Abstract
Background: We have reported that a prehospital 12-lead electrocardiography system (P-ECG) contributed to transport of suspected acute coronary syndrome (ACS) patients to appropriate institutes and in this study, we compared its usefulness between urban and rural areas, and between weekday daytime and weekday nighttime/holiday.
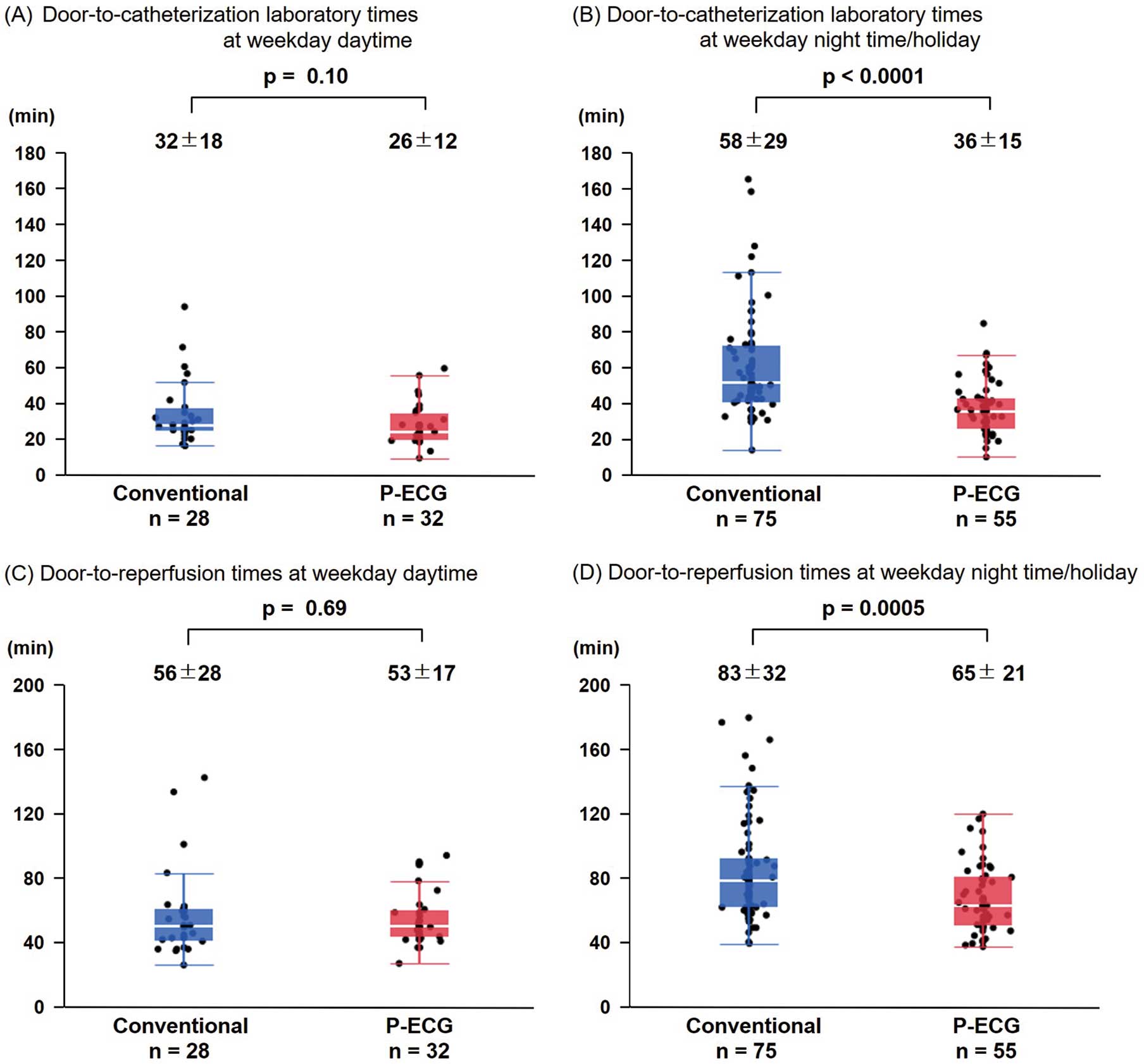
Methods and Results: Consecutive STEMI patients who underwent successful primary percutaneous coronary intervention after using P-ECG were assigned to the P-ECG group (n=123; 29 female, 70±13 years), and comparable STEMI patients without using P-ECG were assigned to the conventional group (n=117; 33 females, mean age 70±13 years). There was no significant difference in door-to-reperfusion times between the rural and urban cases (70±32 vs. 69±29 min, P=0.73). Door-to-reperfusion times in the urban P-ECG group were shorter than those in the urban conventional group for weekday nighttime/holiday (65±21 vs. 83±32 min, P=0.0005). However, there was no significance different between groups for weekday daytime. First medical contact to reperfusion time (90±22 vs. 105±37 min, P=0.0091) in the urban P-ECG group were significantly shorter than in the urban conventional groups for weekday nighttime/holiday, but were not significantly different between the groups for weekday daytime.
Conclusions: P-ECG is useful even in urban areas, especially for patients who develop STEMI during weekday nighttime or while on a holiday.
Many reports have demonstrated that the implementation of a prehospital 12-lead electrocardiography system (P-ECG) for diagnosis of ST-segment elevation myocardial infarction (STEMI) reduces the time from first medical contact to reperfusion and from arrival at the hospital to reperfusion.1–4 We have also reported that the P-ECG shortened door-to-balloon time (DTBT) in STEMI patients in Oita,4 and subsequently that it helped to transport suspected acute coronary syndrome (ACS) patients to optimal institutes.5
P-ECG bestows a significant advantage when there is a longer transport time for STEMI patients, because cardiologists have time to prepare for percutaneous coronary intervention (PCI). Prehospital ECG diagnosis and direct transport to primary PCI facility enables patients living far from PCI institutions to achieve a system delay comparable with that observed in patients near PCI institutes and might be associated with a lower mortality rate.6 However, in urban areas, the transport time is usually shorter than that in the rural areas, so P-ECG may contribute less to DTBT reduction due to the shorter time between ECG transmission and arrival at hospital in urban areas.
