論文ID: CJ-23-0613
論文ID: CJ-23-0613
Background: In 2016, the DANISH study reported negative results regarding the efficacy of implantable cardioverter-defibrillators (ICDs) in patients with non-ischemic cardiomyopathy (NICM) and reduced left ventricular ejection fraction (LVEF). In this study we determined the efficacy of using ICDs for primary prophylaxis in patients with NICM.
Methods and Results: We selected 1,274 patients with underlying cardiac disease who were enrolled in the Nippon Storm Study. We analyzed the data of 451 patients with LVEF ≤35% due to NICM or ischemic cardiomyopathy (ICM) who underwent ICD implantation for primary prophylaxis (men, 78%; age, 65±12 years; LVEF, 25±6.4%; cardiac resynchronization therapy, 73%; ICM, 33%). After propensity score matching, we compared the baseline covariates between groups: NICM (132 patients) and ICM (132 patients). The 2-year appropriate ICD therapy risks were 27.7% and 12.2% in the NICM and ICM groups, respectively (hazard ratio, 0.390 [95% confidence interval, 0.218–0.701]; P=0.002).
Conclusions: This subanalysis of propensity score-matched patients from the Nippon Storm Study revealed that the risk of appropriate ICD therapy was significantly higher in patients with NICM than in those with ICM.
Implantable cardioverter-defibrillators (ICDs) are used worldwide to prevent sudden cardiac death (SCD) in patients with ischemic and non-ischemic cardiomyopathy (ICM and NICM, respectively) who are at risk of fatal arrhythmic events.1–3 In 2016, the Danish Study to Assess the Efficacy of ICDs in Patients with Non-Ischemic Systolic Heart Failure on Mortality (DANISH) reported negative results on the efficacy of ICDs in patients with NICM and reduced left ventricular ejection fraction (LVEF).4 Thus, the European Society of Cardiology guidelines downgraded the indication of primary ICD prophylaxis for NICM patients with reduced LVEF from Class I to IIa.5 However, that change might be considered somewhat divorced from real-world ICD therapy, and we decided to use the Nippon Storm Study, a prospective observational study designed to gather clinical data from Japanese patients receiving ICD therapy, to determine whether the DANISH results are of equal value in the clinical setting.6,7
We aimed to determine the efficacy of ICDs as primary prophylaxis in patients with NICM. The incidence of ICD-appropriate therapy in patients with NICM was compared with that in patients with ICM, for whom primary ICD efficacy is generally recognized as a Class I indication for ICD implantation in Japanese guidelines.
The Nippon Storm Study design details have been previously published.6,7 Briefly, the study was organized by the Japanese Heart Rhythm Society and Japanese Society of Electrocardiology. Data collection concerning the registration of patients who had undergone a new transvenous ICD implantation began in October 2010 and was terminated in July 2012. Patient registration was conducted via a website at 48 Japanese ICD centers, and the Japanese Heart Rhythm Society collected patient data from physicians. The indications and uses of ICD implantation were determined by the attending cardiologists at each center based on the Japanese Circulation Society (JCS) guidelines for non-pharmacotherapy of cardiac arrhythmias (JCS 2011) for implantation of an ICD.8 This study was approved by the Institutional Review Board Ethics Committee of Kindai University (reference number: 10-04). Written informed consent was obtained from all patients. This study was conducted in accordance with the principles of the Declaration of Helsinki, revised in 2013.
ICD ProgrammingThe ICDs were programmed at each physician’s discretion. The following discrimination algorithms were used: PR Logic and Wavelet (Medtronic, Minneapolis, MN, USA), Rhythm ID (Boston Scientific, Marlborough, MA, USA), and Morphology Discrimination plus AV Rate Branch (St. Jude Medical, St. Paul, MN, USA). The ventricular fibrillation (VF) zone was ≥180–200 beats/min with at least 1 train of antitachycardia pacing (ATP) before the shock, and the ventricular tachycardia (VT) zone was ≥140–160 beats/min with at least 3 trains of ATP before the shock, which could be modified according to patient background and could be programmed for the fast VT zone if needed.
Follow-upFor precise follow-up, we constructed a new tracking system called “Chaser,” which was intended to minimize the loss of follow-up data. Data regarding ICD interventions were sent at a maximum interval of 6 months to the office of the Japanese Heart Rhythm Society. The ICD interventions were classified as ATP or shock therapy. An electrical storm was defined as the occurrence of ≥3 separate episodes of VT/VF within a 24-h period.9
Statistical AnalysisSummary statistics for baseline characteristics are expressed as frequencies and proportions for categorical data, and as mean and standard deviation (SD) for continuous variables. Patients’ characteristics were compared using χ2 or Fisher exact test for categorical outcomes and t-test for continuous variables.
