論文ID: CJ-23-0271
論文ID: CJ-23-0271
Background: In patients with atrial fibrillation (AF) and severe blood stasis in the left atrial appendage (LAA), dense spontaneous echo contrast (SEC) disturbs the distinct visualization of the LAA interior, thus making thrombus diagnosis inconclusive. We aimed to prospectively assess the efficacy and safety of a protocol for a low-dose isoproterenol (ISP) infusion to reduce SEC to exclude an LAA thrombus.
Methods and Results: We enrolled 17 patients with AF and dense SEC (Grade 4 or sludge). ISP was infused with gradually increasing doses of 0.01, 0.02, and 0.03 μg/kg/min at 3-min intervals. After increasing the dose to 0.03 μg/kg/min for 3 min, or when the LAA interior was visible, the infusion was terminated. We reassessed the SEC grade, presence of an LAA thrombus, LAA function, and left ventricular ejection fraction (LVEF) within 1 min of ISP termination. Compared with baseline, ISP significantly increased LAA flow velocity, the LAA emptying fraction, LAA wall velocities, and LVEF (all P<0.01). ISP administration significantly reduced the SEC grade (median) from 4 to 1 (P<0.001). The SEC grade decreased to ≤2 in 15 (88%) patients, and the LAA thrombus was excluded. There were no adverse events.
Conclusions: Low-dose ISP infusion may be effective and safe to reduce SEC and exclude an LAA thrombus by improving LAA function and LVEF.
The worldwide prevalence and incidence of atrial fibrillation (AF) have been progressively increasing against the backdrop of an aging society.1 Electrical cardioversion, catheter ablation, and percutaneous left atrial appendage (LAA) closure are the substantial therapeutic options for patients with AF. A pre-existing left atrial (LA)/LAA thrombus is an absolute contraindication for patients undergoing the abovementioned planned procedures due to the high risk of intervention-related thromboembolism.1 Transesophageal echocardiography (TEE) has evolved as the gold standard method of thrombus identification, particularly in LAA.2–4 Despite substantial improvement in TEE image quality in recent years, a dense smoke-like echo, termed spontaneous echo contrast (SEC), occasionally interferes with distinct visualization of the LAA interior in AF patients with severe blood stasis in LAA, rendering the diagnosis of thrombus inconclusive.3,4 Thus, a reliable method of discrimination between dense SEC and a thrombus by TEE is essential to avoid intervention-related thromboembolism and inappropriate cancellation of interventions.
Echogenicity of blood due to a rouleaux formation of erythrocytes caused by significantly slow blood flow is one of the mechanisms underlying SEC formation.4,5 Infusion of isoproterenol (ISP), a β-adrenergic receptor agonist, during TEE reduces dense SEC and allows the exclusion of an LAA thrombus.6,7 Considering the mechanism of SEC formation, ISP infusion may be a promising method and a novel entity of pharmacologic stress echocardiography to diagnose or exclude LAA thrombus in patients with severe blood stasis and dense SEC caused by AF. However, there are only a limited number of studies on ISP stress echocardiography for this purpose.8,9 Moreover, the methods of ISP administration have not yet been completely standardized. Therefore, the present study proposed a low-dose ISP infusion protocol and prospectively assessed its efficacy and safety in lowering dense SEC to exclude LAA thrombus in patients with AF. Furthermore, we aimed to examine the impact of low-dose ISP on cardiac function and the mechanism by which ISP reduces SEC.
This single-arm prospective study, conducted between January 2021 and December 2022, was designed to evaluate the efficacy and safety of low-dose ISP infusion to diagnose or exclude an LAA thrombus in patients with AF and dense SEC. Each patient provided written informed consent prior to the commencement of the study. The study was performed in accordance with the Clinical Trials Act in Japan (jRCT number: s031200261) because of the off-label use of ISP. It was registered with the Japan Registry of Clinical Trials (jRCTs031200261; https://jrct.niph.go.jp/latest-detail/jRCTs031200261) and was performed according to the principles of Declaration of Helsinki. The study was approved by the Tsukuba University Clinical Research Review Board (TCRB20-20).
The main inclusion criteria were as follows: patients with valvular or non-valvular AF undergoing TEE; patients receiving anticoagulant therapy; patients with Grade 3 or 4 SEC or sludge (defined later) in the LA and LAA; and patients in whom it was difficult to exclude the LAA thrombus. The main exclusion criteria were: a history of LAA occlusion or resection; sinus rhythm during TEE; obvious LAA thrombus without ISP infusion; systolic blood pressure (SBP) ≤80 or ≥180 mmHg or heart rate (HR) ≥100 beats/min before the commencement of TEE; hypertrophic cardiomyopathy with significant left ventricle (LV) obstruction; and disorientation, quadriplegia, dysarthria, and visual field impairment before TEE. Detailed inclusion and exclusion criteria are provided in the Supplementary Methods.
In all, 17 patients were enrolled in this study (Figure 1). All patients received adequate anticoagulation therapy during TEE. Details of anticoagulation and AF types, along with the definition of congestive heart failure, are provided in the Supplementary Methods.