In addition, in a previous study, patients treated with primary PCI during weekday nights or holiday times had longer DTBT, which was associated with higher mortality rates.7
Because P-ECG has been integrated in Oita Prefecture, we compared analyzed its usefulness between urban and rural areas, and between weekday daytime and weekday night time/holidays.
Methods
P-ECG System in Oita
On April 17, 2017, the P-ECG (Cloud Cardiology®, Labtech Co., Debrecen, Hungary) system was started in 18 hospitals and 10 ambulances of 10 respective fire departments in Oita Prefecture, and has since been extended to 24 hospitals and 14 respective fire departments in the prefecture. As of July 2022, 41 of a total of 79 ambulances are equipped with ECGs; 19 PCI institutions have 24-h PCI availability, but the 5 regional core hospitals do not.
Emergency medical services (EMS) record a 12-lead ECG in patients with suspected ACS and transmit to a secure cloud server (SCUNA®, Mehergen, Fukuoka, Japan), using the network of the existing image transmission system. The ECG in the cloud server can be browsed simultaneously from personal computers, smartphones, and tablets from anywhere after access key authentication. The EMS are educated that symptoms of ACS are frequently atypical, and non-localized, including upper extremities and jaw, and might be accompanied by non-specific symptoms, including dyspnea, cold sweats, discomfort, and nausea. Immediately after a cardiologist participating in the P-ECG receives a request for an ECG reading from the EMS and diagnoses of suspected ACS, a decision is made to perform emergency cardiac catheterization examination before the patient arrival at hospital.
Patient Selection and Grouping
During the 64 months of the study period (April 2017 to July 2022), the decision to transmit a P-ECG for suspected ACS was left to the judgment of the EMS team on site. The total number of P-ECG transports was 2,340, of which 123 patients (29 women, mean age 70±13 years) with STEMI were transported to 11 participating hospitals by ambulances equipped with P-ECG and underwent successful primary PCI (P-ECG group).
A total of 117 patients with STEMI were transported directly by a conventional ambulance without P-ECG (n=94) or walked in (n=23) to 5 participating hospitals in Oita City and Oita University Hospital within the same time period and were assigned to the conventional group (33 females, mean age 70±13 years). Door-to-catheterization time (50±20 vs. 52±31 min, P=0.76) and door-to-reperfusion time (73±25 vs. 78±35 min, P=0.53) were not significantly different between walk-in and transport cases in the conventional group.
This investigation was conducted according to the principles expressed in the Declaration of Helsinki. The study protocol was approved by the Oita University Research Ethics Committee (approval no. 1262).
Urban cases were defined as patients transported within the same city as the hospital where PCI was performed, and rural cases were defined as patients transported from a different area to the hospital where PCI was performed. All patients were grouped as rural conventional, rural P-ECG, urban conventional, and urban P-ECG groups according to the definitions described above.
Holidays were defined as national holidays and weekends. Nighttime was defined as arrival at the hospital between 6:00 p.m. and 8:00 a.m.7
Definitions of Time Intervals
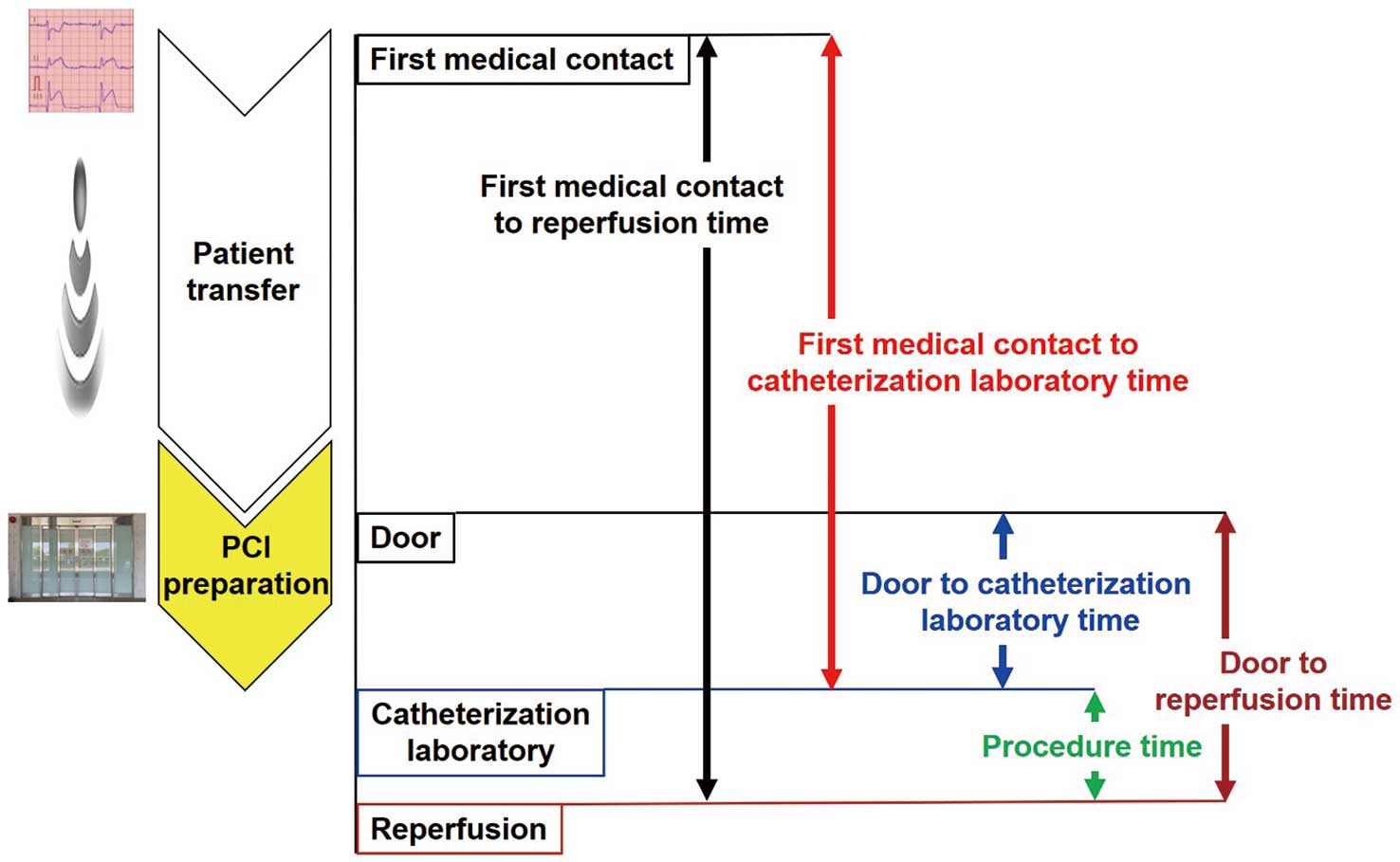
