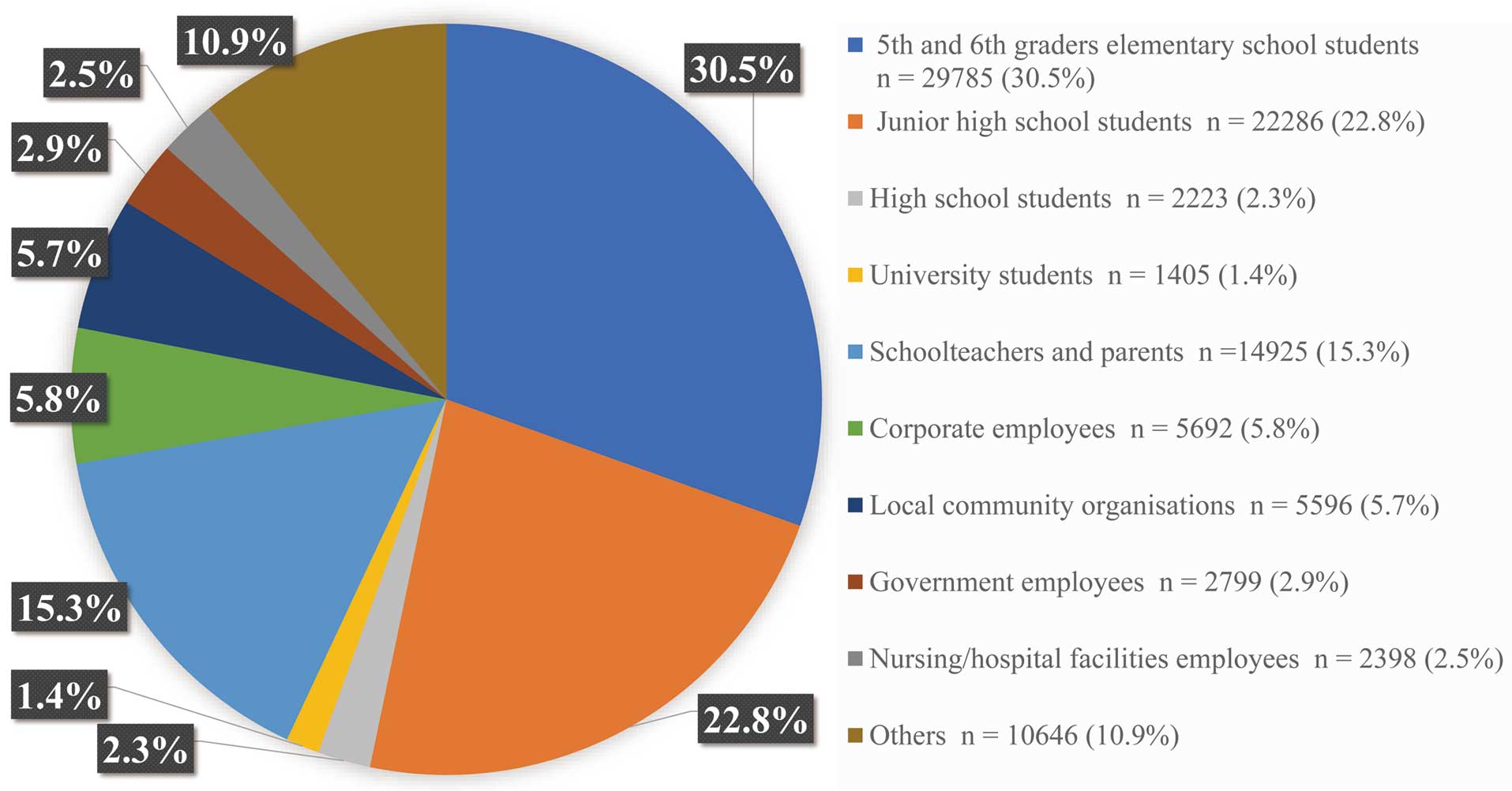
Demographics of participants in chest compression-only training from 2010 to 2019 in Toyonaka city.
Patients and Their Characteristics
Over the study period, 2,796 OHCAs occurred in Toyonaka City, of whom 2,147 non-traumatic OHCA cases resuscitated by EMS personnel were documented. Among them, 1,508 patients were included in the analysis after excluding 198 cases witnessed by EMS personnel and 441 occurring in nursing facilities (Figure 3). In the evaluation of the quality of bystander CPR, of the 675 cases in which bystander CPR was performed, 173 cases for which quality data were not available were excluded, and the remaining 502 cases were included in the analysis.

Patient flow chart. CPR, cardiopulmonary resuscitation; EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest.