The selection of treatment was influenced by patient-specific attributes, because the baseline characteristics of patients receiving a specific treatment often exhibited systematic disparities from those receiving alternative treatments. This consideration holds significant importance when estimating the effects of treatment or exposure on outcomes through observational data. One of the strategies used to eliminate treatment selection bias and confounding factors is propensity score (PS) matching, which enables the design and analysis of observational studies to emulate some attributes of randomized controlled trials. Patient selection was performed using the PS-matching method with a greedy 5 : 1 digit-matching algorithm for demographic and clinical factors, including age, sex, cardiac resynchronization therapy with a defibrillator (CRT-D), and LVEF. After all PS matching was performed, baseline covariates were compared between 2 groups. The 2 groups were made comparable through baseline demographic and clinical factor matching, including age, sex, CRT-D, and LVEF, using PS matching. This matching was achieved with a 1 : 1 greedy nearest neighborhood matching method with a caliber of 0.2 SD for the logit of the estimated PS.
We compared the incidence of ICD therapies between the primary prophylaxis groups of patients with ICM and NICM. For time-to-event outcomes, the Kaplan-Meier method was used to estimate overall and cardiovascular survival within each group. The differences in the survival curves between groups were tested by log-rank test. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using a Cox proportional hazards model. Given that death presents a competing risk for loss to follow-up, the cumulative incidence of ICD therapies was ascertained using a competing risk analysis, which used the Fine-Gray extension of the proportional hazards model, accounting for death as a competing risk. The cumulative incidence was modeled using the subdistribution hazard according to the Fine-Gray approach. All comparisons were preplanned, and the tests were conducted with a two-sided approach. Statistical significance was set at a P value <0.05. All statistical analyses were performed using the SAS software (version 9.4; SAS Institute, Cary, NC, USA).
