Abstract
To identify those who might benefit from weight reduction within a large population of obese individuals, Japan Society for the Study of Obesity (JASSO) advocated the concept of “obesity disease.” Here we summarize the definition, criteria, and core concepts for the management of obesity disease based on JASSO’s latest guideline. JASSO defines obesity as excessive fat storage in adipose tissue associated with a BMI of ≥25 kg/m2. The threshold BMI of obesity is low as compared to Western countries given that Japanese individuals tend to develop obesity-related health disorders at lower BMI. Obesity with a BMI of ≥35 kg/m2 is referred to as “high-degree obesity” as treatment strategies vary based on the degree of obesity. Obesity is diagnosed as “obesity disease” if accompanied by any of the 11 specific obesity-related health disorders that weight reduction can prevent or alleviate, or if it meets the criteria for visceral fat obesity with a visceral fat area of ≥100 cm2. The initial weight reduction goals for high-degree obesity disease range from 5% to 10% of their current body weight, depending on the associated health disorders. That for those with obesity disease who do not qualify as high-degree is 3% or more. If these initial goals are not achieved, intensifying dietary therapy or introducing drug therapy (or both) may be necessary. While surgical treatment is primarily indicated for high-degree obesity disease, it might be appropriate for cases of obesity disease with a BMI <35 kg/m2, depending on the accompanying health disorders. Enhancing the quality of life for individuals with obesity or obesity disease necessitates a broader societal approach, emphasizing the resolution of related stigma.
Introduction
Not all individuals with a large body mass require treatment, from both medical and social perspectives. To identify those who might benefit from weight reduction from among a large population of obese individuals, Japan Society for the Study of Obesity (JASSO) more than 20 years ago advocated the concept of “obesity disease” [1, 2]. Obesity disease is diagnosed not solely on the basis of body mass index (BMI) but rather if a high BMI is accompanied by (i) specific obesity-related health disorders or (ii) visceral fat accumulation, which is an important risk factor for such health disorders. The decision to base medical need not only on the extent of obesity (BMI) but also on accompanying obesity-related health disorders or visceral fat accumulation was clear and rational. Since the initial publication of these diagnostic criteria [1, 2], JASSO has continually updated the guidelines for management of obesity disease [3-5] in order to promote the treatment of patients in line with this concept. We here summarize the definition, criteria, and core concepts for the management of obesity disease based on the latest guidelines of JASSO published in 2022 [5], and we discuss the goals of JASSO to be achieved through its scientific and social activities.
Definition of Obesity
Obesity is defined by JASSO as excessive fat storage in adipose tissue associated with a BMI of ≥25 kg/m2 (Table 1). This threshold of BMI for the definition of obesity was first established in the guidelines published in 2000 [1] and is based on the finding that the mean number of obesity-related health disorders—including glucose intolerance, dyslipidemia, and hypertension—exceeded 1.0 when BMI reached 25 kg/m2 for individuals who underwent health checkups [2]. This threshold, which has been consistently adopted in subsequent guidelines [3-5], is lower than that of other guidelines such as those of the World Health Organization (WHO), the latter stipulating that individuals with a BMI of ≥25 but <30 kg/m2 are overweight and those with a BMI of ≥30 kg/m2 are obese [6]. However, individuals of East Asian ethnicity, including Japanese, tend to develop certain obesity-related health disorders at a lower BMI than do those of European ethnicity [7-9], with the risk of developing diabetes or nonalcoholic fatty liver disease (NAFLD) at a BMI of 30 kg/m2 in the latter being almost equal to that at a BMI of 25 kg/m2 in the former [10, 11]. Such a lower BMI threshold is therefore appropriate for the identification of individuals of Japanese ethnicity who are in need of medical intervention.