The characteristics of the patients, by year from 2010 to 2019, are shown in Table 1. The median age was 77–80 years and the proportion of males ranged from 51.7% to 71.0%. Witnessed cardiac arrests accounted for 36.9–62.6%, with 58.9–90.4% occurring at home. Cardiogenic cardiac arrests accounted for 85.1–93.3%, but the first documented rhythm was shockable in 5.5–13.9%, and patients shocked by public access AEDs comprised 0–1.8% of cases. Dispatcher CPR instruction was given in 63.9–75.5% of cases. The median time from call to CPR by EMS personnel was 6–8 min.
Temporal Trends in Patient and Resuscitation Characteristics of OHCA With Medical Origin
| 2010 (n=60) |
2011 (n=154) |
2012 (n=158) |
2013 (n=107) |
2014 (n=55) |
2015 (n=188) |
2016 (n=168) |
2017 (n=216) |
2018 (n=222) |
2019 (n=180) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Sex, male, n (%) | 31 (51.7) | 91 (59.1) | 102 (64.6) | 76 (71.0) | 29 (52.7) | 115 (61.2) | 101 (60.1) | 125 (57.9) | 135 (60.8) | 121 (67.2) |
| Age, years, median (IQR) | 80 (73–85) | 78 (65–85) | 79 (67–85) | 80 (70–85) | 80 (70–89) | 77 (65–83) | 78 (69–84) | 78 (67–86) | 77 (68–84) | 77 (68–85) |
| ADL before arrest, good, n (%) | 32 (53.3) | 98 (63.6) | 101 (63.9) | 64 (59.8) | 32 (58.2) | 124 (66.0) | 121 (72.0) | 143 (66.2) | 148 (66.7) | 117 (65.0) |
| Bystander-witnessed arrest, n (%) | 28 (46.7) | 68 (44.2) | 72 (45.6) | 67 (62.6) | 29 (52.7) | 95 (50.5) | 73 (43.5) | 99 (45.8) | 82 (36.9) | 72 (40.0) |
| Witnessed by family members | 22 (36.7) | 56 (36.4) | 49 (31.0) | 43 (40.2) | 19 (34.5) | 70 (37.2) | 47 (28.0) | 68 (31.5) | 52 (23.4) | 53 (29.4) |
| Witnessed by others | 6 (10.0) | 12 (7.8) | 23 (14.6) | 24 (22.4) | 10 (18.2) | 25 (13.3) | 26 (15.5) | 31 (14.4) | 30 (13.5) | 19 (10.6) |
| Unwitnessed | 32 (53.3) | 86 (55.8) | 86 (54.4) | 40 (37.4) | 26 (47.3) | 93 (49.5) | 95 (56.5) | 117 (54.2) | 140 (63.1) | 108 (60.0) |
| Location of arrest, n (%) | ||||||||||
| Home | 52 (86.7) | 134 (87.0) | 126 (79.7) | 63 (58.9) | 49 (89.1) | 170 (90.4) | 141 (83.9) | 179 (82.9) | 185 (83.3) | 150 (83.3) |
| Public place | 3 (5.0) | 16 (10.4) | 23 (14.6) | 19 (17.8) | 6 (10.9) | 15 (8.0) | 21 (12.5) | 29 (13.4) | 29 (13.1) | 20 (11.1) |
| Other | 5 (8.3) | 4 (2.6) | 9 (5.7) | 2 (1.9) | 0 | 2 (1.1) | 5 (3.0) | 8 (3.7) | 8 (3.6) | 10 (5.6) |
| Missing | 0 | 0 | 0 | 23 (21.5) | 0 | 1 (0.5) | 1 (0.6) | 0 | 0 | 0 |
| First documented cardiac rhythm, shockable rhythm, n (%) | 8 (13.6) | 14 (9.1) | 15 (9.5) | 10 (9.3) | 3 (5.5) | 16 (8.5) | 16 (9.5) | 18 (8.3) | 18 (8.1) | 25 (13.9) |
| Cause of cardiac arrest, cardiac, n (%) | 54 (90.0) | 131 (85.1) | 136 (86.1) | 94 (87.9) | 47 (85.5) | 173 (92.0) | 149 (88.7) | 201 (93.1) | 196 (88.3) | 168 (93.3) |
| Dispatcher CPR instructions, n (%) | 40 (66.7) | 108 (70.1) | 101 (63.9) | 77 (72.0) | 40 (72.7) | 138 (73.4) | 120 (71.4) | 163 (75.5) | 156 (70.3) | 124 (68.9) |
| Shocked by public access AED, n (%) | 0 | 1 (0.6) | 2 (1.3) | 1 (0.9) | 1 (1.8) | 1 (0.5) | 0 | 2 (0.9) | 1 (0.5) | 2 (1.1) |
| Time from call to CPR by EMS personnel, min, median (IQR) | 7 (6–8) | 8 (6–9) | 7 (6–9) | 7 (5–8) | 6 (5–8) | 6 (5–7) | 6 (5–7) | 6 (5–7) | 7 (6–8) | 7 (6–9) |
ADL, activities of daily living; AED, automated external defibrillator; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; IQR, interquartile range; OHCA, out-of-hospital cardiac arrest.