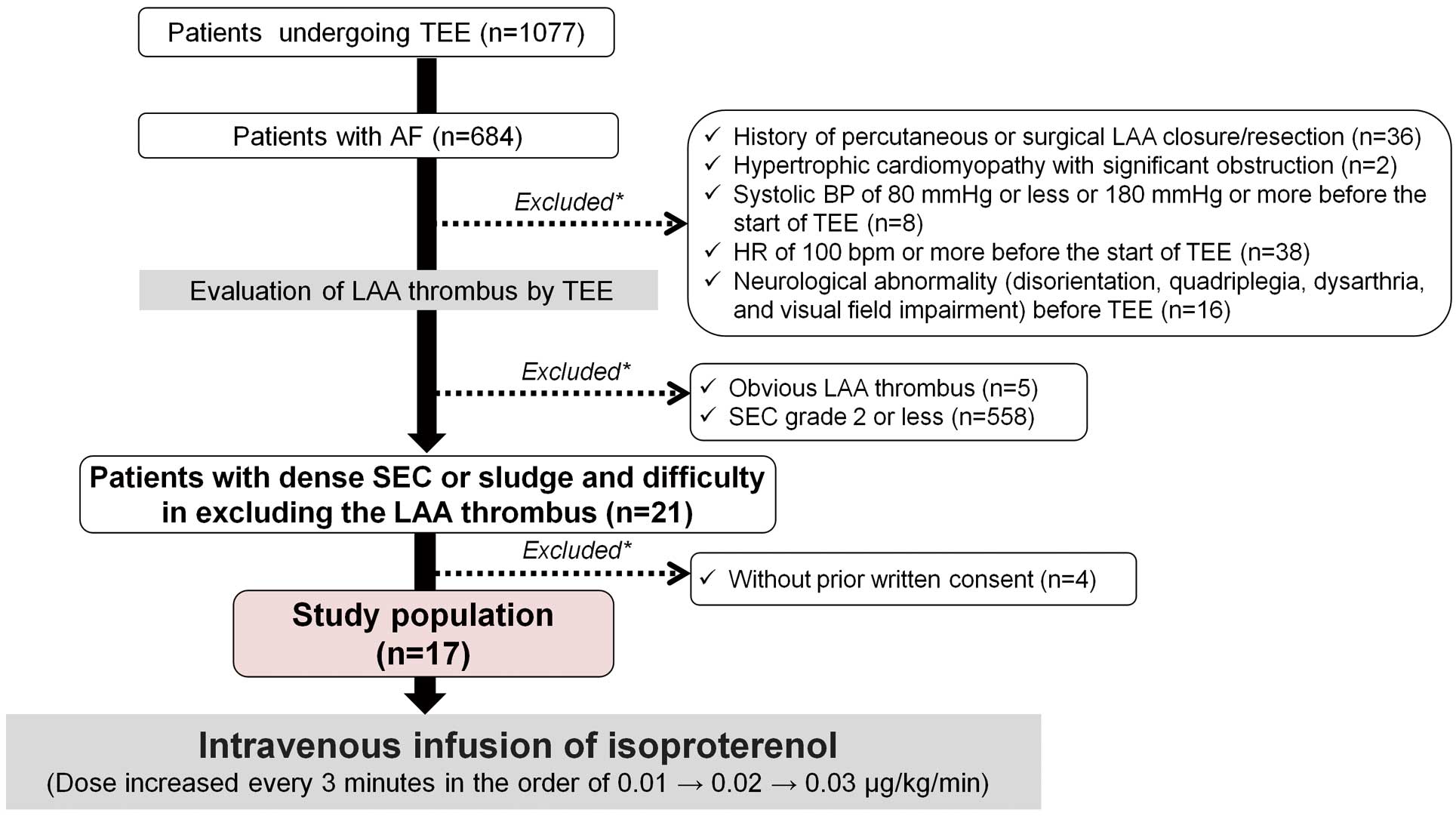
Flowchart showing the study population. Among 1,077 patients undergoing transesophageal echocardiography (TEE) during the study, 17 patients with dense spontaneous echo contrast (SEC) fulfilling the inclusion criteria were enrolled in the present study. Detailed inclusion and exclusion criteria are provided in the Supplementary Methods. AF, atrial fibrillation; BP, blood pressure; HR, heart rate; LAA, left atrial appendage.
TTE was performed using commercially available ultrasound systems (General Electric Medical Systems, Milwaukee, WI, USA) within 3 months prior to TEE. Each echocardiographic measurement was obtained according to the current guidelines.10 The LA volume was measured immediately before mitral valve opening (LA maximum volume) and at mitral valve closure (LA minimum volume) using the biplane method of disks, and was indexed to body surface area. The LA emptying fraction was calculated as [(LA maximum volume − LA minimum volume) / LA maximum volume] × 100. Peak early (E) transmitral flow velocity was measured using pulsed wave Doppler in the apical view. Early peak diastolic velocity (E′) was measured using tissue Doppler imaging at the mitral annular septal and lateral corners. The mean E/E′ ratio was calculated. For 2-dimensional speckle tracking analysis of the LV and LA, we analyzed non-foreshortened apical views using dedicated applications, namely automated functional imaging of the LV and LA (EchoPAC 204; GE Vingmed Ultrasound).10,11 After identifying the endocardial border in each view, the software automatically identified the region of interest and tracked the motion of the speckles in subsequent frames. Consequently, values of LV global longitudinal systolic strain and LA global longitudinal reservoir strain were calculated. Each measurement was averaged in 5 consecutive beats.