Table 1
Definition and diagnosis of obesity disease
| Definition of obesity |
| Excess fat storage in adipose tissue |
| Body mass index (BMI) of ≥25 kg/m2 |
| Classification of obesity levels |
| Obesity with a BMI of ≥35 kg/m2 is defined as high-degree obesity |
| Definition of obesity disease |
| A condition that is characterized by obesity accompanied by obesity-induced or obesity-associated health disorders, or by a high probability of their development, and which from a medical viewpoint requires body weight reduction |
| Diagnosis of obesity disease |
| Category 1: Obesity accompanied by any one of 11 specific obesity-related health disorders |
| Category 2: Obesity accompanied by visceral fat obesity (visceral fat obesity is a diagnostic criterion for obesity disease even in the absence of apparent obesity-related health disorders) |
| Diagnosis of visceral fat obesity |
| Accumulation of visceral fat is screened for by measurement of waist circumference (male ≥85 cm, female ≥90 cm). Visceral fat obesity is diagnosed when a visceral fat area of ≥100 cm2 is confirmed by computed tomography or other modalities |
The proportion of the adult population with a BMI of ≥30 kg/m2 is approximately 5% and 35% in Japan and the United States, respectively, with the average value for countries in the Organisation for Economic Co-operation and Development (OECD) being 15% [12, 13]. On the other hand, the proportion of the adult population with a BMI of ≥25 kg/m2 in Japan is about 25% [12, 14] (Fig. 1). Whereas it is commonly stated that Japan has a low obesity rate, the proportion of obese people in Japan—based on the diagnostic criteria of JASSO—is similar to that in European countries or the United States, where a BMI cutoff of 30 kg/m2 is generally adopted. Consistent with this equivalence, the prevalence of certain types of obesity-related health disorders including type 2 diabetes and nonalcoholic steatohepatitis in Japan is similar to that in populations of European descent [7, 8].
Definition of Obesity Disease
JASSO defines obesity disease as obesity accompanied by obesity-induced or obesity-associated health disorders, or by a high probability of their development, and as a condition that from a medical viewpoint requires body weight reduction (Table 1). This concept of obesity disease, developed with the aim of selecting individuals who require medical care from among the large obese population, is unique from an international perspective, but seems logical and reasonable.
Obesity-related health disorders included in the diagnostic criteria for obesity disease are listed in Table 2. These 11 health disorders are triggered by or associated with obesity, and there is substantial evidence that weight reduction can alleviate their severity or reduce the risk of their development. In addition to these 11 conditions, other health disorders, also shown in Table 2, are known to be associated with obesity. However, these latter disorders are not included in the diagnostic criteria for obesity disease because current evidence in support of the benefits of weight reduction for them is not as strong as that for the 11 included health disorders. Obesity accompanied by any one of these 11 obesity-related health disorders is therefore diagnosed as obesity disease (Table 1).
Table 2
Obesity-related health disorders
| Obesity-related health disorders included in the diagnostic criteria for obesity disease |
| 1. Glucose intolerance (including type 2 diabetes and impaired glucose tolerance) |
| 2. Dyslipidemia |
| 3. Hypertension |
| 4. Hyperuricemia or gout |
| 5. Coronary artery disease |
| 6. Cerebral infarction or transient ischemic attack |
| 7. Nonalcoholic fatty liver disease (NAFLD) |
| 8. Menstrual abnormalities or female infertility |
| 9. Obstructive sleep apnea syndrome or obesity hypoventilation syndrome |
| 10. Musculoskeletal disorders (including osteoarthritis of knee, hip, or finger joints as well as spondylosis deformans) |
| 11. Obesity-related kidney disease |
| Obesity-related health disorders not included in the diagnostic criteria for obesity disease |
| 1. Malignant disease (including colorectal, esophageal, endometrial, pancreatic, renal, breast, and liver cancer) |
| 2. Cholelithiasis |
| 3. Venous thrombosis or pulmonary embolism |
| 4. Bronchial asthma |
| 5. Skin disorders (including acanthosis nigricans, frictional dermatitis, and others) |
| 6. Male infertility |
| 7. Gastroesophageal reflux disease |
| 8. Mental disorder |
Visceral Fat Obesity as an Alternative Criterion of Obesity Disease
Much evidence indicates the pathological relevance of exaggerated accumulation of visceral fat [15-17]. Visceral fat accumulation has thus been linked with health disorders including glucose intolerance, dyslipidemia, and hypertension [1, 18]. The amount of visceral fat, and its clinical marker waist circumference, declines more rapidly than does the amount of subcutaneous fat in response to diet or exercise therapy for weight reduction [16, 17, 19, 20], and a reduction in waist circumference is associated with a decrease in the number of cardiometabolic risk factors [21, 22]. Analysis of body fat distribution by abdominal computed tomography (CT) has shown that visceral fat obesity poses a higher risk for metabolic disorders and atherosclerotic cardiovascular disease than does subcutaneous fat obesity [23]. A study of subjects who underwent health checkups revealed that visceral fat area (VFA) was positively correlated with the number of cardiovascular risk factors, whereas subcutaneous fat area was not [24]. The same study also found that the mean number of risk factors exceeded one at a VFA of –100 cm2 in both males and females. Visceral fat obesity is therefore diagnosed when a VFA of ≥100 cm2 is confirmed by CT or other modalities. Individuals of East Asian ethnicity, including Japanese, tend to accumulate more visceral fat compared with those of European ancestry with a similar BMI [23, 25-27]. This difference may explain why Japanese or other East Asian individuals develop obesity-related health disorders at lower BMIs [10, 11].