We focused on 451 patients who underwent primary prophylactic ICD implantation among 1,274 patients with structural heart disease. After PS matching, the analysis was restricted to 264 patients: 132 (50%) who underwent ICD implantation due to ICM and 132 (50%) who underwent ICD implantation due to NICM. A flow chart of patient classification is shown in Figure 1.
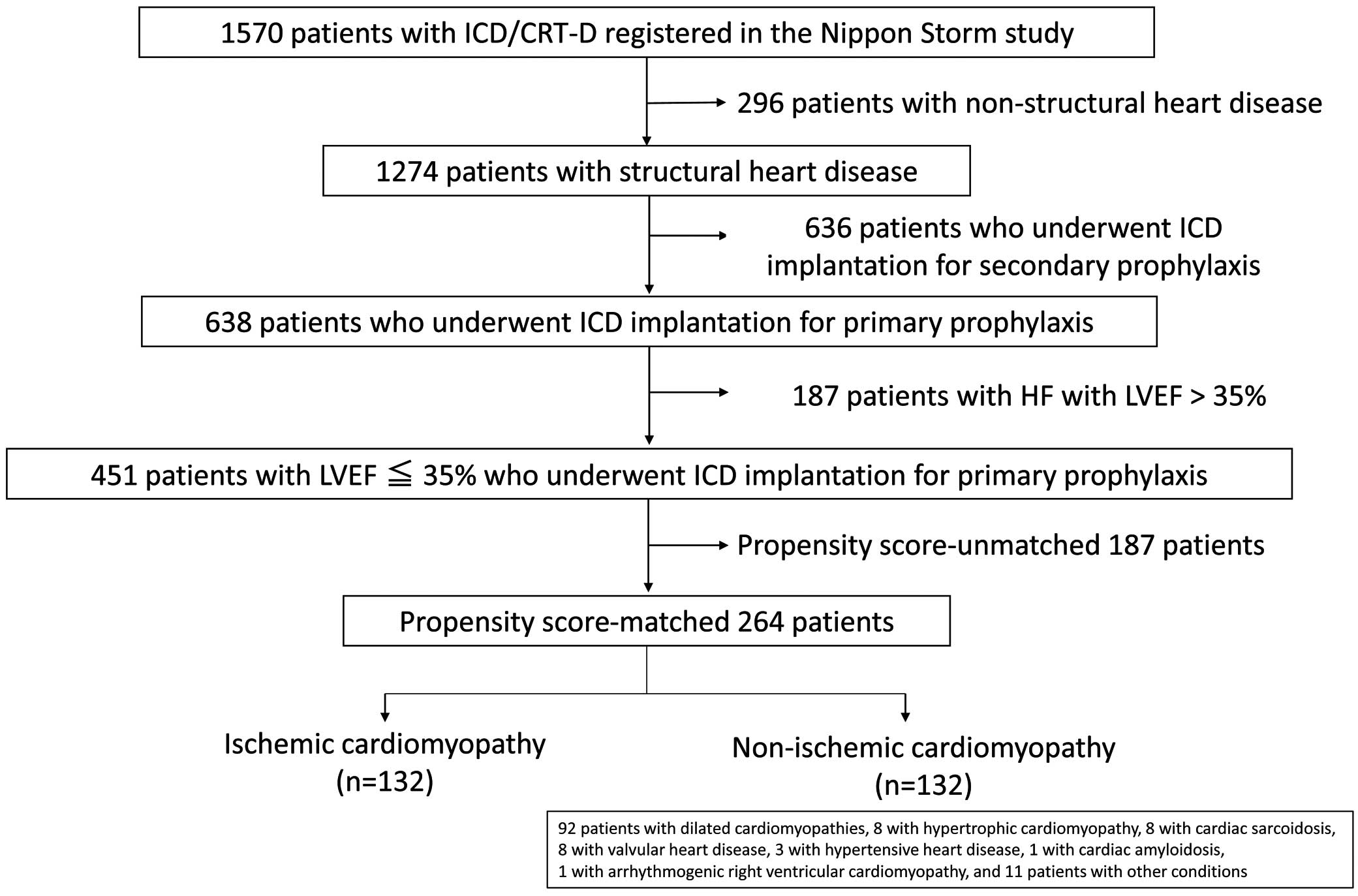
Flow diagram of patient classification in the study. CRT-D, cardiac resynchronization therapy with defibrillator; HF, heart failure; ICD, implantable cardioverter-defibrillator; LVEF, left ventricular ejection fraction.
Baseline Patient Characteristics
In the overall cohort of patients who received a primary prophylactic ICD, the mean (±SD) age was 66 (±12) years, and 78% of patients were male (Table 1). Most of the baseline characteristics differed between the ICM and NICM groups (Table 2). Male sex was more common in the NICM group than in the ICM group. The patients in the NICM group were older, were more likely to receive CRT-D, and had more severe heart failure (HF).
Baseline Clinical Characteristics
| Primary prophylaxis (n=451) | |
| Sex, male | 353 (78.3%) |
| Age, years | 65.5±11.6 |
| ICM | 149 (33.0%) |
| CRT-D | 327 (72.5%) |
| NYHA functional class III or IV | 256 (56.8%) |
| LVEF | 25.1±6.4 |
| BNP, pg/mL | 637.8±843.2 |
| Hb, g/dL | 12.8±2.1 |
| HT | 184 (40.8%) |
| DL | 127 (28.2%) |
| DM | 148 (32.8%) |
| Stroke | 42 (9.3%) |
| HU | 77 (17.1%) |
| PAD | 10 (2.2%) |
| 3VD or LMT | 51 (11.3%) |
| Diuretics | 355 (80.3%) |
| β-blocker | 342 (77.0%) |
| ACE-I or ARB | 325 (74.4%) |
| Antiplatelet agent | 176 (39.6%) |
| Anticoagulant agent | 216 (48.6%) |
| Class III antiarrhythmic drugs | 124 (27.9%) |
Values are presented as mean±standard deviation or n (%). ACE-I, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor; BNP, B-type natriuretic peptide; CRT-D, cardiac resynchronization therapy with a defibrillator; DL, dyslipidemia; DM, diabetes mellitus; Hb, hemoglobin; HT, hypertension; HU, hyperuricemia; ICM, ischemic cardiomyopathy; LMT, left main trunk; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; PAD, peripheral arterial disease; 3VD, 3-vessel disease.
