2013 Volume 55 Issue 4 Pages 267-275
2013 Volume 55 Issue 4 Pages 267-275
Objectives: Previous studies in firefighters have been contradictory regarding their course of lung function over time. The aim of this ongoing study is to investigate how changes in lung function over time in male metropolitan firefighters compare with those in population controls, and to explore associations between firefighters' use of personal respiratory protection devices during occupational exposures and their risk of accelerated lung function decline. Methods: A prospective comparison of FEV1 (forced expiratory volume in 1 second) and FVC (forced vital capacity) was performed between 281 firefighters and 933 population controls. Logistic regression models were used to compare changes from baseline of FEV1 and FVC after 3 years and risk of accelerated decline between the cohorts. Within the firefighter cohort, risk of accelerated decline was compared between subgroups based on use of respiratory protection devices. Results: Controls showed similar mean annual declines for FEV1 and FVC across age categories, whereas firefighters aged <45 years showed increasing values over time (p=0.040). Firefighters had a lower odds of accelerated FEV1 decline compared with controls (OR=0.60, 95%CI 110.44; 0.83), but firefighters who never or rarely used respiratory protection during fire knockdown had a higher odds of accelerated FEV1 decline compared with those who used it often or frequently (OR=2.20, 95%CI 1.02; 4.74). Conclusions: Younger generations of firefighters showed an increase in lung function relative to older colleagues, while population controls consistently showed decline of lung function across all ages. Firefighters who reported to be incompliant in using respiratory protection showed an increased risk of accelerated FEV1 decline.
(J Occup Health 2013; 55: 267-275)
Despite personal protection measures, firefighters may be at increased risk of adverse health effects due to exposure to smoke and other potentially harmful substances during their professional duties. In the past years, safeguarding firefighters' (respiratory) health has received increasing attention in Australia and elsewhere, from a research1) as well as governance2) point of view. Providing respiratory protection devices to firefighters has become standard policy in many fire departments around the world, although the devices may not always be optimally used3). The importance of assessing physical fitness and performance when monitoring firefighters' health and selecting new recruits has also increased4, 5).
Previous investigations have demonstrated that firefighters may show increased bronchial hyperresponsiveness and reduced lung function after occupational exposure3, 6-8). Studies looking at changes in firefighters' lung function over a prolonged period of time are scarce and have shown conflicting results, some indicating accelerated lung function decline9) whereas others did not10-12).
Only two previous studies have compared course of lung function between firefighters and general population controls13, 14). Because both these studies were conducted well over fifteen years ago and firefighters' working conditions have changed considerably during the past decades, their applicability to present-day generations of firefighters is likely to be limited.
The aim of the study reported in this paper was therefore to explore how changes in lung function over time in male metropolitan firefighters compare with those in male general population controls. In addition, we studied associations between firefighters' use of personal respiratory protection devices during occupational exposures and their risk of accelerated lung function decline.
The study was a prospective comparison between two existing cohorts of study subjects, i.e., a cohort of South Australian male metropolitan firefighters15) and a reference cohort of South Australian males randomly selected from the general population16).
Data collection for the ongoing South Australian Metropolitan Fire Service (SAMFS) study commenced in August 2007 and was completed in April 2011. At the start of the study, the SAMFS maintained staff that included 729 full-time and 226 retained firefighters, all but one (99.6%) Caucasians. At baseline, 56% (n=539) of the male staff volunteered to be tested for the study, and 281 (52%) of them could be reassessed for Stage 2 (Fig. 1). In reality, the retained firefighters are in country locations and are difficult to access. The participation rate amongst the metropolitan firefighters was about 74%.
Males from the North West Adelaide Health Study (NWAHS)17) served as population controls for the comparison of the firefighters' course of lung function over time. The NWAHS is an ongoing longitudinal cohort study in 4,060 randomly selected adults, among them 1,988 males. For the current study, we used Stage 1 and Stage 2 NWAHS data (collected between February 2000 and June 2003, and between May 2004 and February 2006, respectively). Details of sampling, recruitment and measurement procedures used in the NWAHS study can be found elsewhere16, 17). Figure 1 shows the recruitment and follow-up for the NWAHS study and the selection for the comparison with the firefighters. A total of 933 (70%) NWAHS male subjects (95.5% Caucasians) could be reassessed for Stage 2 of the study.