It thus appears rational to target individuals with visceral fat obesity for medical treatment and to include this condition as a second category of obesity disease (Table 1). Measurement of waist circumference at the umbilical level is recommended as a screening tool for visceral fat obesity. The waist circumference equivalent to a VFA of 100 cm2 is –85 and –90 cm in adult Japanese men and women, respectively [28]. Given that females tend to have more subcutaneous fat than males, the waist circumference criterion for the same level of visceral fat accumulation is greater in females [1]. Consistent with JASSO’s emphasis on visceral fat obesity, a consensus statement by the International Atherosclerosis Society and International Chair on Cardiometabolic Risk also emphasizes the importance of waist circumference measurement, in addition to BMI, for assessment of cardiometabolic risk [17].
Classification of Obesity and Obesity Disease
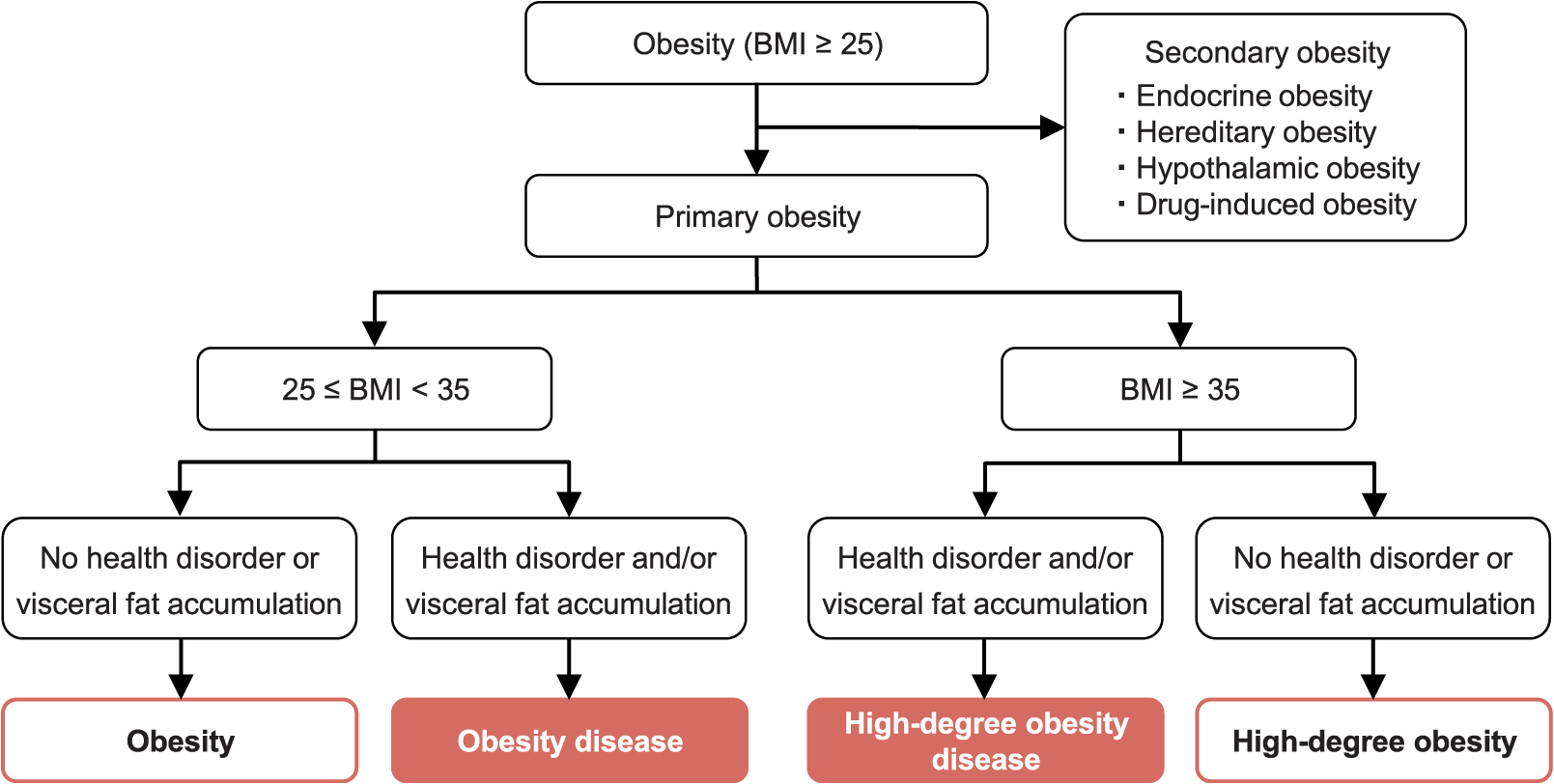
Fig. 2 shows a flowchart for the classification of obesity and obesity disease. Obese individuals (BMI of ≥25 kg/m2) should first be evaluated to determine whether obesity is secondary to another condition such as endocrinopathy, genetic disease, a hypothalamic disorder, or drug treatment. If a treatable factor responsible for obesity is identified, treatment for this factor should be prioritized.
High-Degree Obesity and High-Degree Obesity Disease