TEETEE was performed using the EPIQ CVx/X8-2t ultrasound system (Philips Medical Systems, Andover, MA, USA). All patients underwent TEE after at least a 6-h fast. A topical anesthetic agent was used along with intravenous sedation with midazolam. TEE images were recorded as cine loops for the subsequent analysis. In the longitudinal view of the LAA visualized in 45°–60°, we measured the emptying blood flow velocity with pulsed Doppler, with the sample volume placed 1 cm below the orifice of the LAA.12 Peak LAA emptying and filling flow velocities within each RR interval were measured (Figure 2). We obtained the LAA wall velocity using tissue Doppler imaging in a similar longitudinal view with the sample volume placed at the proximal third of the medial and lateral side walls of the LAA (Figure 2).13,14 The peak upward and downward LAA wall velocities were recorded within each RR interval. The maximum and minimum LAA areas during one cardiac cycle were measured by tracing a line from the ridge of the left upper pulmonary vein along the entire LAA endocardial border. The LAA emptying fraction was calculated as follows: (maximum LAA area − minimum LAA area) / maximum LAA area × 100.12 The LV ejection fraction (LVEF) was calculated by the biplane method of disks with mid-esophageal 4- and 2-chamber views obtained at 0°–20° and 80°–100°, respectively.15 All patients had AF during TEE; therefore, TEE measurements were averaged in 5 consecutive beats.
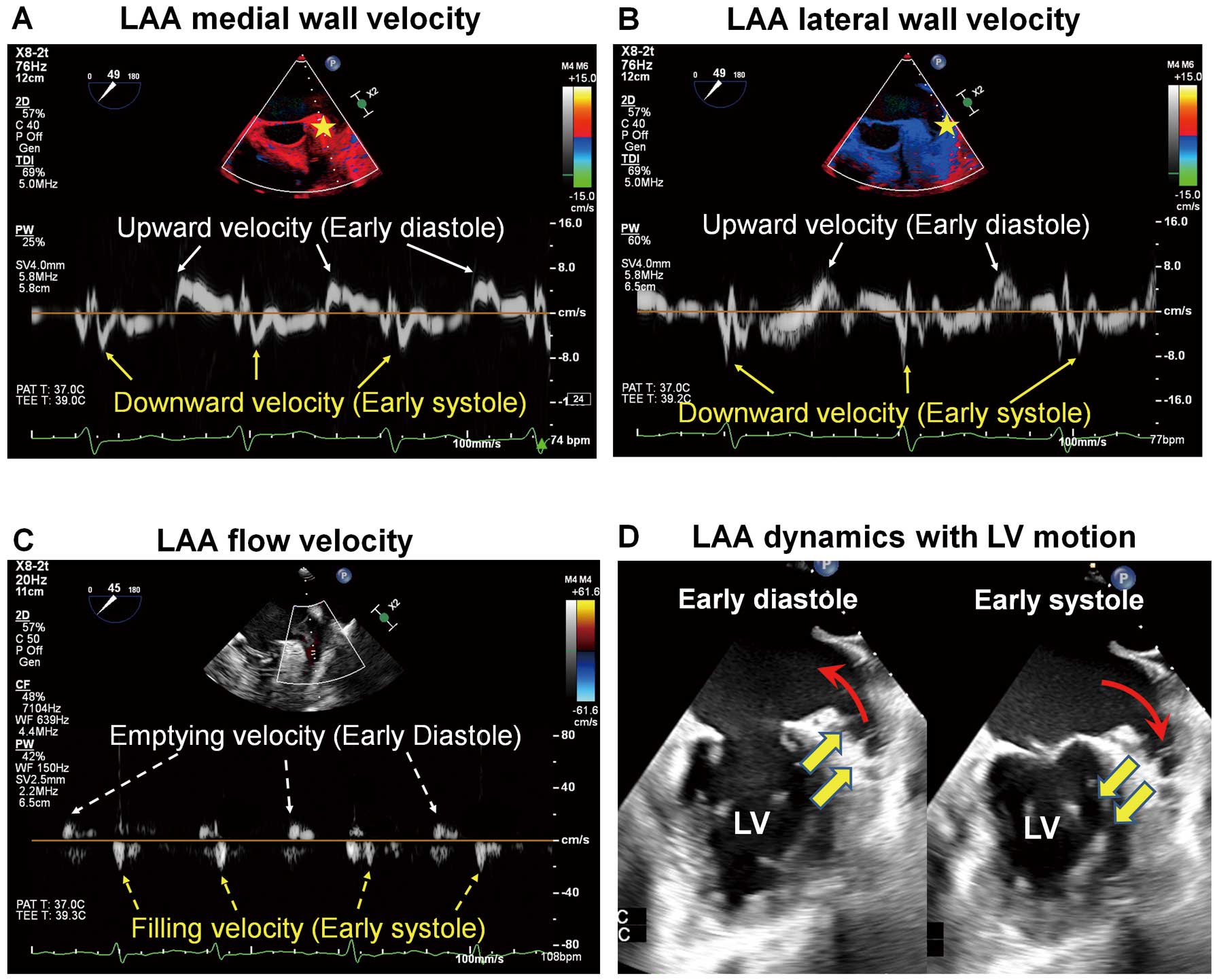
Measurements of left atrial appendage (LAA) function. (A) Medial and (B) lateral wall velocities of the LAA were measured using tissue Doppler imaging. Stars indicate the position of sample volumes. (C) LAA flow velocity. Peak upward (white arrows) and downward (yellow arrows) LAA wall velocities, LAA emptying flow (white dashed arrows), and LAA filling flow (yellow dashed arrows) within each RR interval were measured. The fibrillatory wave is almost absent, and the early diastolic upward wave and early systolic downward wave are dominant (A–C). (D) A schematic representation of LAA wall dynamics with corresponding left ventricular (LV) basal motion. Upward and downward movement of the LV in early diastole and early systole causes the movement of the LAA wall (yellow bold arrows) and generates LAA blood flow (red arrows).