The NWAHS was funded by the University of Adelaide Faculty of Medicine and the Human Services Research Initiatives Projects of the SA Department of Health. Approval for the NWAHS was obtained from the Ethics Committees of the North West Adelaide Health Service, the University of Adelaide and the University of South Australia. The current analysis was funded by the SAMFS and the University of Adelaide and received ethics approval from the University of Adelaide Human Research Ethics Committee (H-057-2007). All study participants gave their informed consent.
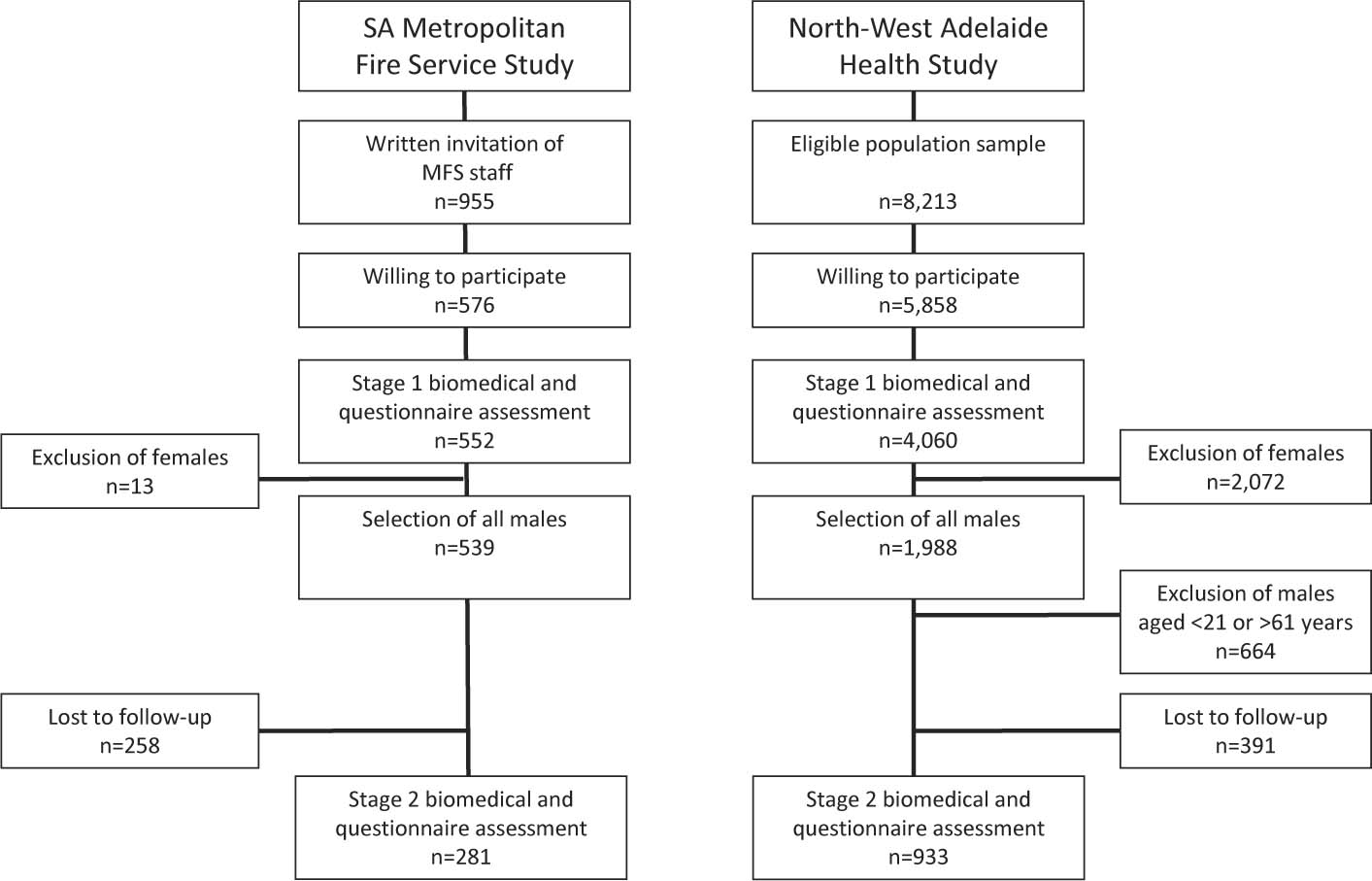
Participant recruitment and follow-up in the MFS firefighters and NWAHS* population control cohorts
*Details of recruitment for the NWAHS cohort taken from the paper of Grant et al.17).