Baseline Characteristics of Unmatched and Propensity Score-Matched Cohorts
| Unmatched cohort | Matched cohort | |||||
|---|---|---|---|---|---|---|
| ICM (n=149) | NICM (n=302) | P value | ICM (n=132) | NICM (n=132) | P value | |
| Male (%) | 131 (87.9) | 222 (73.5) | <0.001 | 114 (86.4) | 116 (87.9) | 0.854 |
| Age (years) | 69.3±8.7 | 63.6±12.4 | <0.001 | 68.5±8.6 | 67.9±10.3 | 0.618 |
| CRT-D (%) | 90 (60.4) | 237 (78.5) | <0.001 | 87 (65.9) | 92 (69.7) | 0.598 |
| NYHA functional class III or IV (%) | 74 (49.7) | 182 (60.3) | 0.034 | 68 (51.5) | 75 (56.8) | 0.459 |
| LVEF (%) | 26.5±6.0 | 24.4±6.5 | 0.001 | 26.1±6.1 | 26.4±6.5 | 0.718 |
| BNP (pg/mL) | 555.7±595.4 | 678.7±941.0 | 0.16 | 567.3±618.5 | 714.3±1,127.8 | 0.202 |
| Hb (g/dL) | 12.4±2.1 | 13.1±2.0 | 0.001 | 12.5±2.1 | 13.0±2.0 | 0.048 |
| HT (%) | 83 (55.7) | 101 (33.4) | <0.001 | 72 (54.5) | 52 (39.4) | 0.019 |
| DL (%) | 63 (42.3) | 64 (21.2) | <0.001 | 58 (43.9) | 24 (18.2) | <0.001 |
| DM (%) | 68 (45.6) | 80 (26.5) | <0.001 | 60 (45.5) | 37 (28.0) | 0.005 |
| Stroke (%) | 17 (11.4) | 25 (8.3) | 0.303 | 16 (12.1) | 10 (7.6) | 0.302 |
| HU (%) | 28 (18.8) | 49 (16.2) | 0.508 | 25 (18.9) | 22 (16.7) | 0.748 |
| PAD (%) | 6 (4.0) | 4 (1.3) | 0.089 | 6 (4.5) | 2 (1.5) | 0.282 |
| 3VD or LMT (%) | 51 (34.2) | 0 (0.0) | <0.001 | 46 (34.8) | 0 (0.0) | <0.001 |
| Drugs | ||||||
| Diuretic agent (%) | 117 (79.1) | 238 (81.0) | 0.704 | 104 (79.4) | 99 (76.7) | 0.654 |
| β-blocker (%) | 109 (73.6) | 233 (78.7) | 0.234 | 96 (73.3) | 98 (74.8) | 0.888 |
| ACE-I/ARB (%) | 107 (73.3) | 218 (74.9) | 0.728 | 95 (73.6) | 93 (72.1) | 0.889 |
| Antiplatelet agent (%) | 120 (81.1) | 56 (18.9) | <0.001 | 105 (80.2) | 26 (19.8) | <0.001 |
| Anticoagulant agent (%) | 65 (43.9) | 151 (51.0) | 0.19 | 56 (42.7) | 56 (42.7) | 1 |
| Class III antiarrhythmic drug (%) | 45 (30.4) | 79 (26.7) | 0.433 | 42 (32.1) | 35 (26.7) | 0.416 |
Values are presented as mean±standard deviation or n (%). NICM, non-ischemic cardiomyopathy. Other abbreviations as in Table 1.
ICD Therapy