Whereas certain obesity-related health disorders can occur at a low BMI in individuals of Japanese ethnicity, others are typically associated with pronounced obesity. These latter health disorders include respiratory diseases such as obstructive sleep apnea syndrome and hypoventilation syndrome, heart failure, obesity-related kidney disease, venous thrombosis, musculoskeletal disorders such as osteoarthritis, and skin disorders such as acanthosis nigricans and intertrigo. The treatment strategy for obesity disease therefore differs depending on the degree of obesity. JASSO recommends that obesity be classified into two categories on the basis of its degree: BMI ≥ 35 kg/m2 or 25 ≤ BMI < 35 kg/m2 (Table 1). Obesity with a BMI of ≥35 kg/m2 is referred to as high-degree obesity, and, when it is associated with any of the 11 stipulated obesity-related health disorders or visceral fat accumulation, it is referred to as high-degree obesity disease (Fig. 2).
Treatment Guidance for Obesity Disease
Treatment guidance for obesity disease is outlined in Fig. 3. When obesity disease is not classified as high-degree obesity disease, an initial weight reduction goal of 3% or more should be set, with this recommendation being based on evidence that multiple obesity-related health disorders are improved by such a weight reduction [29]. For the treatment of high-degree obesity disease, the weight reduction goal depends on the associated health disorders, but the initial goal should generally be a loss of 5% to 10% of current body weight.
Implementation of a combination of dietary, exercise, and behavioral therapy has been shown to be effective for weight loss [30]. With regard to behavioral therapy, JASSO’s guidelines highlight exploitation of tools such as a graphed weight diary (Fig. 4) and food behavior diagram (Fig. 5) [1].