†Age range in the firefighter cohort. MFS: Metropolitan Fire Service. NWAHS: North West Adelaide Health Study.
Change in FEV1 (forced expiratory volume in one second) over time served as the primary outcome for the comparison between the firefighters and general population controls. Change in FVC (forced vital capacity) was studied as a secondary outcome. Spirometry in the firefighters was performed using a MasterScreen® spirometer (Viasys Healthcare/Cardinal Health, Würzburg, Germany) following 2005 recommendations for spirometry18). Spirometry in the NWAHS was performed using a MicroLab® 2000 spirometer (Micro Medical/Cardinal Health, Dublin, OH, USA) following 1987 recommendations19). Reference lung function values from healthy Australian adult lifetime nonsmokers without adverse bronchial symptoms were used to calculate percentage predicted values20).
Information regarding smoking and doctor-diagnosed respiratory and other medical conditions was ascertained by questionnaire in both cohorts. Additionally, in the firefighter cohort, we assessed occupational exposures and use of personal respiratory protection devices using a questionnaire, in which the firefighters reported if and how frequently they had been involved in common firefighting tasks (i.e., knockdown, overhaul, fire investigation, hazmat investigation) in the last 12 months. We also inquired how often the firefighters had worn respiratory protection during these tasks in that same period (never, rarely (i.e., less than 40% of the time), some of the time (40 to 60%), often (60 to 80%), frequently (80 to 100%), respectively). The SAMFS has been using various types of compressed air/decant systems since the early 1970s. From 1997 until present (so during the observation period of the current study), the SAMFS has used AirMaxx self-contained breathing apparatus systems (MSA Auer, Berlin, Germany) for respiratory protection of their firefighters.
Statistical analysisData were analyzed using SPSS®, version 19.0.0 (SPSS Inc., Chicago, IL, USA). The Student's t-test and χ2 test were used to compare baseline characteristics between the subjects in the longitudinal analyses and those who dropped out. Change in body weight (kg/year) was compared between firefighters and controls using the median test. Study subjects were categorized into six age categories based on their baseline age: <35, 36-40, 41-45, 46-50, 51-55 and 56-62 years. In order to incorporate the “clinical relevance” of change in FEV1 over time in our study subjects, accelerated FEV1 decline was defined as >0.050 l/year, which is the average annual FEV1 decline for Australian males who are current heavy smokers21).
A GLM repeated measures model containing study stage (i.e., baseline or follow-up measurement), cohort (MFS or NWAHS), age category and their two and three way interaction terms was used to analyze differences between changes in FEV1 in firefighters and population controls over time. History of chronic respiratory disease and change in body weight between baseline and follow-up measurement22) were added to the model as potential confounders. Because of the small number of current smokers in the firefighter cohort (n=26) and the well-known effect of smoking in causing accelerated FEV1 decline23), this analysis was limited to the nonsmokers in the firefighter cohort as well as in the NWAHS population control cohort.
A logistic regression model, again with interaction terms, was used to compare the odds of accelerated FEV1 decline between firefighters and controls. Within the firefighter cohort, the odds of accelerated FEV1 decline was compared between subgroups based on self-reported use of respiratory protection during knockdown. The logistic regression model included use of respiratory protection (never or rarely, some of the times, often or frequently), baseline smoking status (current smoker, current nonsmoker), age category (<45 years; ≥46 years), and weight change (in kg/year). Again, because of the small number of smokers, interaction between use of respiratory protection and smoking status was not included in the model. In all analyses, statistical significance was defined as p<0.05. Ninety-five percent confidence intervals (95%CIs) were calculated when appropriate.