Bystander CPR and High-Quality CPR
Figure 4 shows the 10-year trends of the proportions of bystander CPR and high-quality bystander CPR. The proportion of bystander CPR was 43.3% in 2010 and 40.0% in 2019, and the proportion of high-quality bystander CPR was 11.7% in 2010 and 20.0% in 2019. There were no statistically significant improvements in the proportion of bystander CPR (OR for a 1-year increase 1.01; 95% CI 0.98–1.05, AOR for a 1-year increase 1.02; 95% CI 0.98–1.05). However, there was statistically significant improvement in the proportion of high-quality bystander CPR (OR for a 1-year increase 1.09; 95% CI 1.04–1.15, AOR for a 1-year increase 1.09; 95% CI 1.04–1.14).

Temporal trend in proportions of bystander CPR and high-quality bystander CPR. We used logistic regression analysis to calculate the OR (95% CI) and adjusted OR (95% CI) to assess 1-year increment changes, using data in 2010 as the base year when the community intervention started. We adjusted for covariates considered clinically associated with outcome, including sex, age, activities of daily living, witness of arrest and location. The proportion of bystander CPR did not increase, but high-quality bystander CPR showed an increasing trend. CI, confidence interval; CPR, cardiopulmonary resuscitation; OR, odds ratio.
Details of the Quality of Bystander CPR
Table 2 shows the 10-year trends in quality of bystander CPR. Correct hand position was 76.5% in 2010 and 94.8% in 2019, correct chest compression rate was 58.8% in 2010 and 82.8% in 2019, and correct compression depth was 41.2% in 2010 and 65.5% in 2019.
Temporal Trend in Quality of Bystander CPR
| 2010 (n=17) |
2011 (n=38) |
2012 (n=56) |
2013 (n=33) |
2014 (n=18) |
2015 (n=58) |
2016 (n=59) |
2017 (n=82) |
2018 (n=83) |
2019 (n=58) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Hand positions, n (%) | ||||||||||
| Correct | 13 (76.5) | 33 (86.8) | 41 (73.2) | 29 (87.9) | 17 (94.4) | 53 (91.4) | 51 (86.4) | 77 (93.9) | 74 (89.2) | 55 (94.8) |
| Incorrect | 4 (23.5) | 5 (13.2) | 11 (19.6) | 3 (9.1) | 1 (5.6) | 4 (6.9) | 7 (11.9) | 5 (6.1) | 9 (10.8) | 3 (5.2) |
| Not assessable |
0 | 0 | 4 (7.1) | 1 (3.0) | 0 | 1 (1.7) | 1 (1.7) | 0 | 0 | 0 |
| Chest compressions rate, n (%) | ||||||||||
| Correct: 100–120/min |
10 (58.8) | 32 (84.2) | 29 (51.8) | 25 (75.8) | 15 (83.3) | 44 (75.9) | 48 (81.4) | 72 (87.8) | 66 (79.5) | 48 (82.8) |
| Too fast: >120/min |
1 (5.9) | 1 (2.6) | 9 (16.1) | 1 (3.0) | 1 (5.6) | 1 (1.7) | 4 (6.8) | 5 (6.1) | 6 (7.2) | 1 (1.7) |
| Too slow: <100/min |
5 (29.4) | 3 (7.9) | 12 (21.4) | 5 (15.2) | 0 | 10 (17.2) | 5 (8.5) | 4 (4.9) | 11 (13.3) | 9 (15.5) |
| Not assessable |
1 (5.9) | 2 (5.3) | 6 (10.7) | 2 (6.1) | 2 (11.1) | 3 (5.2) | 2 (3.4) | 1 (1.2) | 0 | 0 |
| Chest compression depth, n (%) | ||||||||||
| Correct | 7 (41.2) | 25 (65.8) | 27 (48.2) | 21 (63.6) | 13 (72.2) | 41 (70.7) | 43 (72.9) | 61 (74.4) | 59 (71.1) | 38 (65.5) |
| Incorrect | 10 (58.8) | 10 (26.3) | 26 (46.4) | 11 (33.3) | 5 (27.8) | 15 (25.9) | 15 (25.4) | 17 (20.7) | 23 (27.7) | 19 (32.8) |
| Not assessable |
0 | 3 (7.9) | 3 (5.4) | 1 (3.0) | 0 | 2 (3.4) | 1 (1.7) | 4 (4.9) | 1 (1.2) | 1 (1.7) |
Abbreviations as in Table 1.