In the matched cohort, the 2-year appropriate ICD therapy risk was 27.7% and 12.2% in the NICM and ICM groups, respectively (HR=0.390 [95% CI, 0.218–0.701], P=0.002; Figure 2). The 2-year appropriate ATP risk was 25.5% and 11.4% in the NICM and ICM groups, respectively (HR=0.417 [95% CI, 0.226–0.766], P=0.005), and the appropriate shock therapy risk was 6.3% and 1.6% in the NICM and ICM groups, respectively (HR=0.230 [95% CI, 0.049–1.085], P=0.063]). The 2-year electrical storm risks were 8.1% and 2.6% in the NICM and ICM groups, respectively (HR=0.292 [95% CI, 0.080–1.057], P=0.061). The 2-year inappropriate ICD therapy risk was 10.5% and 3.1% in the NICM and ICM groups, respectively (HR=0.376 [95% CI, 0.134–1.055], P=0.063; Figure 3).
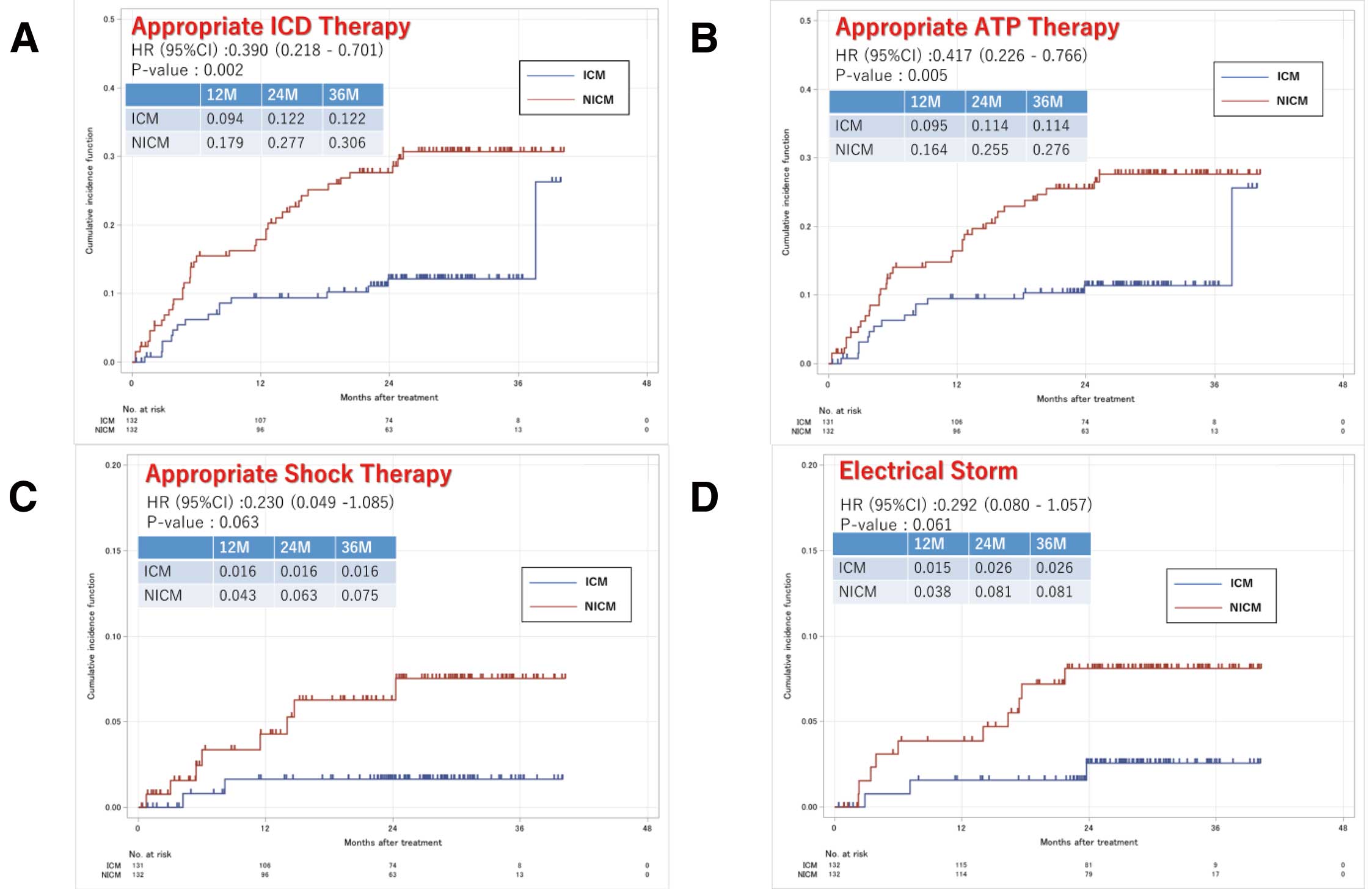
Incidence of appropriate implantable cardioverter-defibrillator therapy (A), appropriate ATP therapy (B), appropriate shock therapy (C), and electrical storm (D) in the propensity score-matched cohorts of patients with ischemic cardiomyopathy and non-ischemic cardiomyopathy. ATP, antitachycardia pacing; HR, hazard ratio; ICD, implantable cardioverter-defibrillator; ICM, ischemic cardiomyopathy; NICM, non-ischemic cardiomyopathy.
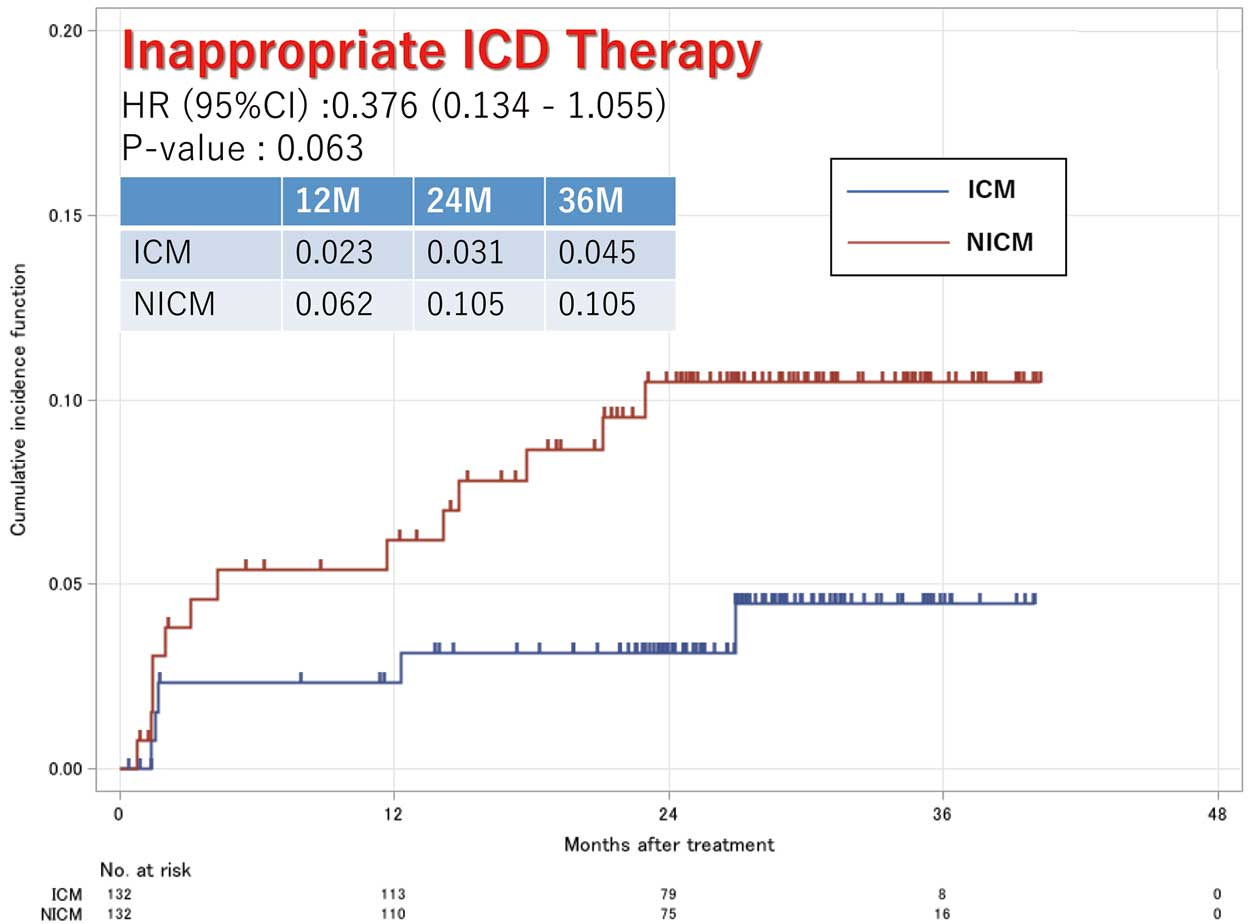
Incidence of inappropriate implantable cardioverter-defibrillator therapy in the propensity score-matched cohorts of patients with ischemic cardiomyopathy and non-ischemic cardiomyopathy. HR, hazard ratio; ICD, implantable cardioverter-defibrillator; ICM, ischemic cardiomyopathy; NICM, non-ischemic cardiomyopathy.
Survival
In this matched cohort, 40 (15.2%) all-cause deaths and 18 (6.8%) cardiovascular deaths, among which 15 (5.7%) were HF-related and 3 (1.1%) were SCDs, occurred over a median follow-up of 815 (interquartile range, 652–949) days. The 2-year event-free overall survival rate was 85.3% and 86.3% in the NICM and ICM groups, respectively (HR=1.255 [95% CI, 0.955–1.649], P=0.103; Figure 4). The 2-year cardiovascular risk was 5.8% and 4.8% in the NICM and ICM groups, respectively (HR, 1.329 [95% CI, 0.519–3.400], P=0.553).