Average duration of follow-up was 2.9 (SD 0.3) years for the firefighters and 3.5 (SD 1.1) years for the controls. Table 1 shows characteristics for the firefighters and the NWAHS controls who entered the longitudinal analysis and for those lost to follow-up. In both cohorts, baseline FEV1 and FVC and their % predicted values were higher in subjects who entered the longitudinal analyses compared with those who were lost to follow-up. In the NWAHS cohort, subjects who were current smokers were more likely to be lost to follow-up.
| Firefighters | NWAHS controls | |||||
|---|---|---|---|---|---|---|
| In longitudinal analysis (n=281) | Lost to follow-up (n=258) | p value | In longitudinal analysis (n=933) | Lost to follow-up (n=379) | p value | |
| Age (years) | 43.3 (8.0) | 43.8 (9.0) | 0.938† | 42.7 (9.8) | 44.5 (13.2) | 0.017† |
| Height (m) | 1.81 (0.06) | 1.79 (0.06) | 0.022† | 1.77 (0.07) | 1.75 (0.07) | <0.001† |
| Weight (kg) | 89.4 (11.4) | 89.3 (10.9) | 0.752† | 88.0 (16.2) | 85.3 (16.9) | 0.009† |
| Body mass index | ||||||
| <25 kg/m2, n(%) | 66 (24) | 51 (20) | 242 (26) | 120 (31) | ||
| 25-30 kg/m2, n(%) | 169 (60) | 159 (62) | 432 (46) | 152 (40) | ||
| ≥30 kg/m2, n (%) | 46 (16) | 48 (19) | 0.794$ | 267 (28) | 111 (29) | 0.061$ |
| Smoking status, n (%)‡ | ||||||
| Current smokers | 26 (9) | 28 (11) | 254 (27) | 134 (35) | ||
| Former smokers | 64 (23) | 70 (27) | 284 (31) | 108 (28) | ||
| Never smokers | 190 (68) | 160 (62) | 0.629$ | 394 (42) | 141 (37) | 0.017$ |
| History of asthma, n (%) | 37 (13) | 30 (12) | 0.569$ | 126 (14) | 53 (14) | 0.816$ |
| History of chronic bronchitis/emphysema, n (%) | 16 (6) | 13 (5) | 0.873$ | 250 (27) | 98 (26) | 0.724$ |
| FEV1* (liters) | 4.51 (0.66) | 4.27 (0.68) | <0.001† | 3.72 (0.70) | 3.52 (0.76) | <0.001† |
| As % predicted | 104.9 (11.8) | 101.3 (12.0) | <0.001† | 90.1 (13.6) | 87.9 (13.8) | 0.007† |
| FVC* (liters) | 6.02 (0.82) | 5.71 (0.82) | <0.001† | 4.57 (0.81) | 4.32 (0.88) | <0.001† |
| As % predicted | 111.3 (11.4) | 108.2 (11.4) | 0.001† | 89.2 (12.3) | 87.0 (12.7) | 0.005† |
*Prebronchodilator values. †Student's t-test. $Chi-square test. ‡Baseline smoking status was missing for 1 firefighter and 1 NWAHS control in the longitudinal analysis. FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; NWAHS, North West Adelaide Health Study.
Baseline rate of current smoking in the firefighter cohort was about a third of the rate in the reference cohort (10% vs. 27%; χ2 test: p<0.001), while the rate of lifelong nonsmoking among the firefighters exceeded the rate among controls by 24% (Table 1). At follow-up, 10 firefighters (38% of all baseline smokers in their cohort) and 51 controls (20% of baseline smokers) reported that they quit smoking (χ2 test: p<0.001). In contrast, 3 firefighters (1.1% of baseline nonsmokers) and 28 controls (4.2%) reported to either have taken up or relapsed into smoking. The firefighters' weights increased by a median of 0.65 (interquartile range 1.50) kg/year, and the controls' weights increased by a median of 0.38 (1.68) kg/year (median test: p=0.087). Firefighters did not show a lower rate of doctor-confirmed asthma compared with controls (Table 1), but the rate of doctor-confirmed chronic bronchitis/emphysema was significantly higher among controls (6% vs. 27%; χ2 test: p<0.001).
Change in lung function in firefighters and controlsPopulation controls showed very similar mean annual declines for FEV1 and FVC in all age categories (Fig. 2). Overall, the younger generations of firefighters (i.e., those <45 years) showed an increase in their average FEV1 and FVC values over time, while their colleagues from older generations either showed no change or a decline (Fig. 2). The repeated measures analysis showed that the difference in the annual change in FEV1 between the younger and older age categories differed between the firefighters and controls (interaction term stage cohort age category: p=0.040).