Patient transfer time was defined as the interval from the time the EMS departed the scene to the door time (i.e., the arrival time at the emergency department where emergency catheterization was performed). Procedure time was defined as the interval from the arrival time at the emergency catheterization laboratory to reperfusion. The door-to-reperfusion time was defined as the interval from the door time to the reperfusion. Door-to-catheterization laboratory time (DLT) was defined as the interval from the door time to the arrival time at the emergency catheterization laboratory. First medical contact to reperfusion time was defined as the interval from the time of EMS arrival on the scene to the reperfusion. First medical contact to catheterization laboratory time was defined as the interval from the time of EMS arrival on the scene to the arrival time at the emergency catheterization laboratory (Figure 1).
Statistical Analysis
Data are presented as the mean±SD. A chi-square test was used for categorical variables and analysis of variance (ANOVA) was used for continuous variables. The differences between groups were analyzed by Student’s t-test. To compare differences among the 4 groups of rural conventional, rural P-ECG, urban conventional, and urban P-ECG groups or the 4 groups of night time/holiday in the conventional group, weekday daytime in the conventional group, night time/holiday in the P-ECG group, and weekday daytime in the P-ECG group, one-way ANOVA was used, followed by Tukey’s HSD to account for multiple comparisons. The ability of defining factors to predict the extension of DLT was assessed by the area under the curve (AUC) generated from receiver-operating characteristics (ROC) analysis. P<0.05 was considered significant. All computations were performed with JMP (version 13.2.0; SAS, Cary, NC, USA) running under Windows 10 (Microsoft, Redmond, WA, USA).
Results
Baseline Characteristics of Patients
The baseline characteristics of the rural conventional, rural P-ECG, urban conventional, and urban P-ECG groups are presented in the Table. No significant difference was observed with respect to age, sex, culprit vessel, number of diseased vessels, Killip class, maximum creatine kinase (max CK), left ventricular ejection fraction (LVEF) or in-hospital deaths.
Table. Baseline Characteristics of the 4 Groups of Patients
| |
Rural conventional
(n=14) |
Rural P-ECG
(n=36) |
Urban conventional
(n=103) |
Urban P-ECG
(n=87) |
P value |
| Age (years) |
72±12 |
73±11 |
70±13 |
69±14 |
0.65 |
| Female (%) |
2 (14) |
9 (25) |
31 (30) |
20 (23) |
0.49 |
| Culprit vessel |
|
|
|
|
0.77 |
| LMT (%) |
1 (7) |
1 (3) |
1 (1) |
4 (5) |
|
| LAD (%) |
8 (57) |
16 (44) |
57 (55) |
44 (51) |
|
| LCX (%) |
1 (7) |
5 (14) |
7 (7) |
7 (8) |
|
| RCA (%) |
4 (29) |
14 (39) |
38 (37) |
32 (37) |
|
| No. of diseased vessels |
|
|
|
|
0.58 |
| 1 (%) |
7 (50) |
21 (58) |
51 (50) |
151 (59) |
|
| 2 (%) |
3 (21) |
11 (31) |
35 (34) |
22 (25) |
|
| 3 (%) |
3 (21) |
3 (8) |
16 (16) |
10 (11) |
|
| LM |
1 (7) |
1 (3) |
1 (1) |
4 (5) |
|
| Killip class (%) |
|
|
|
|
0.80 |
| 1 |
9 (64) |
27 (75) |
80 (78) |
65 (75) |
|
| 2 |
1 (7) |
5 (14) |
7 (7) |
5 (6) |
|
| 3 |
1 (7) |
2 (6) |
6 (6) |
5 (6) |
|
| 4 |
3 (21) |
2 (6) |
10 (10) |
12 (14) |
|
| Max CK (U/L) |
1,909±1,415 |
2,955±2,386 |
2,542±2,142 |
3,232±3,138 |
0.15 |
| EF (%) |
52±10 (n=14) |
54±10 (n=33) |
55±10 (n=101) |
51±10 (n=70) |
0.15 |
| Mortality (%) |
7.1 |
5.6 |
3.9 |
3.5 |
0.90 |
CK, creatine kinase; EF, ejection fraction; LAD, left anterior descending; LCX, left circumflex artery; LMT, left main trunk; P-ECG, prehospital 12-lead electrocardiography system; RCA, right coronary artery.
