論文ID: CJ-23-0521
論文ID: CJ-23-0521
Mitral transcatheter edge-to-edge repair (TEER) using the MitraClipTM (Abbott Vascular, Santa Clara, CA, USA) system is useful as a surgical treatment for severe secondary mitral regurgitation (MR).1,2 However, there are patients for whom TEER does not lead to an improved prognosis. The mitral valve anatomy and left ventricular morphology define the postoperative prognosis,3,4 and renal dysfunction is also recognized as one of the most important prognostic factors in patients undergoing TEER.5,6 In previous studies, serum creatinine and glomerular filtration rate (GFR) have been utilized as indicators of renal function, and they are powerful prognostic factors in cardiovascular disease.7,8
Article p ????
The sympathetic nervous system and the renin-angiotensin-aldosterone system (RAAS) control the circulation of the heart and kidneys, which regulates blood pressure and fluid volume. In addition to hemodynamic changes, various factors such as neurohumoral activation and chronic inflammation can exacerbate renal function in heart failure (HF). This close functional linkage between the heart and the kidneys is called the cardiorenal syndrome.9 Previous clinical studies have shown that the hemodynamic factor most associated with renal dysfunction in HF patients is central venous pressure, not cardiac output.8 Increased central venous pressure increases renal venous pressure, resulting in renal congestion, which in turn reduces renal blood flow and GFR and decreases sodium excretion. Moreover, renal congestion causes an increase in renal interstitial pressure, which might lead to a hypoxic state of the renal parenchyma.
Intrarenal perfusion can be visualized using intrarenal Doppler ultrasonography (IRD), and previous studies have shown that intrarenal venous flow (IRVF) is more associated with right-sided heart hemodynamics than intrarenal arterial flow, suggesting a tight correlation between IRVF and renal congestion.10,11 Therefore, Doppler-derived IRVF is known as a reliable and feasible visual biomarker of renal congestion and a predictor of prognosis in cardiovascular disease.
In this issue of the Journal, Kuwata et al12 show the clinical importance of evaluating Doppler-derived IRVF in 105 patients with secondary MR who underwent TEER. Discontinuous patterns of the IRVF waveform assessed preoperatively were independent prognostic determinants for all-cause death and HF hospitalization after TEER, despite adjusting for estimated GFR (eGFR). One point of interest in this study is that although the IRVF waveforms differed between the continuous and discontinuous groups, the eGFR in both groups was comparable at ≈40 (mL/min/1.73 m2). Because renal congestion should result in progressive renal dysfunction, the discontinuous flow pattern of IRVF in this study may not be solely due to renal congestion. Patients with moderate or greater tricuspid regurgitation (TR) were significantly more common in the IRVF discontinuous group than in the continuous group (66.6% vs. 24.4%, respectively, P<0.001), suggesting that moderate or greater TR may have caused the IRVF waveform to be discontinuous. It has already been demonstrated that impairments of the intrarenal venous circulation may occur even in the normal range of mean right atrial pressure, and impairment of renal perfusion may reflect moderate or greater TR.11 In addition, moderate or greater MR was also more common in the discontinuous IRVF group than in the continuous IRVF group (77.8% vs. 51.3%, respectively, P=0.008), indicating that secondary MR was difficult to control by adequate medical therapy before TEER in the discontinuous IRVF group. As a result, TR may have increased with the increased loading condition and chamber dilatation in the right-sided heart. Residual TR is a well-established predictor for impaired outcomes following surgical treatment of left-sided valvular heart disease,13 and increasing TR severity correlates with higher mortality rates in patients with MR undergoing TEER.14 In the present study,12 the postoperative IRVF waveform remained in a discontinuous pattern in most patients in the preoperative discontinuous flow group, even though the residual MR was ≤grade 2 in most patients. These results suggest that although MR was reduced by TEER, the increased loading condition in the right-sided heart or significant TR may have remained. The IVFR waveform pattern reflects not only renal congestion but also the right heart hemodynamics and significant TR, which may have been useful to evaluate the prognosis of secondary MR patients scheduled for TEER (Figure).