If the initial weight reduction goal is achieved, it is recommended that a new goal be set and the current treatment strategy be continued. If the initial weight reduction goal is not met, intensification of dietary therapy or the introduction of drug therapy (or both) may be necessary. For such intensification of dietary therapy, a very low calorie diet is an option for individuals with high-degree obesity disease. Pharmacological therapy should take into account the mode of action, effectiveness, and safety of the considered drug. Surgical treatment is indicated mostly for high-degree obesity disease, but it may also be appropriate for obesity disease with a BMI <35 kg/m2 depending on the accompanying health disorders. It is important to emphasize that weight reduction is not the end goal, but rather a means to treat obesity disease. Throughout the treatment process, it is crucial to evaluate the improvement in obesity-related health disorders in tandem with changes in body mass and waist circumference.
During interventions for weight reduction, it is also important to be aware of potential harmful effects associated with excessive weight loss, such as frailty in older adults. Japan has an exceptionally high aging rate, with approximately 28% and 15% of the population being 65 or 75 years of age or older, respectively [31]. The relation between obesity and health impairments varies with age [32, 33], necessitating specific treatment guidance for older adults. However, because of insufficient evidence, JASSO has yet to establish clear treatment guidelines for obesity disease in this age group. Mental disorders are among the health issues associated with obesity, and a substantial number of individuals with high-degree obesity have mental health concerns. It is therefore also important to include appropriate mental health evaluations and to provide necessary psychological support during the treatment of obesity disease.
Importance of Social Engagement and the Initiatives of JASSO
The ultimate goals of treatment for obesity disease, similar to those of treatment for other conditions, is to prevent early death, to prolong healthy life expectancy, and to preserve quality of life (QOL) (Fig. 6). The maintenance or improvement of QOL for individuals with obesity or obesity disease cannot be achieved solely by a medical approach, with an approach from a social perspective, including the resolution of stigma, also being important.

The development of obesity depends on various factors including genetic or epigenetic factors, factors related to growth and development, and socioeconomic factors. However, it is often overly attributed to an individual’s lifestyle. As a result, individuals with obesity often face prejudice that labels them as lacking the ability of self-management. In addition to such social stigma, personal stigma characterized by the perception that obesity is their own responsibility, often raises problems in the treatment of individuals with obesity disease. The inappropriate conclusion that obesity is solely a matter of self-control and thus not a subject for medical treatment deters individuals from receiving appropriate medical care.
One reason that obesity is often viewed as an individual issue is that treatment has long been limited to lifestyle modification. The recent proliferation of surgical treatments and the development of effective medicines should not only promote patient care but also help shift societal perceptions of obesity. The development of new treatments and the dissemination of knowledge about the pathogenesis and appropriate management of obesity and obesity disease—efforts that also contribute to elimination of obesity stigma—are key responsibilities of academic organizations engaged in obesity research. Given the wide array of health issues linked to obesity, a broad-ranging collaboration is crucial. In 2018, JASSO, together with 23 other Japanese academic societies, issued the Kobe Declaration, pledging to collaborate broadly on academic and social initiatives addressing obesity [34]. Since then, and within this framework, JASSO has been conducting activities to promote understanding of the concept of and appropriate treatment for obesity disease. These activities will also contribute to enhancement of QOL for individuals dealing with obesity or obesity disease.
Summary and Conclusion
We have here described the diagnostic criteria and core concepts for the treatment of obesity disease based on the guidelines of JASSO. The relation between obesity and health disorders varies according to ethnicity, likely as a result of many factors including genetic, geographical, and societal influences. It is therefore rational that the diagnostic criteria and treatment for obesity also vary depending on ethnicity. This concept is becoming more widely recognized among practitioners and researchers who specialize in obesity treatment, but not as much among those with other specialties. Given the diversity of health disorders caused by or associated with obesity, professionals in various medical fields should be aware of the ethnicity-dependent differences in the connection between obesity and its related health disorders.
Acknowledgments
We thank all the authors of Guidelines for the Management of Obesity Disease 2022 as well as Hitoshi Nishizawa for assistance with writing the draft of this paper.