When all eligible patients were analyzed, max CK was significantly higher in all patients who had P-ECG performed than in those who did not (3,150±2,930 vs. 2,466±2,075 U/L, P=0.039), despite the shorter time factor.
A total of 3 patients in the rural P-ECG group, 2 in the urban conventional group, and 17 in the urban P-ECG group had indeterminate LVEF.
Rate of P-ECG Procedures
We analyzed the 24-month period from September 2019 to August 2021, when a detailed survey was available for Oita City, which accounts for 43% of the population of Oita Prefecture and has the highest number of transports. The number of P-ECG transports among 200 patients, excluding 151 transfers and 34 cases of cardiopulmonary arrest from the 385 total transported patients with acute myocardial infarction (AMI), was 79, and the P-ECG procedure rate for transported patients with AMI was 40%.
Procedure Times Between P-ECG and Conventional Groups
Procedure time in the P-ECG group was significantly longer than in the conventional group (30±15 vs. 25±16 min, P=0.016).
Time Intervals for Rural and Urban Cases
Patient transfer times in rural cases were significantly longer than in urban cases (36±15 vs. 9±6 min, P<0.0001). However, there was no significant difference in door-to-reperfusion times (70±32 vs. 69±29 min, P=0.73) or DTL times (39±23 vs. 42±25 min, P=0.45) between rural and urban cases.
Time Intervals Among the 4 Groups
EMS stayed on the scene 11±8 min in rural conventional, 14±6 min in the rural P-ECG, 13±7 min in the urban conventional, and 14±6 min in the urban P-ECG group and there were no significant differences among the 4 groups.
Due to lack of data on the time the EMS departed the scene, 2 patients in the rural conventional group, 1 in the rural P-ECG group, and 29 in the urban conventional group (including 23 walk-ins) had indeterminate patient transfer times. Patient transfer times in the rural conventional and the rural P-ECG groups were significantly longer than in the urban conventional and the urban P-ECG groups (Figure 2). The 23 walk-in patients in the urban conventional group were excluded from this analysis. Therefore, 2 patients in the rural conventional group, 1 in the rural P-ECG group, and 6 in the urban conventional group had indeterminate patient transfer times due to unknown onsite departure times.

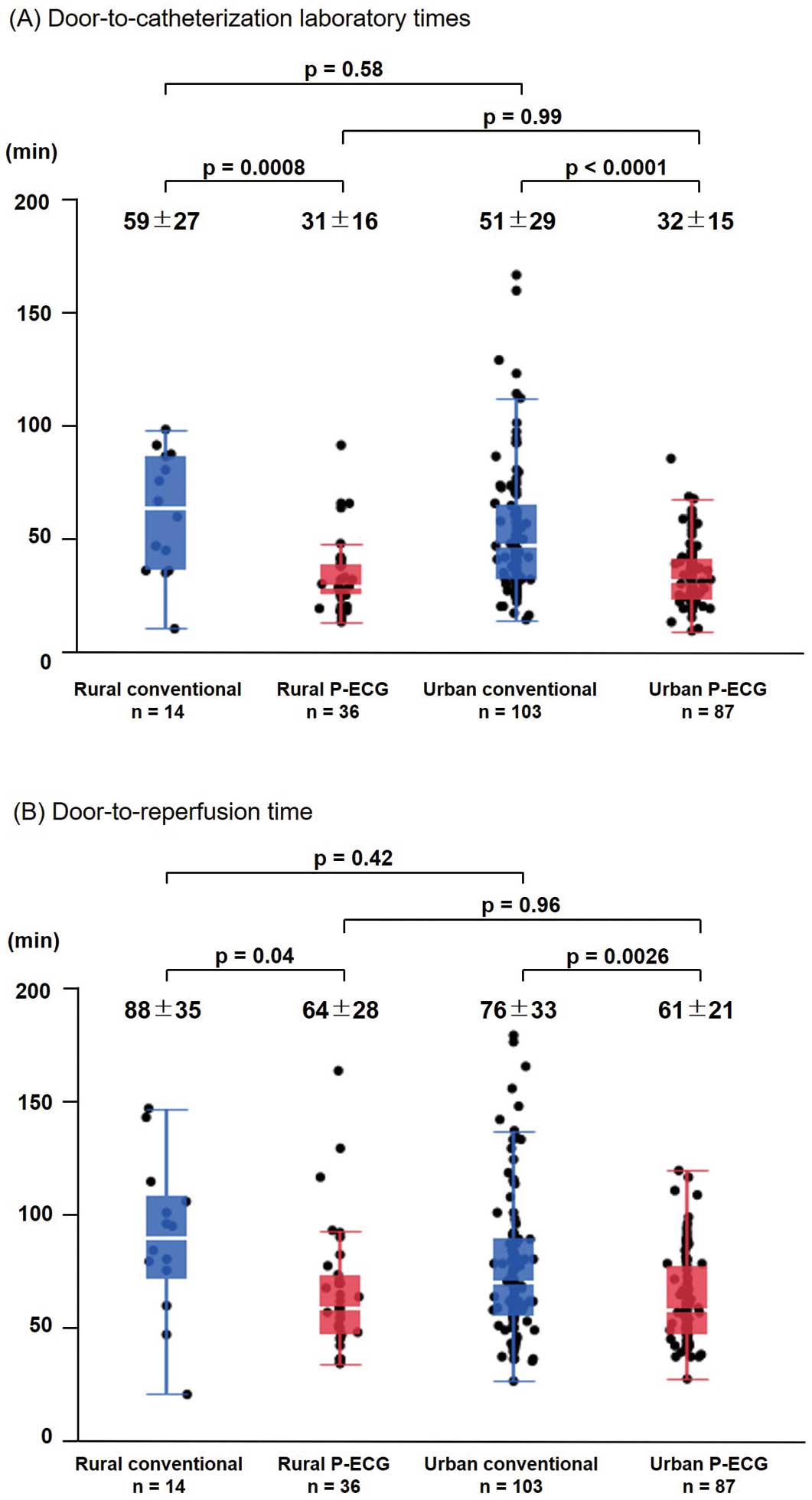
Door-to-reperfusion times in the rural and urban P-ECG groups were significantly longer than in the rural and urban conventional groups (Figure 3A). The DTL times in the rural and urban P-ECG groups were significantly longer than in the rural and urban conventional groups. Door-to-reperfusion times and DTL times did not differ between the rural and urban conventional groups or between the rural and urban P-ECG groups (Figure 3B).