Survival
Table 3 shows the 10-year trends in survival. The 1-month survival was 8.3% in 2010 and 7.8% in 2019, and the 1-month survival with favorable neurological outcome was 5.0% in 2010 and 4.4% in 2019.
Temporal Trends in 1-Month Survival and 1-Month Survival With Favorable Neurological Outcome
| 2010 (n=60) |
2011 (n=154) |
2012 (n=158) |
2013 (n=107) |
2014 (n=55) |
2015 (n=188) |
2016 (n=168) |
2017 (n=216) |
2018 (n=222) |
2019 (n=180) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| 1-month survival, n (%) | 5 (8.3) | 8 (5.2) | 15 (9.5) | 11 (10.3) | 4 (7.3) | 11 (5.9) | 13 (7.7) | 17 (7.9) | 15 (6.8) | 14 (7.8) |
| 1-month survival with favorable neurological outcome, n (%) |
3 (5.0) | 3 (1.9) | 8 (5.1) | 7 (6.5) | 1 (1.8) | 6 (3.2) | 9 (5.4) | 11 (5.1) | 9 (4.1) | 8 (4.4) |
Since 2010 we have strategically disseminated CCCPR training in addition to conventional CPR training in Toyonaka City and successfully provided training to 41.9% of residents. However, the proportion of bystander CPR did not change despite 10 years of aggressive CPR training. Although the proportion of high-quality bystander CPR gradually increased, both the proportion of 1-month survival and 1-month survival with favorable neurological outcomes did not change.
Despite this result differing from our hypothesis, this information is valuable for understanding the difficulties in increasing the performance of CPR by bystanders in community through public education, because few studies have evaluated this outcome in the community over long periods. Although various efforts to increase bystander CPR through other interventions have been introduced, such as the introduction and improvement of dispatcher CPR instruction and publicity campaigns using mass media,22–26 it is difficult to identify specific interventions that have had a significant effect. Before starting this study, most of the interventions that could have influenced the proportion of bystander CPR, such as the implementation of dispatcher CPR instruction, public awareness campaigns toward CPR, and conventional CPR training, had been implemented in Toyonaka City, and the proportion of bystander CPR at the starting point was higher than in other areas of Japan.27 We strategically introduced simplified CCCPR training where these other community interventions were well implemented and in order to demonstrate an increase in bystander CPR and survival after OHCA. Although the results of this study were negative, it was important to disclose them because they provide substantial evidence of the need for additional intervention.
We assessed the quality of bystander CPR at the scene and found that it had increased over the study period. Because the quality of bystander CPR is related to survival,28 high-quality CPR by not only EMS personnel, but also citizens will increase a patient’s chances of survival after OHCA. Thus, it is important to understand the quality of bystander CPR in the community. However, assessing the quality of bystander CPR in the prehospital setting is not as easy as assessing the quality of CPR by healthcare providers in hospitals or by EMS personnel, who have access to accelerometers and defibrillators that may be objectively evaluated. For these reasons, few reports have evaluated the quality of bystander CPR using limited parameters such as compression rate and compression fraction collected by emergency call records.29 Therefore, the results of this study are valuable in providing a long-term, comprehensive assessment of the quality of bystander CPR throughout a region in which CPR training has been aggressively provided. As shown in Table 2, the detailed data on the quality of bystander CPR suggested that the proportion of chest compressions with correct depth had been low but seems to have improved over time with the cumulative increase of CPR training in this community. Previous studies have shown that compression depth is inaccurate even in CPR performed by healthcare providers.30–32 Our study newly revealed that providing chest compressions with correct depth was difficult for citizen bystanders, but can be improved by wider dissemination of CPR training in the community. For citizens, to acquire and maintain correct chest compression skills, the simplified CCCPR training may be most useful, as previously reported.12,14
There are several possible explanations why the proportion of bystander CPR did not increase despite the dissemination of CPR training for over 40% of residents during the 10-year period. First, the proportion of bystander CPR was already relatively high at 40.3% in 2009. Although CPR education plays a major in role in increasing bystander CPR, it has been reported that untargeted education is ineffective except in areas with a high incidence of cardiac arrest or a low proportion of bystander CPR.33,34 Given that the proportion of bystander CPR in Toyonaka City before staring the study was high, it would be relatively difficult to further increase bystander CPR and thus a more targeted strategy might be needed.