A total of 72 (26%) firefighters and 363 (39%) controls showed accelerated FEV1 decline (i.e., >0.050 l/year) during the observation period. Logistic regression analysis controlling for age, baseline smoking status and history of chronic respiratory conditions showed that firefighters had a lower odds of accelerated FEV1 decline compared with population controls (OR=0.60, 95%CI 0.44 to 0.83; p=0.002).

Annual change in FEV1 (panel A) and FVC (panel B) by age category for nonsmoking firefighters (n=254) and population controls (n=678). Error bars indicate standard errors of the mean
FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity. * For interaction term cohort age category in relation to change in FEV1 over time.
At baseline, 78% of the firefighters had been on the job for >6 years. Of all the firefighters in the cohort, 80% reported involvement in fire knockdown in the past twelve months. On average, firefighters who had not been involved in knockdown were about five years older (47.2 (SD 7.0) years versus 42.5 (SD 8.0) years; Student's t-test: p<0.001) than the ones that had been involved, were more often current or former smokers (46% vs. 29%; χ2 test: p=0.027) and were more likely to have a history of chronic respiratory disease (24% vs. 13%; χ2 test: p=0.039).
Firefighters involved in knockdown who reported never or rarely using their respiratory protection during that task (n=50) were also more likely not to wear protection during other tasks that involve exposure to smoke or other potentially harmful substances (i.e., during overhaul, 87%, χ2 test, p<0.001; during fire investigation, 73%, χ2 test, p=0.063). Never or rarely using respiratory protection during fire knockdown was more common in older firefighters than in younger firefighters (12% in those aged ≤40 years, 27% in those aged 41 to 50 years and 40% in those aged >51 years (χ2 test: p=0.039)).
Figure 3 shows the annual change in lung function for the firefighters in relation to their involvement in knockdown and, if applicable, self-reported use of respiratory protection during knockdown. Logistic regression analysis controlling for smoking status, age and history of chronic respiratory disease showed that firefighters who reported never or rarely using their respiratory protection during fire knockdown had a higher odds of accelerated FEV1 decline compared with those who used it often or frequently (OR=2.20, 95%CI 1.02 to 4.74; p=0.044). Firefighters who wore their respiratory protection some of the time seemed to have a higher odds of accelerated FEV1 decline, but this was not statistically significant (OR=1.71, 95%CI 0.69 to 4.24; p=0.248). The interaction term between age category and frequency of using respiratory protection devices during knockdown in relation to change in FEV1 came close to statistical significance (OR=1.96, 95%CI 0.91 to 4.22; p=0.086). The logistic regression model also showed that the odds of accelerated FEV1 decline in firefighters who were current smokers was 4.59 (95%CI 1.71 to 12.33) compared with their nonsmoking colleagues.
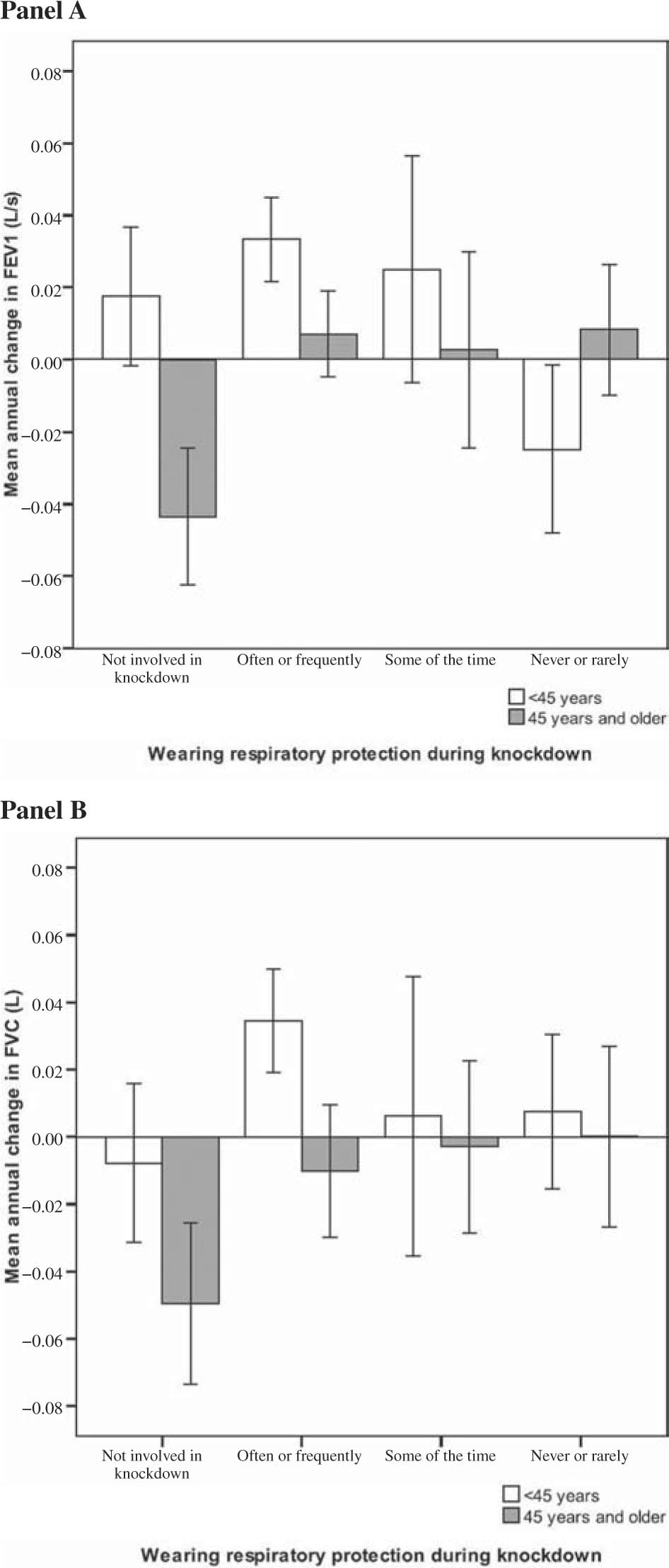
Annual change in FEV1 (panel A) and FVC (panel B) by age group and use of respiratory protection devices during knockdown in male firefighters (n=281). Error bars indicate standard errors of the mean
FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.