Factors Affecting DTL Time
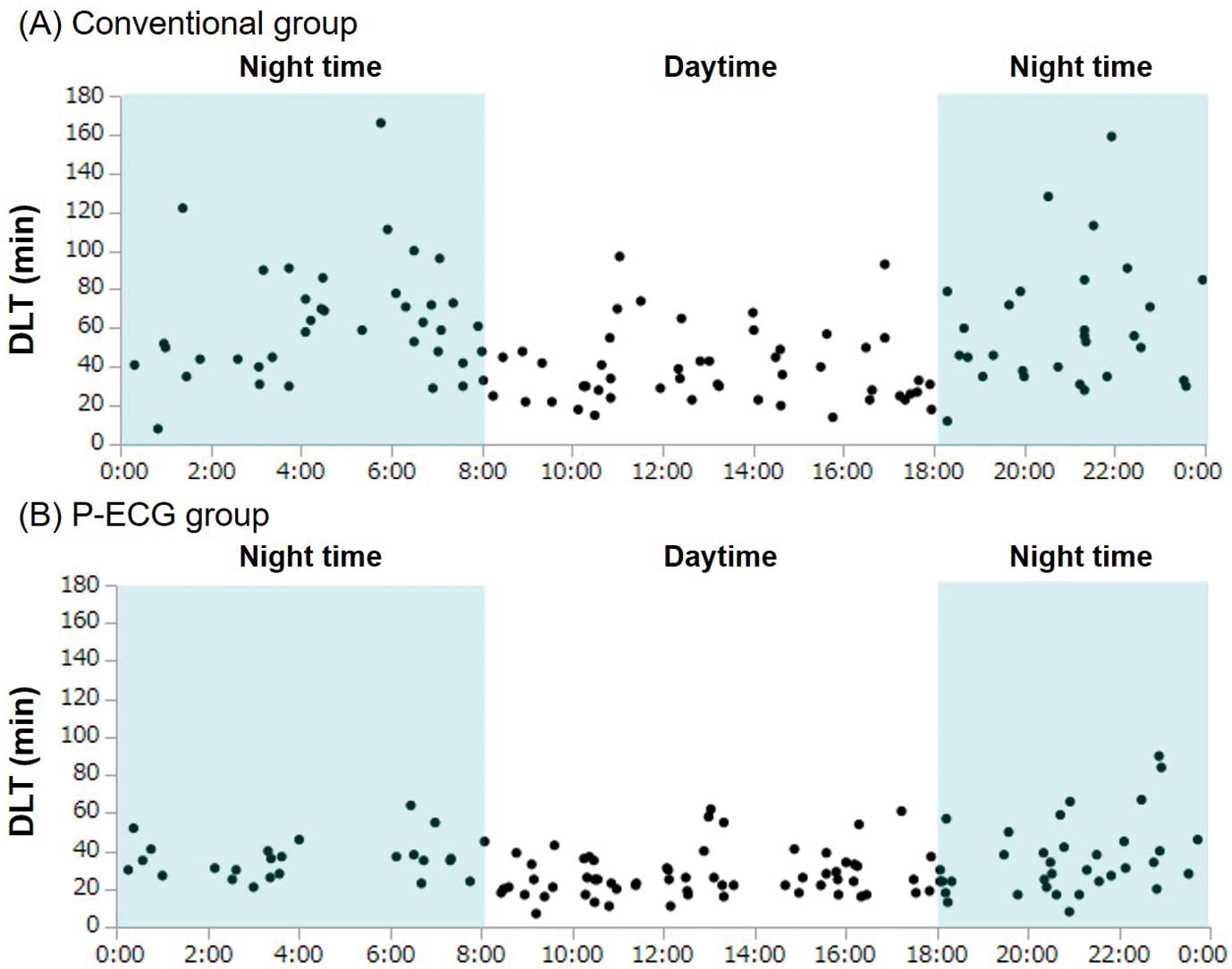
DTL times were longer at night time in many cases of the conventional group (Figure 4A), but less so in the P-ECG group (Figure 4B). According to one-way ANOVA, DTL times in the conventional group in night time/holiday were longer than in weekday daytime (59±29 vs. 35±20 min, P<0.0001). However, for the P-ECG group DTL times at night time/holiday did not differ from weekday daytime (35±16 vs. 25±11 min, P=0.08).