SEC was visually graded from 0 to 4 with careful attention to the gain settings adjusted to distinguish the background white noise.3,16,17 The severity of SEC was scored as follows: Grade 0, none (i.e., the absence of echogenicity); Grade 1, mild (minimal echogenicity in the LAA or sparsely distributed in the LA; may be detectable only transiently during the cardiac cycle); Grade 2, mild-moderate (a more dense swirling pattern than the Grade 1 pattern, but with a similar distribution); Grade 3, moderate (a dense swirling pattern in the LAA detectable constantly throughout the cardiac cycle); and Grade 4, severe (intense echodensity and slow swirling patterns in the LAA and LA).2,16,17 Dense SEC is often termed “sludge”.2,3,17 LAA sludge exhibits dynamic, viscous, layered echo-dense findings without a discrete mass. Despite the sludge appearing denser than SEC, the 2 often coexist.3,4 Further, an accurate differentiation is difficult because of the unavailability of ultrasound-enhancing agents in Japan.17 Therefore, the sludge was integrated with SEC Grade 4 and graded on a 5-point scale. The SEC grade, sludge, and LAA thrombus were determined by T.M.-O. (Observer 1) during TEE. After the examination, similar parameters for each patient were independently evaluated by K. Minami (Observer 2), who was blinded to the clinical data, using stored TEE images and off-line software. Multiple cross-sections by biplane mode of LAA images from 0° to 135° were used to comprehensively determine the SEC grade, sludge, and thrombus. Consequently, we calculated the reproducibility and concordance rate between the 2 observers.
LAA thrombi were defined as round, oval, or irregularly shaped masses that were uniformly echo dense within the LAA, distinct from the underlying LAA endocardium, and present in more than one imaging plane.2–4,16 Special care was taken to differentiate the LAA thrombus from pectinate muscles.
ISP InfusionAfter the baseline recording of TEE, Proternol-L (l-isoprenaline hydrochloride; Kowa Co. Ltd, Nagoya, Japan) was infused through the antecubital vein using an infusion pump at gradually increasing doses of 0.01, 0.02, and 0.03 μg/kg/min at 3-min intervals. ISP infusion was terminated when the HR increased by 20% from baseline, after a dose increase to 0.03 μg/kg/min for 3 min, or when the LAA interior could be distinctly visualized. We reassessed the SEC grade, the presence of thrombus, and quantitative parameters within 1 min of ISP termination; the TEE was completed. The dose and duration of the ISP injection were based on previous studies on safety and efficacy.18–20 The observation period was set as the time from the beginning of ISP infusion to 30 min after its termination based on its half-life (2.5–5 min).21 The electrocardiogram was continuously monitored during the observation and was recorded in case of arrhythmia, except AF. Blood pressure and HR were recorded prior to TEE and measured every minute during and up to 5 min after the discontinuation of ISP administration and every 5 min during the observation thereafter. The investigators assessed for impaired consciousness, quadriplegia, dysarthria, and visual field disturbances at the end of the observation period.
Sample Size CalculationSample size was based on the following rationale, with change in the context of SEC grade before and after ISP infusion as the primary endpoint. SEC comprises 5 grades ranging from 0 to 4 (including sludge), and the enrolled patients included those with Grade 3 or 4 SEC. A previous study showed that the mean change in SEC grade following ISP infusion was −2.1;18 however, we assumed, more conservatively, that the changes in SEC grade after ISP infusion would be −3, −2, −1, 0, and +1 at a rate of 20%, 50%, 20%, and 10%, respectively. If the study enrolled 15 patients, it would have a power >90% based on the Wilcoxon signed-rank test, with a significance level of α=0.05. Considering the dropout rate, we set the sample size as 20. However, 17 patients were enrolled in this study, and there were no dropouts after ISP infusion. Therefore, we analyzed a total of 17 patients.
Statistical AnalysesContinuous variables are presented as the median with interquartile range (IQR). Categorical variables are presented as numbers and percentages. The Wilcoxon signed-rank test was used to compare SEC grades and other TEE parameters before and after ISP infusion. Interobserver agreement in the differentiating grade of SEC was determined using the concordance rate and the κ coefficient. We used a linear mixed-effects model with unstructured covariance for random effects to evaluate repeated measurements of SBP and HR. Statistical significance was set at P<0.05. All statistical analyses were performed using SPSS (version 28.0; SPSS Inc., Chicago, IL, USA).
The Table summarizes the general characteristics of the study participants. Of the 17 participants, 13 (76.5%) were men, with a median age of 77 years. More than half the patients had a history of stroke or thromboembolic episodes under appropriate anticoagulation, and their CHADS2 and CHA2DS2-VASc scores were high. Regarding the TTE parameters, we observed LV systolic dysfunction, a high E/E′ ratio reflecting LV diastolic dysfunction, and severe dilatation of the LA. Moreover, LA reservoir strain and LA emptying fraction, suggestive of progressed degeneration of the LA, were also observed.