Event-free overall survival (A) and incidence of cardiovascular survival (B) in the propensity score-matched cohorts of patients with ICM and NICM. HR, hazard ratio; ICD, implantable cardioverter-defibrillator; ICM, ischemic cardiomyopathy; NICM, non-ischemic cardiomyopathy.
The major findings from this study of patients who received a primary prophylactic ICD in Japan were that (1) the risk of appropriate ICD therapy was significantly higher in patients with NICM than in those with ICM; (2) the risk of appropriate ICD shock therapy and electrical storm were comparable between the NICM and ICM patient groups; and (3) no significant differences in mortality or cardiovascular survival rates were observed between the NICM and ICM groups.
Differences in the Risk of SCD According to EtiologyAlthough ICD therapy is effective in preventing SCD in patients with HF and reduced LVEF resulting from either ICM or NICM, the benefits of prophylactic ICD vary according to the type of cardiomyopathy. Individuals with ICM have demonstrated consistent mortality benefits in large multicenter randomized trials of ICD vs. those who received conventional medical therapy in the early 2000s.1,2,10 However, randomized trials examining the use of prophylactic ICD implantation in patients with NICM have yielded variable results.11–15
Recently, the DANISH study failed to demonstrate a significant mortality benefit of ICD therapy over medical therapy alone among 1,116 patients with NICM and LVEF ≤35%.14 In addition, novel therapies, such as the use of angiotensin-receptor neprilysin inhibitors (ARNI) and sodium glucose cotransporter 2 inhibitors (SGLT-2i), have improved patient survival, hospitalization, and outcomes in this specific population of patients with HF. Based on these findings, together with the results of the DANISH trial, the new European Society of Cardiology guidelines have softened the recommendations for ICD implantation as primary prophylaxis in patients with NICM.5 Patients with ICM remain under the Class Ia recommendation for ICD implantation, whereas those with symptomatic systolic NICM have been downgraded from a Class I recommendation to a Class IIa recommendation.
