論文ID: CJ-23-0388
論文ID: CJ-23-0388
Catheter ablation to treat symptomatic atrial fibrillation (AF) has steadily increased in popularity but rarely produces life-threatening complications, such as pulmonary vein stenosis (PVS), a refractory condition possibly leading to adverse clinical outcomes. Severe PVS associated with radiofrequency (RF) catheters has decreased dramatically from 42.4% in 19991 to 0.29% thereafter2 because of a shifting in strategy from ostial to antral ablation. Early-stage symptomatic PVS is difficult to detect and can progress rapidly, leading to complete PV obstruction, chronic pulmonary hypertension, and irreversible parenchymal damage and its sequelae.3 Intervention with PV balloon angioplasty or stenting has been reported but with suboptimal results.4,5
Article p ????
Further, balloon-based ablation has flourished, reducing procedure times and providing outcomes comparable to those for conventional RF-based ablation. In Japan, approximately 79,000 AF ablations were performed in 2020, with balloon-based treatments currently on track to exceed 20,000. Currently, available balloon-based ablation technologies include cryoballoon (CB), hot balloon (HB), and laser balloon (LB) systems. Both CB and HB systems are covered by insurance for use in persistent AF, and balloon-based technology usage increases yearly. However, there are only single-center reports on PVS associated with various balloon types, and none have compared systems side-by-side.
In this issue of the Journal, Tokuda and colleagues6 present the incidence and characteristics of PVS among 320 patients who underwent ablation any of the 3 balloon-based systems between 2017 and 2020 and then contrast-enhanced spiral CT 3 months later. The authors found mainly that the highest incidence of moderate (50–75%) PVS followed LB ablation, whereas the incidence of severe (>75%) PVS was similar for all balloon systems. Overall, severe PVS occurred in 7 (2.2%) patients, with only 1 (0.3%) complaining of PVS-related symptoms. That patient presented with chest pain and hemoptysis 6 months post-HB ablation and underwent urgent PV angioplasty.
The authors are to be commended for their in-depth follow-up of a large number of patients. Theirs is the first study to longitudinally examine the incidence and outcomes of PVS in relation to all 3 balloon types, providing new information on complications induced by modern balloon technologies.
Currently, the true incidence of balloon ablation-related PVS is unknown, as many centers do not routinely perform imaging post-balloon ablation. The 0.3% overall incidence of symptomatic PVS post-balloon ablation reported by Tokuda and colleagues is extremely low and comparable to that recently reported for conventional RF ablation. Thus, the data strongly suggest the safety of recently developed balloon devices for protection against PVS.
The Figure shows the heat transfer area for each balloon system. In CB: balloon surface from the northern hemisphere to equatorial plane; HB: all surfaces reached by conductive heating; LB: differs from the others by creating linear laser ablation lesions. Atrial muscles in the proximal PVs are sufficiently thick, whereas those in the distal PV sleeves appear more vulnerable to tissue damage from the transfer of thermal energy. Avoiding as much as possible delivering energy distally is considered essential to prevent PVS. Notably, Tokuda and colleagues found that using the HB and CB tended to result in stenosis distal (rather than proximal) to the atrial body, as shown in their table 3.6 As in the Figure, the HB and CB have a larger surface area and thus tend to more easily ablate the distal PVs. The data suggest that operators should be careful when positioning the balloon, to avoid PVS by distal ablation in the remote phase.
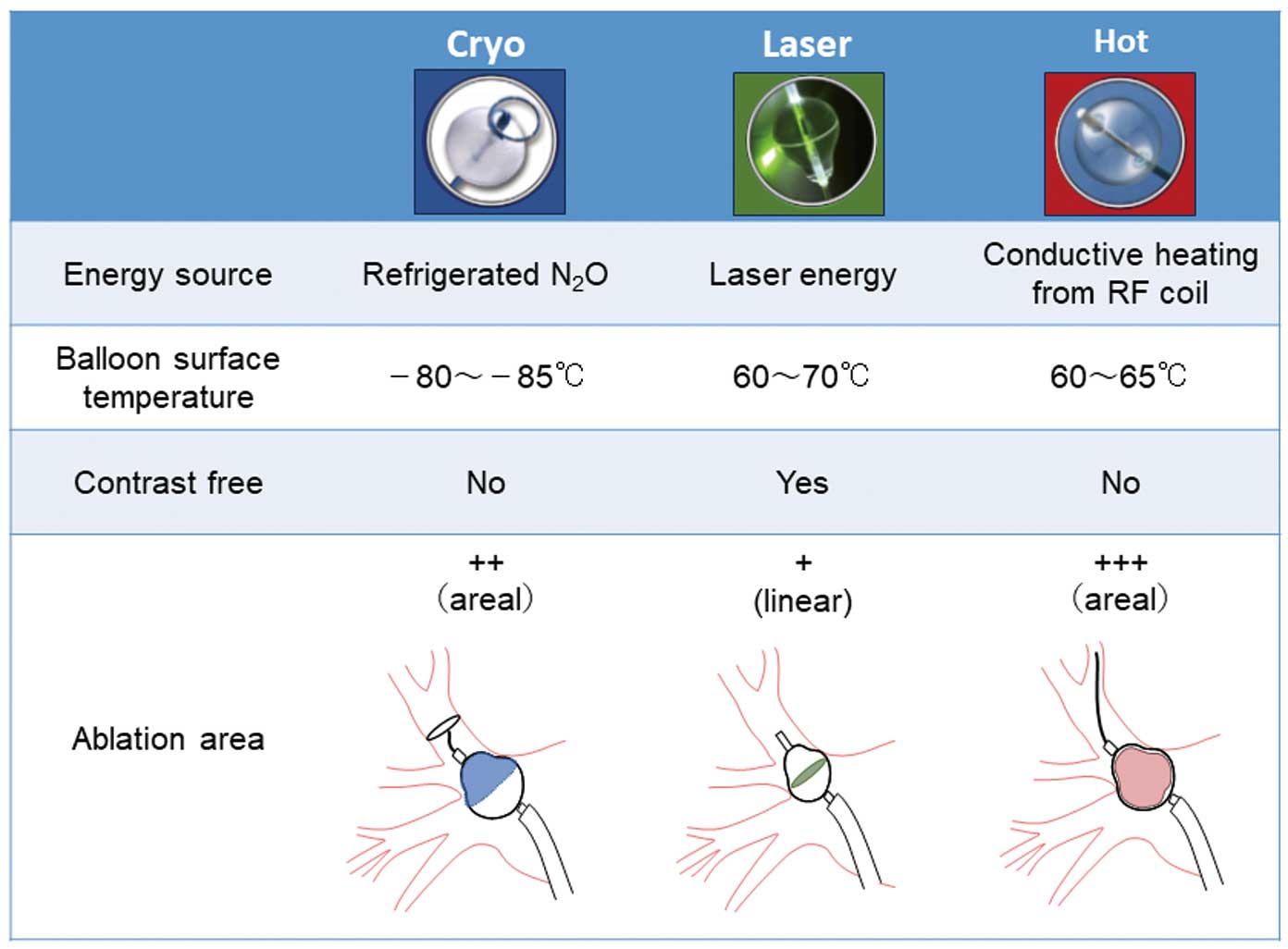
Details of the 3 current balloon ablation systems. RF, radiofrequency.