| Age (years) | 77.0 [72.5, 80.0] |
| Male sex | 13 (76.5) |
| Body surface area (m2) | 1.64 [1.49, 1.77] |
| CHADS2 score | 4.0 [2.0, 5.0] |
| CHA2DS2-VASc score | 5.0 [4.0, 6.5] |
| Recent decompensated heart failure | 6 (35.3) |
| Hypertrophic cardiomyopathy (non-obstructive) | 3 (17.6) |
| Moderate to severe systolic LV dysfunction (LVEF ≤40%) | 6 (35.3) |
| Hypertension | 11 (64.7) |
| Diabetes | 7 (41.2) |
| History of stroke or TIA or thromboembolism | 10 (58.8) |
| Vascular disease | 4 (23.5) |
| Laboratory data | |
| B-type natriuretic peptide (pg/mL) | 267.0 [125.8, 689.5] |
| eGFR (mL/min/1.73 m2) | 43.0 [28.8, 66.1] |
| PT-INR | 1.77 [1.22, 2.29] |
| D-dimer (μg/mL) | 0.7 [0.6, 1.6] |
| AF pattern | |
| Non-valvular AF | 16 (94.1) |
| Paroxysmal/persistent/long-standing persistent | 1 (5.9)/5 (29.4)/11 (64.7) |
| Duration of non-paroxysmal AF, years (n=16) | 4.0 [0.6, 9.5] |
| Oral anticoagulant therapy | |
| Dabigatran/rivaroxaban/apixaban/edoxaban/warfarin | 3 (17.6)/1 (5.9)/6 (35.3)/1 (5.9)/6 (35.3) |
| Transthoracic echocardiography | |
| LV end-diastolic volume (mL/m2) | 61.4 [47.9, 95.6] |
| LV end-systolic volume (mL/m2) | 34.1 [18.8, 48.4] |
| LVEF (%) | 51.0 [38.0, 63.5] |
| LV mass index (g/m2) | 112.0 [85.0, 133.0] |
| LV global longitudinal strain (%) | −11.3 [−13.5, −8.6] |
| LA diameter (mm) | 52.0 [42.5, 57.5] |
| LA maximum volume index (mL/m2) | 59.0 [41.2, 87.9] |
| LA minimum volume index (mL/m2) | 49.1 [31.5, 73.1] |
| LA emptying fraction (%) | 15.0 [12.0, 30.5] |
| LA reservoir strain (%) | 8.0 [5.0, 10.5] |
| Mitral inflow E wave (cm/s) | 89.0 [78.0, 118.0] |
| E/E′ ratio | 12.5 [9.6, 19.4] |
Results are presented as the median [interquartile range] or as n (%). AF, atrial fibrillation; eGFR, estimated glomerular filtration rate; LA, left atrial; LV, left ventricular; LVEF, left ventricular ejection fraction; PT-INR, international normalized ratio of prothrombin time.
The peak injection doses for ISP were 0.01, 0.02, and 0.03 μg/kg/min in 3, 4, and 10 patients, respectively. Figure 3 shows the effects of ISP infusion on LAA and LV function. Compared with baseline, ISP infusion significantly increased the LAA emptying fraction along with the upward and downward wall motion velocities of the LAA medial and lateral sides. Furthermore, it improved LVEF. Thus, both LAA emptying and filling velocities were significantly increased.

Effects of isoproterenol (ISP) on the functions of the left atrial appendage (LAA) and left ventricle (LV). Changes in (A) LAA flow velocity, (B) LAA emptying fraction, (C) LAA medial wall velocity, (D) LAA lateral wall velocity, and (E) LV ejection fraction at baseline and after ISP infusion. Open circles indicate the 15 patients in whom ISP infusion improved the spontaneous echo contrast (SEC) and closed circles indicate the 2 patients with persistent dense SEC after ISP administration. In box plots, the median is indicated by the horizontal line and the mean is indicated by the “X”. Numbers near the boxes are median values. P-values shown were determined using the Wilcoxon signed-rank test.
Figure 4 shows changes in HR and blood pressure caused by ISP infusion. HR increased and blood pressure decreased significantly during ISP infusion. The mean HR increased from 71 beats/min at baseline to 97 beats/min at peak. Mean SBP decreased from 107 to 96 mmHg (from baseline to peak), and mean diastolic blood pressure decreased from 61 to 51 mmHg (from baseline to peak).

Hemodynamic effects of isoproterenol (ISP). Bar shows changes in systolic and diastolic blood pressure before, during, and up to 10 min after the infusion of ISP. The line shows changes in heart rate. Bars and symbols represent the estimated marginal means of the measurements at each time point. Error bars represent 95% confidential intervals. P-values were determined using a linear mixed-effects model.
The percentages of SEC grades were independently assessed by 2 observers. There was almost perfect agreement in the findings between the 2 observers (κ=0.88, P<0.001). Figure 5 shows the percentages of SEC grades evaluated by the Observer 1. All patients had an SEC Grade 4 or sludge at baseline. However, after ISP infusion, the SEC grade decreased to ≤2 in 15 (88%) patients, and no LAA thrombus was identified. ISP administration significantly reduced the SEC grade (median) from 4 (baseline) to 1 (P<0.001).

Changes in spontaneous echo contrast (SEC) grades at baseline and during isoproterenol (ISP) infusion. SEC grades assessed by Observer 1 at baseline and after ISP infusion at peak dose are shown. Boxes represent the proportion of each SEC grade. P-values were determined using the Wilcoxon signed-rank test. Thrombus could be excluded in 15 patients in whom ISP reduced the SEC grade to ≤2. However, the thrombus could not be excluded in 2 patients, in whom SEC Grade 4 or sludge persisted after ISP infusion.