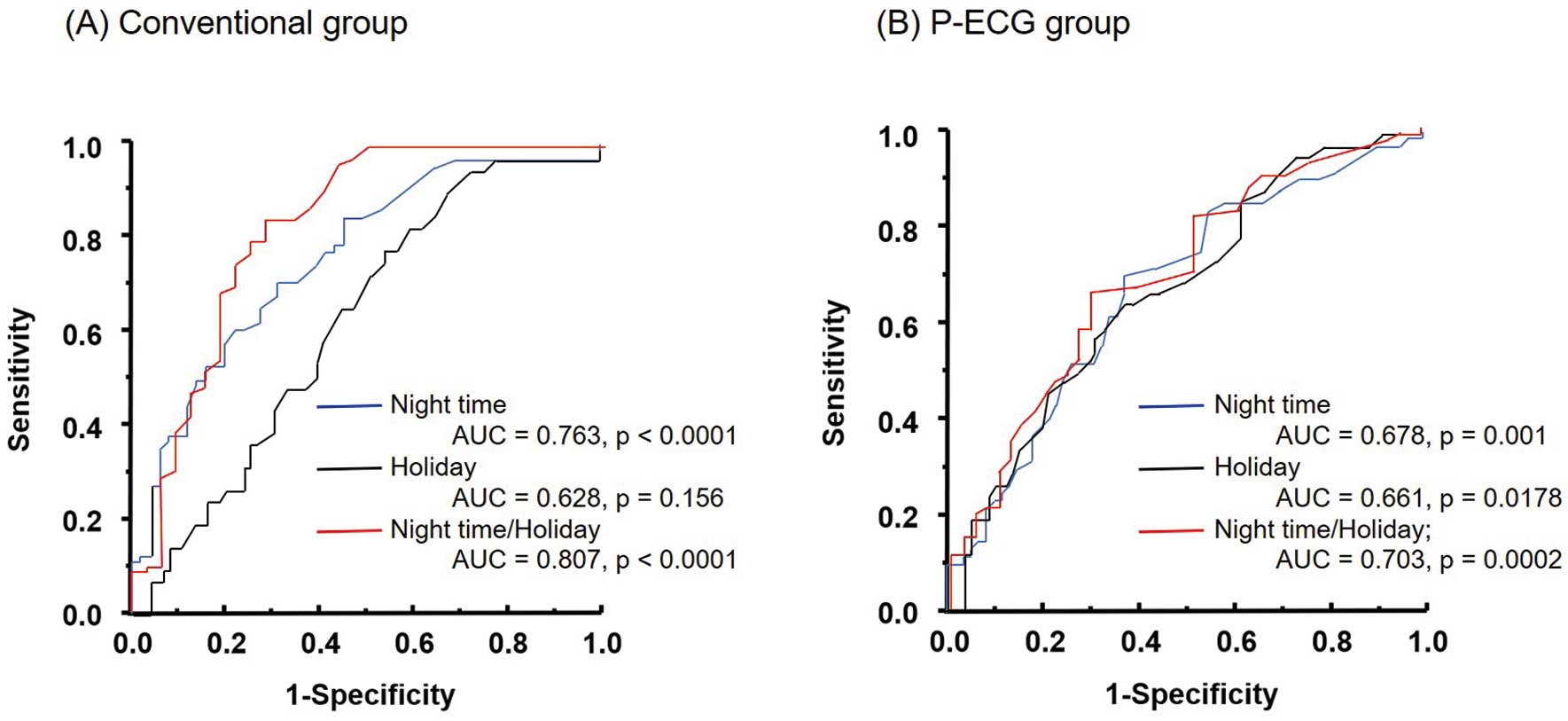
ROC curves for the ability to predict prolongation of DTL times at night time, holidays, and a combination of both in the conventional and P-ECG groups are shown in Figure 5A,B. Night time/holiday had the largest AUC to predict DTL time prolongation in each group.
Time Intervals for Urban Cases in the Conventional and P-ECG Groups
First medical contact to reperfusion time (85±22 vs. 97±38 min, P=0.0098) and first medical contact to catheterization laboratory time (56±17 vs. 72±34 min, P<0.0001) were significantly shorter in the urban P-ECG group than in the urban conventional group.
Door-to-reperfusion and DTL times were significantly shorter in the urban P-ECG group than in the urban conventional group in weekday night time/holiday (Figure 6A,B). However, the door-to-reperfusion and DTL times did not differ significantly between the urban P-ECG and conventional groups in weekday daytime (Figure 6C,D).
First medical contact to reperfusion time and first medical contact to catheterization laboratory time were significantly shorter in the urban P-ECG group than in the urban conventional group in weekday night time/holiday (Figure 7A,B). However, first medical contact to reperfusion time and first medical contact to catheterization laboratory time did not differ significantly between the urban P-ECG and conventional groups in weekday daytime (Figure 7C,D).
There was no advantage for urban cases alone, but when analyzed for all patients, the time from first medical contact to revascularization (122±59 vs. 96±33 min, P=0.037) and time from first medical contact to catheterization laboratory (90±58 vs. 69±28 min, P=0.045) for all patients who died in hospital were significantly longer than for patients discharged alive.
Discussion
The core findings of the present study are: (1) door-to-reperfusion time and DTL time did not differ between the rural and urban P-ECG groups, (2) patient transport in weekday night time/holiday was a factor in prolonged DTL time, and use of the P-ECG system improved this, and (3) in weekday night time/holiday, first medical contact to reperfusion time and first medical contact to catheterization laboratory time were significantly shorter in the urban P-ECG group than in the urban conventional group, but not significantly different in weekday daytime.
Rural and Urban Disparity
Rural and urban areas are very difficult to define.8 Previous studies have defined rural and urban areas in various ways, including by population density,9,10 rurality index,8 interviews with transporting physicians,11,12 and distance from the scene to the PCI facility.6 The definitions used in this study were chosen independently because of the importance of determining whether a patient was transported from within or outside the EMS jurisdiction.
One reason for the lower number of rural patients in both the conventional and P-ECG groups compared with urban patients in this study may be that rural patients are less likely to be transported directly to a PCI facility by EMS and more likely to be transported to a PCI facility via a nearby regional core hospital or general practitioner. Such patients were not included in the current study.