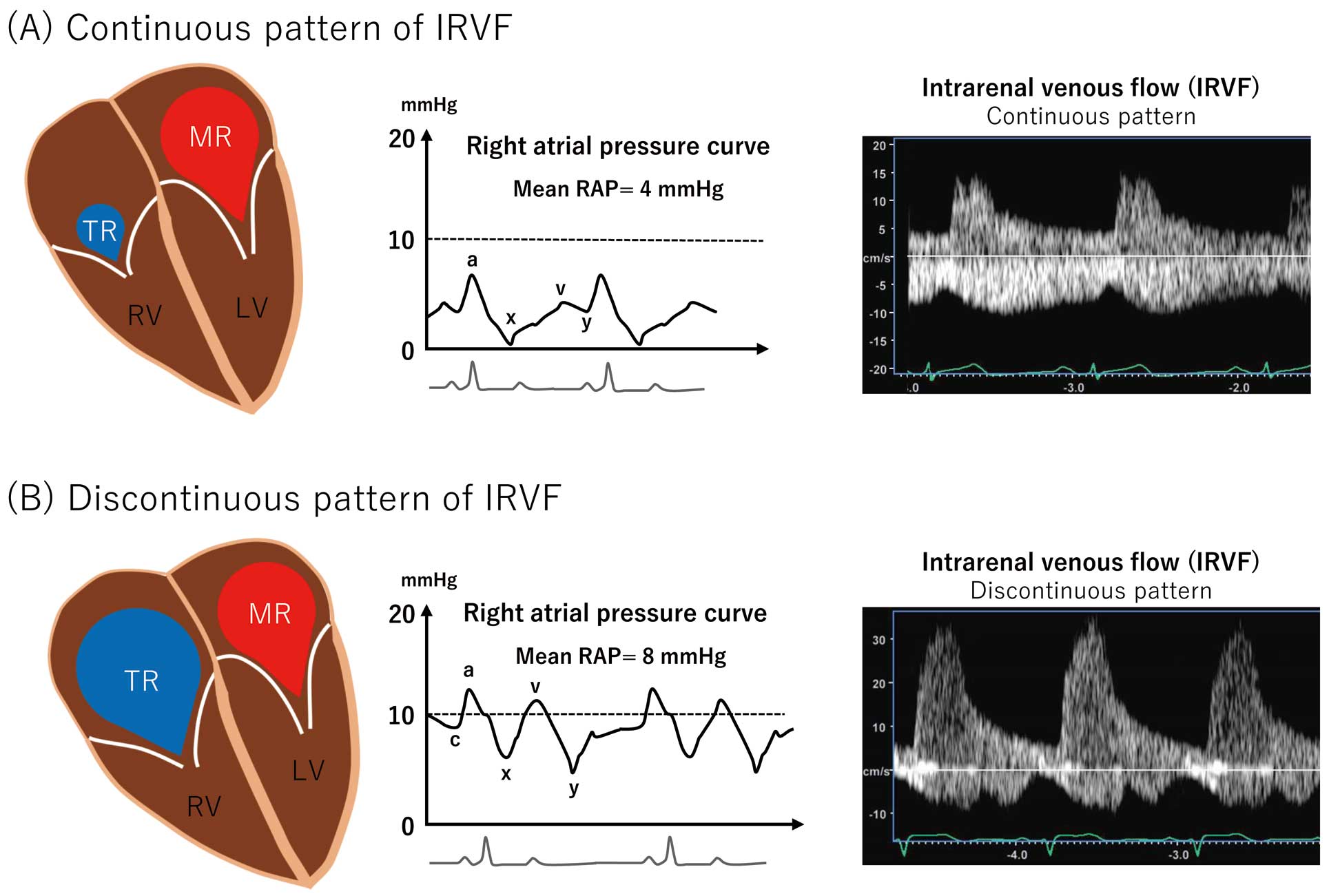
Schema showing hypothesized pathophysiology of different IRVF waveforms in patients with secondary MR. (A) In patients with secondary MR who present with continuous IRVF, TR may be less than moderate and mean RAP may be in the normal range. (B) In patients with secondary MR who present with discontinuous IRVF, TR may be equal to more than moderate and mean RAP may be elevated with high a-wave and v-wave. IRVF, intrarenal venous flow; MR, mitral regurgitation; RAP, right atrial pressure; TR, tricuspid regurgitation.
Although this was a single-center study of a small number of cases, it shows that analysis of IRVF waveforms by IRD may be a powerful prognostic marker for patients with secondary MR who undergo TEER. The usefulness of this clinical index should be validated in large multicenter studies.
S.K. has no conflicts of interest. Y.S. received a research grant from Canon Medical Systems Corporation and is a member of Circulation Journal’s Editorial Team.