In this study, we assessed the course of lung function in male metropolitan firefighters over a three-year time period and compared this with males from a general population cohort. We found that younger generations of firefighters showed an increase in their FEV1 and FVC values relative to older generations of firefighters, while the population controls consistently showed decline in FEV1 as well as FVC across all ages. Firefighters had a lower risk of accelerated FEV1 decline compared with population controls. Within the firefighter cohort, smokers and those who reported not or only occasionally using their respiratory protection devices during fire knockdown showed an increased risk of accelerated FEV1 decline compared with those who used their respiratory protection more consistently.
Comparison with existing literatureAnalysis of the baseline data of our firefighter cohort showed that those with the highest rate of self-reported exposure to dust, smoke and fire showed statistically significant lower FEV1, FEV1 % predicted and FVC values compared with colleagues who reported being less exposed to these factors15). It has previously been shown that firefighters may be at increased risk of accelerated lung function decline, depending on their actual exposure to inhaled harmful substances during their professional duties13, 24, 25). Rapid decline of lung function over time has been reported in a study in Baltimore City firefighters9) and in firefighters who presented for pulmonary evaluation after having been involved in the rescue work at the World Trade Center (WTC) disaster26). On the other hand, a follow-up study conducted in England showed that, as a group, male firefighters showed a lower rate of lung function decline over time than control subjects did14). Our comparison between firefighters and NWAHS general population controls supports the latter finding and adds that this phenomenon may be mainly attributable to an increase in lung function over time in younger (i.e., <45 years) firefighters rather than a decelerated rate of decline across all age groups. Although there is a body of literature showing that the respiratory system undergoes various anatomical and physiological changes with age and that after 20-25 years of age, aging is associated with progressive decline in lung function27, 28), this may be different for firefighters. Possible explanations for this are the selection of healthy and very fit men for service (“healthy worker effect”)29, 30), the regular use of self-contained breathing apparatus systems14), the strenuous physical demands that come with the job or a combination of these (and other) factors. Moreover, firefighters are likely to realize that physical training and looking after their (respiratory) health are a year-round commitment if they are to successfully meet the demands of their job31)—which seems to be reflected in the low smoking rate (∼10%) in our firefighter cohort. Confirmation of our findings in another cohort of firefighters and/or comparison with other males selected based on their physical fitness (for instance, soldiers) who can be matched to firefighters is necessary. To further study the role of self-contained breathing apparatus systems as a possible explanation of our findings, a comparison with professional divers could be made. But even by matching to more suitable controls, in the case of firefighters the physical fitness and activity cannot be “isolated” from the other potential explanations for the unexpected increase in lung function (e.g., frequent use of breathing apparatus and performing strenuous physical activity while using this equipment).