Influence of Procedure Time on Door-to-Reperfusion Time
In this study, procedure time defined as the interval from the door time to reperfusion was significantly longer in the P-ECG group than in the conventional group. This observation might be due to the fact that EMS teams tend to apply the P-ECG system to severe patients, including congestive heart failure, who required devices such as intra-aortic balloon pumping ventilator or pacemaker, which results in a longer procedure.
The large variation in procedure time between the 2 groups may be due to the tendency for younger physicians to perform the procedure first and more experienced physicians to take over in primary PCI.
Base on these observations, the DTL time might be more practical than door-to-reperfusion time for analyzing the time intervals of patient transfer.
DTL Time for Rural and Urban Areas
Patient transport time was 9 min for the urban P-ECG group compared with 37 min for the rural P-ECG group, a difference of 28 min. The urban P-ECG group was expected to have a longer DTL time than the rural P-ECG group because of the shorter time to prepare for PCI. However, in the present study, there was no significant difference between the 2 groups. PCI preparation occurs between ECG transmission by the EMS and the arrival of the patient at the hospital. The time for PCI preparation includes the time the EMS team stays at the scene, which averaged 14 min in the urban P-ECG group and when combined with the 9 min of patient transport time, consumes some time. This may be one of the reasons why the DTL time was shorter in the P-ECG group even in urban areas.
Efficacy of P-ECG System in Urban Areas
As in rural areas, operation of the P-ECG system reduced door-to-reperfusion and DTL times in urban areas. Because the average patient transport time in the urban P-ECG group was 9 min, there may be advantages to using the P-ECG system when transport times are longer than 9 min. The EMS stayed on the scene on average 14 min in the rural P-ECG group, which was also included in the patient transport time. Therefore, the PCI system was expected to be ready by the time the patient arrived at the hospital. In a previous study, patients from rural areas were transported a median of 30 km further than patients from urban areas, but this prolonged the system delay for EMS contact to balloon time by only 9 min in Aarhus County, Denmark.6 Those authors asserted that this phenomenon reflected the better preparatory conditions in the catheterization laboratory during longer transports, thus outweighing the potential disadvantage of living far from a primary PCI hospital.6 DTBT was shorter for primary PCI patients in rural areas compared with urban areas in our study, and ∼3 min in the previous study.6 The reason for the slight difference in times is thought to be due to the different transportation distances, transportation systems, and hospital acceptance systems in each region.
In urban areas, there are many institutions that can provide emergency medical care within a relatively short distance. During the weekday daytime, facilities and clinics that do not provide nighttime or holiday care may be included in the emergency transport options, but it may be difficult to select the optimal facility. We previously reported the advantages of P-ECG in optimal patient transport,5 and find it will be particularly useful in urban areas.
The EMS interviews showed that patients with more severe conditions were more willing to undergo P-ECG. For example, patients with left main trunk lesions were unevenly distributed, with 4 patients in the urban P-ECG group vs. 1 in the in the urban conventional group. Furthermore, when analyzed for all patients, max CK was significantly higher in patients with P-ECG recording than in those without P-ECG, even though the time factor was shorter. Such bias in the condition of the transported patients may be one reason why there was a significant difference in the time factor but no difference in in-hospital deaths between the patients with and without P-ECG. Another possible reason is that deaths in hospital were very low compared with all eligible patients. In fact, when analyzed for all patients, first medical contact to reperfusion time and first medical contact to catheterization laboratory time in all patients who died in hospital were significantly longer than those discharged alive, in this study.
Night Time/Holiday as a Factor in Delays in Urban Areas
In this study, we found larger time differences in door-to-reperfusion time, DTL time, first medical contact to reperfusion time, and first medical contact to catheterization laboratory time in urban areas, and larger time differences occurred between the P-ECG group and the conventional group at night and during holidays. In contrast, the advantage of P-ECG disappeared during the weekday daytime. We believe that P-ECG may result in a reduction in time for the cardiologist to be notified that a patient is coming to the hospital in need of primary PCI. For example, if an EMS transports a patient to a hospital at night time/holidays and there is no cardiologist on duty, a cardiologist will be called at that time point and preparations for primary PCI will then begin. However, P-ECGs are often transferred directly to the cardiologist, and preparation for primary PCI can begin immediately.5 During the weekday daytime, as cardiologists were already on duty, the preparation for PCI is quicker, and thus there was no difference between the P-ECG and conventional groups. In the previous study,7 patients treated with primary PCI during night time/holidays had longer DTBTs. Treatment during night time/holidays was an independent predictor of longer DTBT, and longer DTBTs were associated with higher mortality rates.7
DTBT and Door-to-Reperfusion Time
Many studies use the term DTBT,10,13,14 defined as the time from hospital arrival to the first device passage. However, there have been many other definitions such as door-to-intervention,15 median time interval from hospital arrival to reperfusion therapy,16 the time from hospital arrival to the first reperfusion catheter crossing the culprit lesion,17 etc. According to the purpose of this study, we considered the time from onset to reperfusion to be the prognostic factor in AMI, and defined this time interval as door-to-reperfusion time. Furthermore, we believe that evaluating the DTL time removes the procedure time bias and more reliably highlights the characteristics of the P-ECG system.
Future Issues for the P-ECG System
Compared with the number of AMI patient transports in Oita City, the number of P-ECGs performed was small. According to interviews with EMS teams, the reasons for this were that the hospital to which the patient was transported was very close to the scene, the physician at the destination gave priority to transport over P-ECG transmission, the patient did not have typical anginal pain, and the patient was transported by an ambulance that was not equipped with a P-ECG system.
In the future, it is considered important to further increase the operation of the P-ECG while maintaining a high level of optimization of patient transport by thoroughly educating and enlightening the EMS teams, using the results of this study as a guide.