Disclosure
Wataru Ogawa has received the following remuneration and financial assistance: lecture fees from Abbott Japan LLC., Nippon Boehringer Ingelheim Co., Ltd., Sumitomo Pharma Co., Ltd., and Novo Nordisk Pharma Ltd.; research expenses (including those for contracted research, joint research, and clinical trials) and grants from Abbott Diabetes Care UK Ltd., Eli Lilly Japan K.K., Nippon Boehringer Ingelheim Co., Ltd., Noster Inc., Teijin Pharma Ltd., and Sumitomo Pharma Co., Ltd.; scholarship donations from Kowa Company, Ltd., Novo Nordisk Pharma Ltd., Sumitomo Pharma Co., Ltd., Teijin Pharma Ltd.. and Takeda Pharmaceutical Co. Ltd. Yushi Hirota received the following remuneration and financial assistance: lecture fees from Eli Lilly Japan K.K. Sanofi, Terumo Corp., Sumitomo Pharma Co., Ltd., and Abbott Japan LLC.; research support from Sumitomo Pharma Co., Ltd., Kyowa Kirin Co., Ltd. and Medtronic Japan Co., Ltd. Shigeru Miyazaki received the following remuneration: lecture fees from Novo Nordisk Pharma Ltd. Yoshihiro Ogawa has received the following remuneration and financial assistance: lecture fees from Daiichi Sankyo Co., Ltd.; scholarship donations from Medical Corporation Saisei Mirai, and Federation of National Public Employees Mutual Aid Associations Sasebo Kyosai hospital. Iichiro Shimomura has received the following remuneration and financial assistance: lecture fees from Ono Pharmaceutical Co., Kowa Company, Ltd., Sumitomo Pharma Co., Eli Lilly Japan K.K, and Novo Nordisk Pharma Ltd.; research expenses (including those for contracted research, joint research, and clinical trials) and grants from Japan Agency for Medical Research and Development (AMED), Cancerscan Inc., Kubarahonke Co. Ltd., Kowa Company, Ltd., Kobayashi Pharmaceutical Co. Ltd., and Rohto Pharmaceutical Co. Ltd.; scholarship donations from Kowa Company, Ltd., Daiichi Sankyo Co., Sumitomo Pharma Co., Takeda Pharma K.K., Mitsubishi Tanabe Pharma Co., Teijin Pharma, Novo Nordisk Pharma Ltd., Mochida Pharmaceutical Co., Suzuken Memorial Foundation, Manpei Suzuki Diabetes Foundation, Midori Health Care Center, McSYL, and Hakuhokai Central Hospital. Toshimasa Yamauchi has received the following remuneration and financial assistance: lecture fees from Ono Pharmaceutical Co., Takeda Pharma K.K., MSD, Sumitomo Pharma Co., Teijin Healthcare Ltd, Nippon Boehringer Ingelheim Co., Ltd., Novo Nordisk Pharma Ltd.,; research expenses (including those for contracted research, joint research, and clinical trials) and grants from Kowa Company, Ltd., Minophagen Co., Nipro Co.,; scholarship donations from Novo Nordisk Pharma Ltd., Mitsubishi Tanabe Pharma Co., Kyowa Kirin Co., Ltd., Takeda Pharma K.K., Ono Pharmaceutical Co., Sumitomo Dainippon Pharma Co., Ltd.,; chairs courses endowed by Ono Pharmaceutical Co., Mitsubishi Tanabe Pharma Co., Novo Nordisk Pharma Ltd., Nippon Boehringer Ingelheim Co., Ltd., Kowa Company, Ltd., Nitto Boseki Co., Ltd. and Asahi Mutual Insurance Co. Koutaro Yokote has received the following remuneration and financial assistance: lecture fees from Astellas Pharma Inc., AstraZeneca, Daiichi Sankyo Co., Eli Lilly Japan K.K., Jansen Pharma K.K., Kowa Company, Ltd., Mitsubishi Tanabe Pharma Co., MSD, Ono Pharmaceutical Co., Sumitomo Pharma Co., Takeda Pharma K.K., Nippon Boehringer Ingelheim Co., Ltd., Novartis Pharma K.K., Novo Nordisk Pharma Ltd., Sanofi and Taisho Pharma Co., Ltd.; research expenses (including those for contracted research, joint research, and clinical trials) and grants from Taisho Pharma Co., Ltd.; scholarship donations from Astellas Pharma Inc., Bayer Yakuhin Ltd., Daiichi Sankyo Co., Kowa Company, Ltd., Mitsubishi Tanabe Pharma Co., MSD, Nippon Boehringer Ingelheim Co., Ltd., Novo Nordisk Pharma Ltd., Ono Pharmaceutical Co., Shionogi Pharma Co., Ltd., Sumitomo Pharma Co., Taisho Co., Ltd., Takeda Pharma K.K., and Teijin Pharma. All remaining authors declare no conflict of interest.