Figure 6 and Supplementary Movie 1 shows a case of persistent AF and dilated cardiomyopathy with depressed LVEF. ISP injection reduced the SEC Grade 4 or sludge to Grade 1 and confirmed the absence of a thrombus.
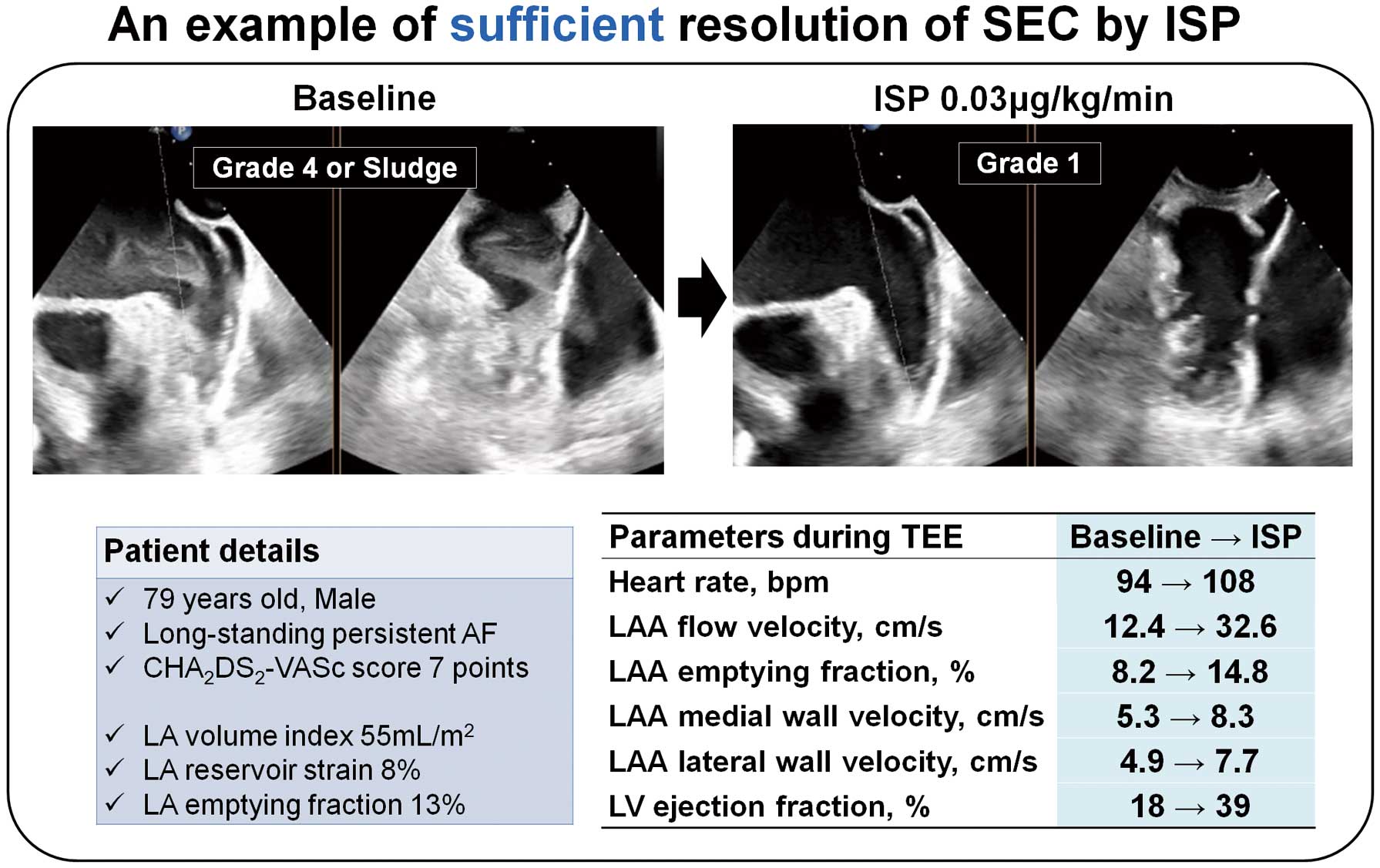
Example of sufficient resolution of spontaneous echo contrast (SEC) following isoproterenol (ISP) infusion. A 79-year-old male patient with dilated cardiomyopathy and reduced left ventricular ejection fraction (LVEF) of 18% was infused with ISP (0.03 μg/kg/min). ISP improved the LVEF and left atrial appendage (LAA) function, and reduced SEC Grade 4 or sludge to Grade 1. AF, atrial fibrillation; LA, left atrium; LV, left ventricle; TEE, transesophageal echocardiography.
However, TEE findings did not show any improvement from SEC Grade 4 or sludge after ISP administration in 2 (12%) patients. LAA thrombus could not be excluded because the LAA interior was not observed distinctly throughout the cardiac cycle. In both cases, LVEF was well preserved. However, both these patients exhibited severe LA enlargement and dysfunction. Moreover, LAA function did not improve sufficiently after ISP infusion. Figure 7 and Supplementary Movie 2 shows one such case.