Second, more than half of the participants in the CCCPR training were elementary school students and junior high school students, and they might have had a low chance of encountering a cardiac arrest during the study period. In Norway, where bystander CPR has reached 80%, CPR education has been offered in schools since the 1960s. It may take longer to increase the proportion of bystander CPR through school education, although CPR training in school has been recommended in resuscitation guidelines and policies6,35,36 to provide CPR training to all groups of society. CPR retraining is also necessary because CPR skills and knowledge deteriorate over time.37,38 After graduating from high school, the only mandated CPR training in Japan is at the time of obtaining a driving license (mostly around the age of 20).39 We have started another strategy to disseminate CPR training that targets middle-aged and older adults who have more chance of encountering a cardiac arrest.
Third, the response time interval from call to EMS arrival at the patient’s side, which is an important factor in improving survival, is very short in Toyonaka City (6.1 min),1,17 which means bystanders in this area have limited time to initiate CPR. Fourth, Toyonaka City is an urban area with significant annual migration of residents (20,000 residents per year, both inflow and outflow).16 In addition, the day/night residents ratio is ≈88%, meaning that more residents move out of the city during the daytime compared with the nighttime.16 These factors may reduce the effectiveness of CPR training in the community.
Our results clearly demonstrate that further increasing the proportion of bystander CPR in an area where it is already high is not easy. Although the proportion of high-quality bystander CPR increased, 1-month survival did not improve. To improve the outcome of OHCA patients, it is necessary to further increase the proportion of high-quality bystander CPR. According to recent reports, bystander CPR can be increased by using smartphones to provide information about the location of OHCA to citizen volunteers who can rush to the scene.40,41 In addition to conventional efforts including CPR training, advertisements, and dispatcher instructions, such new approaches are required to increase bystander CPR. Although the use of this technology has allowed citizen volunteers trained in CPR to easily go to the scene of a cardiac arrest, as many volunteers as possible need to be trained in CPR to utilize such technologies. The combination of new technologies and CCCPR training, which can train many volunteers at once, would aid in increasing high-quality bystander CPR and improve survival in the community.
Study LimitationsFirst, because we assessed the trend of bystander CPR in a community, we cannot prove a causal relationship between the dissemination of CCCPR and the change in bystander CPR. Second, the quality of bystander CPR was acquired subjectively by EMS personnel and may be biased. We conducted a pre-assessment test on the EMS personnel who were the evaluators and kept a kappa statistic >0.8 to equalize the quality of the evaluators and to ensure the quality of the data obtained. Recently, live video from a bystander’s smartphone was used to provide the dispatcher with information from the scene of a cardiac arrest.42 We also may consider the use of such technology to improve the quality of data in the future. Third, bystander CPR may be influenced by local cultural and prehospital emergency care systems. Therefore, it may be difficult to apply our results to other regions. Fourth, we had no control area that did not actively provide training in this study. In practice, however, it might be very difficult to select an area as control for the following reasons. First, to ensure comparability, it is necessary to select regions with similar population sizes, similar proportions of elderly and young people, similar local conditions such as medical facilities, and similar proportions of bystander CPR. Such areas are hard to find. Second, in the current context where hands-only CPR has been established as one of the training methods for the general public, it would be challenging for us to gain support from residents, governments, and other stakeholders if active training cannot be conducted due to being designated as a control area. For these reasons, it might be very difficult to set up a control area. Finally, we were unable to identify the number of people who took the training multiple times or those who moved out of the area. Therefore, the percentage of participants in CPR training may be overestimated.
The proportion of bystander CPR did not increase after wider dissemination of CCCPR training combined with conventional CPR training in the community over a 10-year period. In addition to continuing strategic CPR training and considering effective teaching methods and targets, other approaches such as the use of technology are necessary to increase bystander CPR and improve outcomes after OHCA.
We thank the Toyonaka City Fire Department for their CPR education and data collection.
This study was supported by the Laerdal Foundation for Acute Medicine and a Grant-in-Aid for Health and Labour Sciences Research Grants (H21-Shinkin-001; H24-Shinkin-Ippan-001; H27-Shinkin-Ippan-004; H29-Junkankitou-Ippan-009; 20FA1014; 23FA1023) from the Japanese Ministry of Health; Labour and Welfare.
None declared.
This study was approved by the Ethics Committee of the Graduate School of Medicine, Kyoto University (R2790).
The data of this study will not to be made available.