Although the LB system is a balloon system, it produces linear lesions like those of conventional RF systems. Specifically, the LB is dilated within the PV, blocking PV blood flow from distal sites, and the laser is applied to the target tissue under direct-vision facilitated by the built-in endoscope. Further, laser energy differs significantly from the other balloon systems’ energy and RF energy by penetrating the endocardium and producing transmural lesions from the mid-myocardium. Tokuda and colleagues report a relatively high incidence of moderate PVS, possibly for the following reasons. (1) LB ablation has just begun in Japan and thus there are many cases of early clinical use in which the influence of operator skill cannot be ruled-out. The incidence of moderate stenosis in skilled facilities overseas is relatively low.7 (2) First-generation LBs had poor compliance, making blocking blood flow and ensuring a good field of view challenging. Undeniably, unintentionally delivering excessive deep-tissue laser energy under these circumstances could result in remote phase linear waist-shaped stenosis. In contrast, the latest 3rd-generation LBs are highly compliant, facilitating interruption of blood flow and ensuring a stable field of view. In addition, they facilitate ultrafast, precision laser irradiation, thus reducing the amount of energy delivered to tissue. Further studies are needed to determine whether operator experience with 3rd-generation LBs will reduce the incidence of PVS.
Symptomatic severe PVS requiring angioplasty has, in Japan, been reported following CB ablation in 6 cases and HB ablation in 2.5,8–10 Although presently reported data suggest LB ablation frequently causes PVS, there are no reports worldwide associating LB ablation and the need for angioplastic intervention. Symptomatic PVS due to HB use occurred in only 1 (0.3%) of the presently reported cases, and currently, the incidence of serious symptomatic PVS post-balloon treatment is considered similar or lower than that following RF catheter treatment. This raises the question whether follow-up CT with radiation exposure and contrast administration is necessary for all patients undergoing balloon therapy. In a previous study, routine imaging screening of 976 conventional RF ablation patients revealed severe PVS in 0.7% and symptomatic PVS in only 0.1%.11 In the present study, severe PVS was recognized on imaging in 2.2% of cases, but symptomatic PVS was extremely low. In another study, 6% of cases had a zero pressure gradient with <50% stenosis on pulmonary venography, despite preoperative CT showing severe stenosis.12 Furthermore, it seems necessary to investigate whether Tokuda and colleagues’ measurement method also overestimated PVS.6
Among the presently reported patients, severe PVS tended to be more common in relatively young patients (average: 56 years). Other studies have also shown a predilection for younger patients,5,9 and further investigation may be needed to determine whether histologic PV vulnerability varies with age. At present, it can be said that follow-up CT may be necessary for younger patients, those with small-diameter PVs, those who require or receive distal PV treatment, and those with a marked increase in pulsed-wave Doppler PV flow velocity.
Symptomatic PVS is a rare but frightening post-AF ablation complication. Currently, its incidence is very low, and robust data to suggest routine CT imaging in all cases is lacking. However, it is essential that all healthcare professionals caring for patients treated with balloon devices, which has become increasingly common, are aware of both the various balloon devices’ characteristics and the signs and symptoms of PVS to diagnose it early and act quickly before chronic obstruction and its sequelae occur. Tokuda et al’s paper is both excellent and timely, covering the issues at hand, and certainly worthy of our attention.