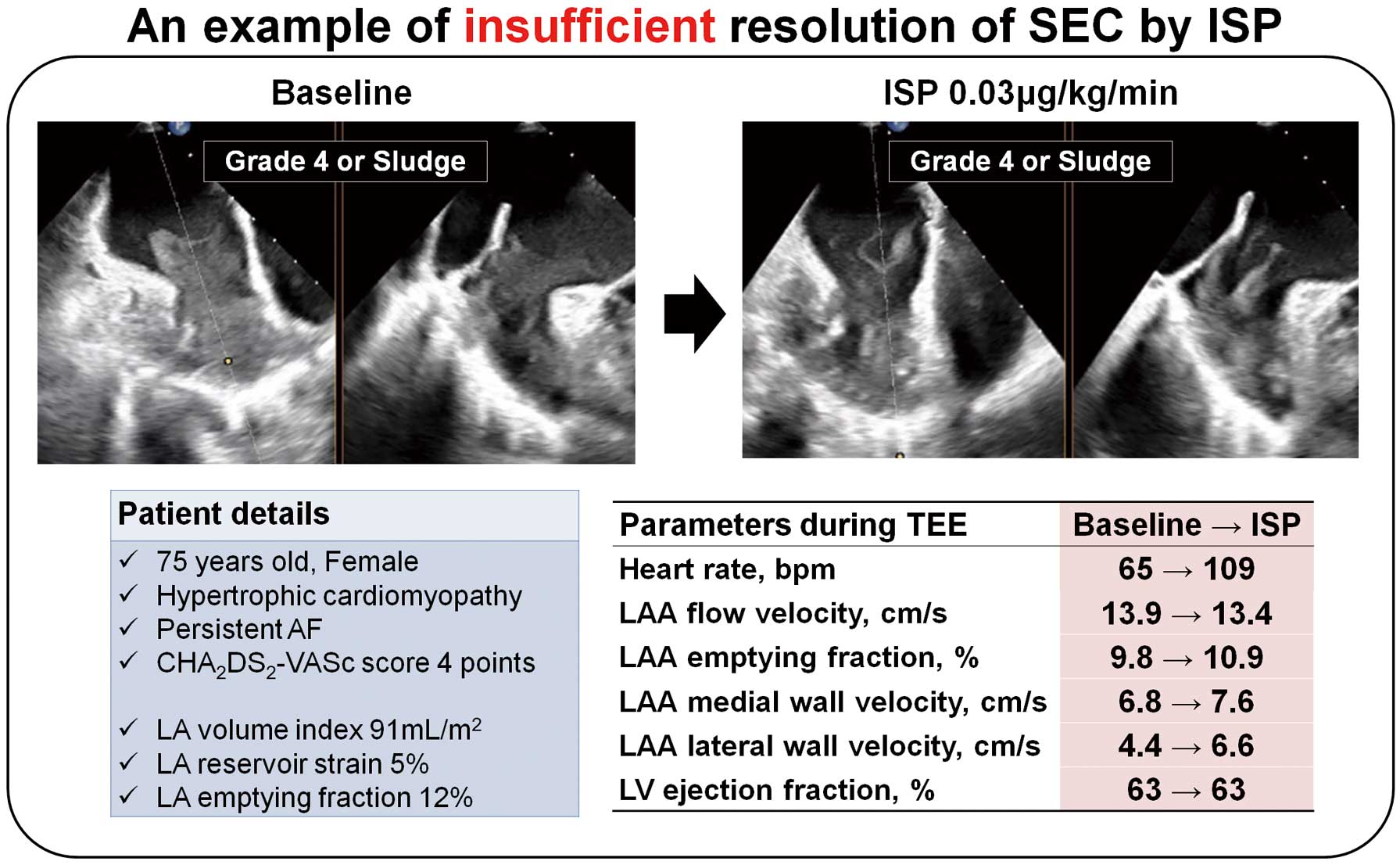
Example of insufficient resolution of spontaneous echo contrast (SEC) following isoproterenol (ISP) infusion. A 75-year-old female patient with hypertrophic cardiomyopathy and preserved left ventricular ejection fraction (LVEF) of 63% but impaired left atrial (LA) and left atrial appendage (LAA) functions was infused with ISP (0.03 μg/kg/min), which did not change the LVEF and resulted in poor improvement of LAA function. Moreover, SEC Grade 4 or sludge persisted. AF, atrial fibrillation; LV, left ventricle; TEE, transesophageal echocardiography.
We observed no major adverse events related to the study. During ISP infusion, single ventricular premature contractions <5 beats/min occurred in 3 patients, and up to 4 consecutive non-sustained ventricular beats occurred in 1 patient; however, they did not cause hemodynamic changes. In the evaluation at the end of the observation period after ISP infusion, there were no novel neurological abnormality, such as impaired consciousness, quadriplegia, dysarthria, and visual field disturbances. ISP administration caused a transient increase in HR and decreased blood pressure, which was restored to baseline within the 30-min observation period. Further, no life-threatening complications or side effects requiring specific treatment occurred in any patient.
Of the 15 patients in whom the LAA thrombus could be excluded by ISP infusion, 11 underwent catheter ablation of AF and 4 underwent percutaneous LAA closure within 24 h. No patient experienced thromboembolic complications related to the procedures. The scheduled procedures were postponed in 2 patients in whom the LAA thrombus could not be excluded because of persistent dense SEC after ISP infusion.
In this study, low-dose ISP infusion significantly improved not only LAA function, but also LV function in most patients with AF and dense SEC in the LAA, excluding the possibility of a thrombus. Low-dose ISP infusion significantly increased the HR and decreased blood pressure. Nonetheless, no side effects requiring specific treatment were observed. Moreover, 2 patients in whom SEC was not sufficiently reduced by low-dose ISP exhibited an increase in HR with ISP, along with poor improvement in cardiac function.