However, in our opinion, this change may be somewhat out of step with real-world ICD therapy. In fact, a prespecified subgroup analysis of DANISH demonstrated a significant age interaction by showing a beneficial effect of primary prophylactic ICD implantation on all-cause and cardiovascular deaths in patients aged ≤70 years, but not in those aged >70 years.16 Consequently, a recent consensus report from the Heart Failure Association of the European Society of Cardiology stated that it may be acceptable to abstain from ICD implantation in patients aged >70 years with NICM and reduced LVEF.17 A recent meta-analysis, including all available randomized trials, showed a survival benefit of ICD therapy for the primary prophylaxis of NICM. Treatment with an ICD was associated with a 23% risk reduction for all-cause death and a 57% risk reduction for SCD.18 These findings, together with those of the DANISH trial, highlight the need for improved patient selection when referring patients with NICM for ICD therapy for primary prophylaxis. Therefore, significant differences in demographic variables and comorbid conditions exist between patients with NICM and those with ICM, which may contribute to the disparities in outcomes.19,20
Moreover, a high proportion of patients in the DANISH trial received a cardiac resynchronization therapy (CRT) device, which improved the prognosis of patients with HF. However, the results were independent of whether the patients received a CRT device in the main study.4 Thus, in the contemporary era and in optimally treated patients with HF with reduced EF, it may be difficult to show a significant benefit of ICD implantation for primary prophylaxis. Therefore, the patients who may benefit from this therapy should be identified. In contemporary settings, it is important to incorporate additional parameters beyond the LVEF and cardiomyopathy type to identify patients who will benefit significantly from primary ICD therapy. Several risk stratification scores, such as the MADIT-ICD benefit score, have been developed to assist physicians in this challenging task.21
Primary Prophylactic Effects of ICD Implantation in Patients With HF Demonstrated in JapanThe CHART-2 trial, which investigated the prognosis of patients with HF in Japan, provided the basis for determining the recommended levels in the JCS guidelines.22 The study enrolled 2,778 HF patients with New York Heart Association (NYHA) functional class II–III (2,247 with ICM and 531 with NICM). They were further classified by LVEF or non-sustained VT (NSVT) into Groups A (LVEF=35% and NSVT, n=56), B (LVEF ≤35% and no NSVT, n=259), and C (LVEF ≥35%, n=2,463) and were prospectively followed for prognosis. During a mean follow-up period of 3.2 years, the incidence of fatal arrhythmic events was 16.1% in Group A, 8.9% in Group B, and 1.9% in Group C. The annual incidence rates were 5.0%, 2.8%, and 0.6%, respectively, and were significantly higher in Groups A and B. In addition, the incidence rate was significantly higher in Groups A and B than in Group C. Surprisingly, 44.4% and 8.2% of patients in Groups A and B, respectively, were treated with ICDs, which are indicated for Class IIa or higher by the JCS guidelines, highlighting the critical issue of the underuse of ICDs. Although the number of patients in Group A was small in Japan (2% of patients with HF), there are definitely high-risk patients (Low EF + NYHA I or higher + NSVT) who require active use of ICDs.
The Nippon Storm Study and Its SubanalysesThe Nippon Storm Study is the largest prospective registry study of patients who have undergone ICD implantation in Japan, and the main study was published by Noda et al in 2018.23 The study enrolled 1,570 patients and investigated the prognostic effect of electrical storm in 1,270 with structural heart disease. After a mean follow-up of 28 months, 6.6% of patients had experienced electrical storms, and their mortality rate was twice that of patients who had not experienced electrical storms (HR: 2.10, P=0.0048). The following are the results of the subanalysis performed after publication of the main study.