Our observation that a more frequent use of respiratory protection devices during fire knockdown and other potentially harmful tasks may prevent firefighters from having accelerated lung function decline is consistent with a report from the previously mentioned study in Baltimore firefighters, in which a correlation between the use of protective devices and rate of FEV1 decline was found9). In contrast, analyses of longitudinal spirometry data of WTC rescue workers did not show an association between respirator use and FEV1 or FVC decline32), which may be explained by the typical, very intense and enduring inhalation exposure of the rescue workers in the aftermath of the disaster33) and the variety of respirator devices that were used32). Another interesting finding in our study was that the subgroup of older (>45 year) firefighters who had not actively been involved in fire knockdown in the past year showed the fastest rate of lung function decline, which may indicate that they were exempted from the heavier physical tasks and/or protected against inhaled exposures due to impaired respiratory health.
Strengths and limitationsTwo particular strengths of this study are the sizes of the firefighter and population control cohorts and the considerable follow-up time (∼3 years) for both cohorts. Apart from the ongoing monitoring of WTC rescue workers26, 34), longitudinal studies in well-defined cohorts of firefighters like ours are rather scarce. At baseline, some selection may have occurred when recruiting firefighters for the study, as firefighters who suspected that their respiratory health could be compromised (for instance, as a consequence of smoking habits or awareness of limited physical fitness) may have been less likely to volunteer for the study. This may have caused some selection bias towards better general and respiratory health in the firefighter cohort.
The observed increase in lung function in the younger firefighters does at least suggest that strenuous physical activity can improve lung function over time, as it is likely that as a group firefighters perform more-and more frequent-strenuous activities and are more physically fit than age-matched population controls. Unfortunately, in the current study, we had no further documentation from standardized exercise testing, activity monitoring or otherwise about the firefighters' and controls' levels of physical fitness or physical activity.
Another limitation is the fact that we only had results of two spirometry tests at our disposal, whereas more frequent measurements would have enabled us to get more precise estimates of lung function changes in both cohorts35). However, the limited precision applies to the measurements in firefighters as well as in controls and therefore cannot explain the observed differences between the two groups. Spirometry in the North West Adelaide Health Study was performed using less strict criteria for judging acceptability and repeatability of forced blows19) compared with the SAMFS firefighter study18). Although this difference in measurement procedures may have contributed to the observed differences in lung function indices in the two cohorts, it is rather unlikely that this factor can fully explain the substantial difference in FEV1 and FVC changes over time between the firefighters and population controls.
Our data about involvement in firefighter tasks and exposures to potentially harmful substances was limited to firefighters' self-reports only. Clearly, we would have preferred to have more comprehensive information regarding length of time spent in exposed jobs, number of responses and actual use of respiratory protection devices at our disposal, but in the current study, it was not feasible to collect this kind of data.
In this exploratory study, we observed an increase in lung function over time in younger generations of firefighters relative to older generations of firefighters, while general population controls consistently showed decline of lung function across all age groups. Overall, firefighters had a lower risk of accelerated FEV1 decline compared with population controls. These observations need to be verified in further studies with suitable age-matched controls. Within the firefighter cohort, smokers and those who reported not or only occasionally using their respiratory protection devices showed an increased risk of accelerated FEV1 decline compared with those who used their respiratory protection more consistently. This study supports improvement in the use of respiratory protection devices by firefighters, as well as monitoring firefighters' (respiratory) health over time.
Acknowledgments: Acknowledgment is made of the generosity of the South Australian Metropolitan Fire Service (SAMFS) firefighters and North West Adelaide Health Study (NWAHS) participants in the giving of their time and effort and of the contribution to the study by the SAMFS staff and the NWAHS research clinic and recruiting staff. Sarah Appleton is acknowledged for providing the authors access to the NWAHS data. The authors very much appreciate the preparatory work for the study performed by Guillaume Dujardin and Christine Holton, the statistical advice provided by Michelle Lorimer and the support in data entry and processing provided by Daniel Blakeley.
Conflict of interest: The authors declare that they have no conflict of interest.