References
- 1 Matsuzawa Y, Inoue S, Ikeda Y, Sakata T, Saito Y, et al. (2000) Atarashii himan no hantei to himanshou no shindan kijun (New diagnostic criteria for obesity and obesity disease). Journal of Japan Society for the Study of Obesity 6: 18–28 (In Japanese).
- 2 Examination Committee of Criteria for ‘Obesity Disease’ in Japan; Japan Society for the Study of Obesity (2002) New criteria for ‘obesity disease’ in Japan. Circ J 66: 987–992.
- 3 Committee for Guidelines for the Treatment of Obesity Disease 2006 by Japan Society for the Study of Obesity (2006) Himanshou Chiryou Gaidorain 2006 (Guidelines for the treatment of Obesity Disease 2006). Journal of Japan Society for the Study of Obesity 12 (Extra Edition): 1–91 (In Japanese).
- 4 Japan Society for the Study of Obesity (2016) Guidelines for the management of obesity disease 2016. Life Science Publishing Company, Tokyo, Japan (In Japanese).
- 5 Japan Society for the Study of Obesity (2022) Guidelines for the Management of Obesity Disease 2022. Life Science Publishing Company, Tokyo, Japan (In Japanese).
- 6 World Health Organization (ed) (1998) Obesity: preventing and managing the global epidemic. Report of a WHO consultation on Obesity, Geneva 3–5 June 1997. World Health Organization, Geneva, Switzerland.
- 7 Kodama K, Tojjar D, Yamada S, Toda K, Patel CJ, et al. (2013) Ethnic differences in the relationship between insulin sensitivity and insulin response: a systematic review and meta-analysis. Diabetes Care 36: 1789–1796.
- 8 Shai I, Jiang R, Manson JE, Stampfer MJ, Willett WC, et al. (2006) Ethnicity, Obesity, and Risk of Type 2 Diabetes in Women. A 20-year follow-up study. Diabetes Care 29: 1585–1590.
- 9 Huxley R, James WP, Barzi F, Patel JV, Lear SA, et al. (2008) Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. Obes Rev 9 Suppl 1: 53–61.
- 10 Chiu M, Austin PC, Manuel DG, Shah BR, Tu JV (2011) Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diabetes Care 34: 1741–1748.
- 11 Azuma K, Kadowaki T, Cetinel C, Kadota A, El-Saed A, et al. (2009) Higher liver fat content among Japanese in Japan compared with non-Hispanic whites in the United States. Metabolism 58: 1200–1207.
- 12 NCD Risk Factor Collaboration (NCD-RisC) (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390: 2627–2642.
- 13 OECD (2017) Overweight and obesity among adults. In: Health at a Glance 2017. OECD Indicators, OECD Publishing, Paris, France. https://doi.org/10.1787/health_glance-2017-en accessed on August 12, 2023.
- 14 (2020) Ministry of Health, Labour and Welfare. National Health and Nutrition Survey Japan 2020. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/eiyou/r1-houkoku_00002.html accessed on August 12, 2023 (In Japanese).
- 15 González-Muniesa P, Mártinez-González MA, Hu FB, Després JP, Matsuzawa Y et al. (2017) Obesity. Nat Rev Dis Primers 3: 17034.
- 16 Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, et al. (2019) Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol 7: 715–725.
- 17 Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, et al. (2020) Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol 16: 177–189.
- 18 WHO expert consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363: 157–163.
- 19 Ryo M, Kishida K, Nakamura T, Funahashi T, Shimomura I (2014) Short-term intervention reduces bioelectrical impedance analysis-measured visceral fat in type 2 diabetes mellitus. Diabetes Res Clin Pract 103: e27–e29.