In a previous subanalysis of the Nippon Storm Study, the authors evaluated the appropriateness of primary prophylactic ICD indication in patients with ICM and found that the risk of electrical storm was significantly higher in patients who received secondary prophylaxis than in those who received primary prophylaxis. However, appropriate ICD therapy is commonly applied at rates comparable to those of primary or secondary prophylaxis in patients with ICM. The importance of prophylactic ICD implantation in Japanese patients with ICM was demonstrated in a prospective Japanese registry.24 In addition, Sasaki et al demonstrated that the incidence of appropriate ICD therapy and electrical storms was significantly higher in their secondary prophylactic group than in their primary prophylactic group in PS-matched Japanese patients with ICM.25 However, the risk of ICD shock was comparable between the groups in this analysis.25
The mechanism by which the incidence of appropriate ICD therapy for patients with NICM was higher than that for patients with ICM in this subanalysis remains unclear. However, several clinical trials comparing appropriate ICD therapy rates in patients with NICM with those in patients with ICM have shown similar results to the present study.26,27 The fact that ARNI, which are believed to prevent more appropriate ICD therapy in NICM than in ICM, were not approved in Japan at the beginning of this study and thus could not be used in combination may be a reason for the higher NICM activation rate.28 Although this subanalysis of the Nippon Storm Study showed that patients with NICM received appropriate ICD therapy more frequently and were at significantly higher risk of having an electrical storm than patients with ICM, there was no difference in all-cause and CV deaths between the 2 groups. This finding seems to contradict the main results in the Nippon Storm Study, but the following are pertinent: (1) the PS-matched analysis excluded patients with more severe NICM, (2) electrical storms may be more strongly related to prognosis in patients with ICM than in those with NICM, (3) the appropriate adjunctive treatment might be taken after an electrical storm in ICM patients, and (4) intensive HF treatment may have become the focus after appropriate ICD therapy, which might have improved patient survival in the NICM group.
Prophylactic ICD Therapy in the JCS GuidelinesPrevious studies have established the effectiveness of primary prophylaxis against ICM.1–3 According to the current JCS guidelines, in both patients with ICM and NICM, ICD implantation is indicated for Class I if the LVEF ≤35%, NSVT is present, and the patient’s condition is classified as NYHA II–III.29 As previously mentioned, the prognosis of Japanese patients who meet the criteria for primary ICD prophylaxis was poor in the CHART-2 trial. In addition, the HINODE registry from Japan has recently shown that primary prophylactic ICDs were effective in patients with appropriate risk levels.30 Moreover, the results of this subanalysis showed that the incidence of appropriate ICD therapy was significantly higher in patients with NICM than in those with ICM. Therefore, it is premature to downgrade the indications for ICD implantation for NICM in the forthcoming Japanese guidelines. Risk stratification for SCD prophylaxis based on the NICM and ICM guidelines in Japan is reasonable. However, the advent of novel HF medications, such as ARNI, SGLT-2i, and vericiguat, may affect the previously established prognostic value of ICDs. Therefore, the results of large-scale prospective clinical trials are eagerly anticipated.
Study LimitationsFirst, its prospective observational design and multicenter registry resulted in a lack of randomization. Moreover, the sample size was relatively small and underpowered, particularly in the PS-matched analysis; therefore, hidden bias is possible. Second, both model selection and detailed programming of the ICDs were performed at the discretion of the attending physician. Therefore, differences in the tachycardia detection rates and length of the detection interval affected the incidence of ICD therapy, and overtreatment for self-terminating VT/VF was possible. Additionally, differences in tachycardia discrimination algorithms among manufacturers may affect the incidence of inappropriate ICD therapy. Third, the guideline-directed medical therapy for NICM was clearly suboptimal compared with that used in recent Western trials, which also contributed to the incidence of ICD therapy. Fourth, the underlying heart disease of NICM was determined at the discretion of each institution, and no cardiac magnetic resonance imaging data were collected in this study. This may have obscured the predictors of primary prophylaxis. Fifth, because the patients in this study were enrolled between 2010 and 2012, the indication criteria for an ICD and CRT-D were based on the guidelines for non-pharmacotherapy of cardiac arrhythmias (JCS 2011). Therefore, the indication criteria for CRT-D differed slightly from those in the current guidelines,22 in which the presence or absence of a left bundle branch block and QRS width are stated as the indication criteria for CRT-D. These differences may have affected the incidence of ICD therapy and prognosis of patients who received CRT-D.
The present subanalysis of the Nippon Storm Study revealed that the risk of appropriate ICD therapy was significantly higher in patients with NICM than in those with ICM, based on a PS-matching method.
We gratefully acknowledge all 48 Japanese implantable cardiac shock device centers involved in this study and the office of the Japanese Heart Rhythm Society, especially Ms. Yoko Sato, as well as Ms. Shoko Narumi and Mr. Hitoshi Ono for data collection.
No financial support.
This study did not receive any specific funding. Y.K. received lecture fees from Daiichi-Sankyo, Bayer Yakuhin, Abbott Medical Japan, Biotronik Japan, Boston Scientific Japan, and Japan Lifeline; T. Noda received lecture fees from Medtronic Japan and Biotronik Japan and belongs to the endowed department supported by Biotronik Japan; T.K. received lecture fees from Medtronic Japan, Abbott Medical Japan, and Biotronik Japan.
This study was approved by the Institutional Review Board’s Ethics Committee of Kindai University (reference number: 10-04).
The data generated in this study will not be shared.