Possible Mechanisms of SEC Reduction via Positive Inotropic Effects of ISPMost patients with dense SEC had severe LA structural remodeling and significant impairment of LA contractile and reservoir functions, which could be considered the pathogenesis of atrial cardiomyopathy caused by persistent AF.22 Furthermore, LAA function, represented by LAA emptying fraction and wall velocity, was markedly reduced and suggested possible myocyte loss and LAA fibrosis in the cohort. However, in approximately 90% of these cases, low-dose ISP was sufficiently effective in reducing the SEC grade by improving LAA wall motion and increasing LAA blood flow velocity.
Because LA myocardial fibers in patients with chronic AF require 10-fold greater ISP concentrations than those in patients with sinus rhythm to achieve equivalent positive inotropic effects,23 the degree of LAA degeneration may cause differences in response to ISP administration. This study included consecutive cases without arbitrary selection, thereby suggesting the potential utility of low-dose ISP administration in most AF patients with dense SEC. In addition, ISP improved the SEC of the LAA by improving LV contraction because the LAA is located adjacent to the lateral basal wall of the LV.14 Generally, the LAA wall and LAA blood flow in AF exhibit rapid fibrillary motion by intrinsic contractions.13 However, with the progression of LAA degeneration, the fibrillary wave disappeared and the early diastolic upward wave, along with the early systolic downward wave, became dominant (Figure 2). The upward and downward waves of the LAA wall synchronize completely with early diastolic and systolic motion of the LV and mitral ring.14 Thus, in patients with severely impaired LAA function, ISP may improve LAA contraction from the outside via inotropic effects on the LV.
Possible Mechanisms of SEC Reduction via Positive Chronotropic Effects of ISPDiastasis refers to the pause between the early and late diastolic phases. It is responsible for the quiescent status of blood flow from the atrium to the ventricle.24 Prolonged diastasis caused by bradycardia may cause blood stasis and dense SEC.24 Therefore, positive chronotropic effects of ISP may reduce the SEC grade by increasing the HR and reducing diastasis. However, in the case shown in Figure 7 and Supplementary Movie 2, SEC was not sufficiently reduced, even though ISP significantly increased HR. This finding may indicate that the chronotropic effect of ISP was less important than its inotropic effects for reducing SEC in certain patients.
Clinical Implications and Limitations of Low-Dose ISP InfusionISP doses used in previous reports were boluses of 2–32 μ g or continuous infusions of 1–2 μg/kg/min.7–9 However, relatively lower doses of ISP (0.01–0.03 μg/kg/min) were found to be sufficient to reduce SEC and exclude a thrombus in most patients in the present study. ISP exerts greater chronotropic and peripheral vasodilator effects and weaker inotropic effects compared with other β-adrenergic receptor agonists, such as dobutamine and dopamine. Thus, administration of high-dose ISP results in hypotension.25 Furthermore, sedation for TEE markedly reduces blood pressure, particularly in older patients.26 Because most patients with AF and dense SEC are older patients or those with impaired cardiac function, clinicians are required to maintain the lowest ISP dose to avoid hemodynamic instability during TEE. Our proposed low-dose ISP infusion may serve as a reference for a potentially safe and effective method in echocardiography laboratories. In the present study, 2 patients with severe structural and functional degeneration of the LA and LAA demonstrated residual SEC after low-dose ISP administration. Such patients exhibit a reduced response to β-adrenergic receptor agonists and may require even higher concentrations of ISP or other agents with stronger chronotropic effects than ISP to decrease SEC.8,9,25 However, further investigations are required to confirm these hypotheses.
Study LimitationsFirst, because this was a small single-arm study with a limited number of patients, no definite conclusions can be drawn regarding the safety and efficacy of ISP injections. This study only provides preliminary data on ISP dose and methodology. A randomized control trial with a larger study population may be required to confirm our results. Second, although we confirmed the absence of new abnormal neurological findings after ISP injection, we did not perform brain magnetic resonance imaging to exclude cardiogenic embolism. Thus, the safety of low-dose ISP infusion was only partially confirmed in this study with respect to hemodynamics. Safety confirmation regarding the risk of embolism should be assessed by magnetic resonance imaging at the time of inclusion in the study and after ISP infusion. Moreover, the findings should be ultimately confirmed by an experienced neurologist unaware of the TEE findings. Further investigations are warranted in this regard.
In most patients with AF and dense SEC in the LAA, low-dose ISP infusion significantly improved LAA and LV functions and sufficiently reduced SEC to exclude an LAA thrombus. Despite the potential safety and efficacy of low-dose ISP administration, further studies are required to confirm our results.
The authors are grateful to R.N. Saito for technical assistance.
This study was sponsored by the University of Tsukuba, Grant for Implementation of Advanced Medicine and supported by JSPS KAKENHI (Grant no. 19K17586).
K. Maruo provided statistical analysis advice for projects other than the present study conducted by Kowa Co., Ltd. M.I. is an Associate Editor of Circulation Journal. None of the other authors have any conflicts to interest relevant to the contents of this paper to disclose.
This study was approved by the Tsukuba University Clinical Research Review Board (TCRB20-20).
The deidentified participant data will not be shared.
Supplementary Movie 1. An example of sufficient resolution of SEC by ISP infusion. SEC, spontaneous echo contrast; ISP, isoproterenol.
Supplementary Movie 2. An example of insufficient resolution of SEC by ISP infusion. SEC, spontaneous echo contrast; ISP, isoproterenol.
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-23-0271