- 20 Chaston TB, Dixon JB (2008) Factors associated with percent change in visceral versus subcutaneous abdominal fat during weight loss: findings from a systematic review. Int J Obes (Lond) 32: 619–628.
- 21 Okauchi Y, Nishizawa H, Funahashi T, Ogawa T, Noguchi M, et al. (2007) Reduction of visceral fat is associated with decrease in the number of metabolic risk factors in Japanese men. Diabetes Care 30: 2392–2394.
- 22 Ryo M, Nakamura T, Funahashi T, Noguchi M, Kishida K, et al. (2011) Health education “Hokenshido” program reduced metabolic syndrome in the Amagasaki visceral fat study. Three-year follow-up study of 3,174 Japanese employees. Intern Med 50: 1643–1648.
- 23 Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S (1987) Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism 36: 54–59.
- 24 Hiuge-Shimizu A, Kishida K, Funahashi T, Ishizaka Y, Oka R, et al. (2012) Absolute value of visceral fat area measured on computed tomography scans and obesity-related cardiovascular risk factors in large-scale Japanese general population (the VACATION-J study). Ann Med 44: 82–92.
- 25 Katsuki A, Sumida Y, Urakawa H, Gabazza EC, Murashima S, et al. (2003) Increased visceral fat and serum levels of triglyceride are associated with insulin resistance in Japanese metabolically obese, normal weight subjects with normal glucose tolerance. Diabetes Care 26: 2341–2344.
- 26 Nazare JA, Smith JD, Borel AL, Haffner SM, Balkau B, et al. (2012) Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/Intra-Abdominal Adiposity. Am J Clin Nutr 96: 714–726.
- 27 Kadowaki T, Sekikawa A, Murata K, Maegawa H, Takamiya T, et al. (2006) Japanese men have larger areas of visceral adipose tissue than Caucasian men in the same levels of waist circumference in a population-based study. Int J Obes (Lond) 30: 1163–1165.
- 28 Committee to Evaluate Diagnostic Standards for Metabolic Syndrome (2005) Definition and the diagnostic standard for metabolic syndrome. Nihon Naika Gakkai Zasshi 94: 188–203 (In Japanese).
- 29 Muramoto A, Matsushita M, Kato A, Yamamoto N, Koike G, et al. (2014) Three percent weight reduction is the minimum requirement to improve health hazards in obese and overweight people in Japan. Obes Res Clin Pract 8: e466–e475.
- 30 Barrett S, Begg S, O’Halloran P, Kingsley M (2018) Integrated motivational interviewing and cognitive behaviour therapy for lifestyle mediators of overweight and obesity in community-dwelling adults: a systematic review and meta-analyses. BMC Public Health 18: 1160.
- 31 Cabinet Office (2021) Annual Report on the Aging Society: Summary FY2021. https://www8.cao.go.jp/kourei/english/annualreport/2021/pdf/2021.pdf accessed on October 3, 2023.
- 32 Ahmadi SF, Streja E, Zahmatkesh G, Streja D, Kashyap M, et al. (2015) Reverse epidemiology of traditional cardiovascular risk factors in the geriatric population. J Am Med Dir Assoc 16: 933–939.
- 33 Dramé M, Godaert L (2023) The obesity paradox and mortality in older adults: a systematic review. Nutrients 15: 1780.
- 34 Japan Society for the Study of Obesity, along with 23 other Japanese academic societies (2018) the Kobe declaration 2018. http://www.jasso.or.jp/data/data/pdf/kobe2018.pdf accessed on August 12, 2023 (In Japanese).
 https://orcid.org/0000-0002-0432-4366
https://orcid.org/0000-0002-0432-4366
 https://orcid.org/0000-0002-3035-4155
https://orcid.org/0000-0002-3035-4155
 https://orcid.org/0000-0002-0834-2836
https://orcid.org/0000-0002-0834-2836
 https://orcid.org/0000-0002-0851-9603
https://orcid.org/0000-0002-0851-9603
 https://orcid.org/0000-0003-4827-6404
https://orcid.org/0000-0003-4827-6404
 https://orcid.org/0000-0003-3033-4813
https://orcid.org/0000-0003-3033-4813