Study Limitations
Several limitations need to be considered. First, when analyzed using the definitions of urban and rural in this study, it is likely that there were cases in which transportation from outside the nearby metropolitan area was more distant, even within the same city.
Second, the time from onset to reperfusion could not be assessed because the time of onset of STEMI was unknown.
Conclusions
Our results demonstrated that P-ECG is useful even in urban areas, especially in patients who develop STEMI during weekday nights or holidays. Further advances in the operation of P-ECG system will be important to improve the prognosis of STEMI patients in the future.
Acknowledgments
We thank all the cardiologists at the hospitals and EMS staff at the fire departments that participated in the Oita remote image transmission system.
We thank also Masae Hayashi, and Tomomi Syuto for their assistance with the manuscript.
Sources of Funding
This research received no financial support and no grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclosures
N.T. is a member of Circulation Journal’s Editorial Team.
Statement of Ethics
The authors have no ethical conflicts to disclose.
IRB Information
The Oita University Research Ethics Committee (No: 1262) approved this study.
References
- 1.
Kikuchi M, Tahara Y, Yamaguchi J, Nakashima T, Nomura O, Tanaka A, et al; Japan Resuscitation Council (JRC) Acute Coronary Syndrome (ACS) Task Force and the Guideline Editorial Committee on behalf of the Japanese Circulation Society (JCS) Emergency and Critical Care Committee. Executive Summary: Acute coronary syndrome in the Japan Resuscitation Council guidelines for resuscitation 2020. Circ J 2023; 87: 866–878.
- 2.
Kawakami S, Tahara Y, Noguchi T, Yagi N, Kataoka Y, Asaumi Y, et al. Time to reperfusion in ST-segment elevation myocardial infarction patients with vs. without pre-hospital mobile telemedicine 12-lead electrocardiogram transmission. Circ J 2016; 80: 1624–1633.
- 3.
Kobayashi A, Misumida N, Aoi S, Steinberg E, Kearney K, Fox JT, et al. STEMI notification by EMS predicts shorter door-to-balloon time and smaller infarct size. Am J Emerg Med 2016; 34: 1610–1613.
- 4.
Yufu K, Shimomura T, Fujinami M, Nakashima T, Saito S, Ayabe R, et al. Impact of mobile cloud electrocardiography system on door-to-balloon time in patients with acute coronary syndrome in oita prefecture. Circ Rep 2019; 1: 241–247.
- 5.
Kawano K, Yufu K, Shimomura T, Sato H, Ishii Y, Yonezu K, et al. Prehospital 12-lead electrocardiography system in oita assisted transport of “true” acute coronary syndrome patients to optimal institutes. Circ J 2022; 86: 1481–1487.
- 6.
Sørensen JT, Terkelsen CJ, Nørgaard BL, Trautner S, Hansen TM, Bøtker HE, et al. Urban and rural implementation of pre-hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Eur Heart J 2011; 32: 430–436.
- 7.
Rashid MK, Wells G, So DY, Chong AY, Dick A, Froeschl M, et al. Off-hours presentation, door-to-balloon time, and clinical outcomes in patients referred for primary percutaneous coronary intervention. J Invasive Cardiol 2023; 35: E185–E193.
- 8.
Muula A. How do we define ‘rurality’ in the teaching on medical demography? Rural Remote Health 2007; 7: 653.
- 9.
Cui ER, Fernandez AR, Zegre-Hemsey JK, Grover JM, Honvoh G, Brice JH, et al. Disparities in emergency medical services time intervals for patients with suspected acute coronary syndrome: Findings from the North Carolina Prehospital Medical Information System. J Am Heart Assoc 2021; 10: e019305.
- 10.
Fukui K, Takahashi J, Hao K, Honda S, Nishihira K, Kojima S, et al; JAMIR Investigators. Disparity of performance measure by door-to-balloon time between a rural and urban area for management of patients with ST-segment elevation myocardial infarction: Insights from the nationwide Japan Acute Myocardial Infarction Registry. Circ J 2023; 87: 648–656.
- 11.
Williams P, Bond C, Hannaford P, Ritchie L. Influences on general practitioners’ use of pre-hospital thrombolysis: A qualitative study. J Public Health 2004; 26: 38–41.
- 12.
Bloe C, Mair C, Call A, Fuller A, Menzies S, Leslie SJ. Identification of barriers to the implementation of evidence-based practice for pre-hospital thrombolysis. Rural Remote Health 2009; 9: 1100.
- 13.
Nakashima T, Hashiba K, Kikuchi M, Yamaguchi J, Kojima S, Hanada H, et al. Impact of prehospital 12-lead electrocardiography and destination hospital notification on mortality in patients with chest pain: A systematic review. Circ Rep 2022; 4: 187–193.
- 14.
Welsford M, Nikolaou NI, Beygui F, Bossaert L, Ghaemmaghami C, Nonogi H, et al. Part 5: Acute coronary syndromes: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2015; 132: S146–S176.
- 15.
Dhruva VN, Abdelhadi SI, Anis A, Gluckman W, Hom D, Dougan W, et al. ST-Segment Analysis Using Wireless Technology in Acute Myocardial Infarction (STAT-MI) trial. J Am Coll Cardiol 2007; 50: 509–513.
- 16.
Canto JG, Rogers WJ, Bowlby LJ, French WJ, Pearce DJ, Weaver WD, et al. The prehospital electrocardiogram in acute myocardial infarction: Is its full potential being realized? J Am Coll Cardiol 1997; 29: 498–505.
- 17.
Chan AW, Kornder J, Elliott H, Brown RI, Dorval JF, Charania J, et al. Improved survival associated with pre-hospital triage strategy in a large regional ST-segment elevation myocardial infarction program. JACC Cardiovasc Interv 2012; 5: 1239–1246.