2015 Volume 57 Issue 1 Pages 69-80
2015 Volume 57 Issue 1 Pages 69-80
Objectives: The aim of this study was to investigate workplace violence by patients or their relatives towards health-care workers in Congolese hospitals. Methods: Through the autumn of 2012, a cross-sectional survey on workplace violence was conducted in a sample of 2,210 registered health-care workers (989 males and 1,221 females, aged 33 ± 8 years) from 436 hospitals located in the province of Katanga, Democratic Republic of the Congo. Verbal aggression, harassment and physical violence perpetrated by patients or their relatives within the previous year along with factors contributing to violence, were recorded, and the response rate was 99%. Results: About 80.1% of the health-care workers had experienced one or more types of workplace violence. Overall, the severity of workplace violence varied from verbal aggression (57.4%) and harassment (15.2%) to physical violence (7.5%). Patients were the major perpetrators of verbal aggression and harassment, whereas patients' relatives were mainly involved in physical violence. The frequency of workplace violence was similar across hospitals. Male health-care workers were more likely to be victims of physical violence, whereas female health-care workers were the prime target for harassment. Only 34.3% of the violent episodes were reported to a supervisor. Furthermore, disrespect for medical deontology was the main cause of workplace violence perceived by 68.8% of the health-care workers. Conclusions: Although it has not been officially recognized, there has been workplace violence towards health-care workers perpetrated by patients or their relatives despite the fact that health-care workers have traditionally been highly respected in Congolese society. Further studies on this issue may suggest opportunities for combating violence in Congolese hospitals.
(J Occup Health 2015; 57: 69–80)
Workplace violence (WPV) is on the increase in both high- and low-income countries. WPV is a matter of particular interest, and it remains a major and widespread issue of public concern among workers1, 2). Although there is no agreement on the definition of WPV, for the International Labor Organization (ILO), WPV refers to “incidents where staff are abused, threatened or assaulted in circumstances related to their work”3). WPV is associated with several negative outcomes that may lead to absenteeism or work inefficiency4, 5) or to homicide6). Since WPV is still a common crime, there is a need for adequate preventive measures7).
The true prevalence of WPV is unknown; however, many professionals in the health-care sector are known to be at high risk of becoming victims of violence in their own workplaces4, 8). Health-care workers (HCWs) in emergency departments and those caring for psychiatric patients have been reported to be highly exposed to violence from patients9). The HCWs in other departments, such as surgery, however, are not immune to a high risk of harassment or aggression in the workplace10). Although providing health care is regarded as a noble service, and the negative impact of violence on the delivery of the health-care service is a well-known phenomenon, violence in the health-care sector is on the increase worldwide, and the trend is likely to continue in the coming years11).
Due to the rapid spread of workplace violence in the health-care sector and its negative consequences, an increasing number of researchers have been trying to identify the determinants of workplace violence and those workers at high risk, underscoring the need for interventional programs4, 12). Previous studies have demonstrated that the consequences may affect the life and career of the workers. Stress, deterioration in the quality of the services provided, absenteeism or abandonment of work are among the consequences of WPV in the health-care sector13, 14). Consequently, the abandonment of work by HCWs contributes to the shortage of HCWs that most countries are facing. For example, Sub-Saharan Africa has only 2% of the world's health-care workforce with 25% of its disease burden15, 16).
The Democratic Republic of the Congo (DRC) is not an exception with regard to the shortage of HCWs. Government spending on health has declined for decades and the health-care system has almost collapsed17). Human resources for health-care have been known to be insufficient for a long time, and a great number of available domestic HCWs are migrating to other countries. In this context, violence towards HCWs might have contributed to a reduction in the already-strained domestic resource of HCWs. As there is no published information available on WPV towards HCWs in the DRC, scientific interest in this problem could be an important public health exercise vital for tackling this issue. The relevance of this study in occupational health is that it provides evidence that WPV does exist in Congolese health-care facilities and calls for strong preventive measures and managerial social support for victims. As WPV in Congolese health-care facilities has not yet been investigated, this study was designed to scrutinize the magnitude and types of WPV and factors contributing to WPV towards HCWs in the Congolese economic, political and cultural contexts.
Study design: In the autumn of 2012, we carried out a cross-sectional retrospective survey in which physical violence, verbal aggression and harassment were investigated among HCWs.
Setting: Congolese health-care facilities (n=436) such as general hospitals, clinics, community health centers and dispensaries located in Katanga Province, an area mostly unaffected by the current armed conflict in the DRC. Located in the southeast region of the DRC, Katanga Province is the Congo's second largest province (496,977 km2), and the mining capital of the DRC. In 2010, Katanga Province was inhabited by approximately 5,608,683 people. Although Katanga is a province of prosperous mining activities, the local living standard is low18).
Participants and data collectionAt baseline, 2,233 potential participants (receptionists, nurses, laboratory technicians, radiology technicians, doctors, pharmacists, physical therapists and administrative personnel) were contacted through their supervisors. To reach all 436 health-care facilities, 72 investigators were involved in data collection. Being a registered HCW at one of the participating health-care facilities and being present during the survey were the inclusion criteria; on the other hand, supervisors, medical students in training and nursing students in training were excluded from this study. Before signing an informed consent form, the HCWs received a detailed explanation of the study. They were instructed to fill out a questionnaire and return it to investigators within a month. The questionnaire was conceived by our research team and was informed by the guidelines for assessing WPV in the health sector jointly released in 2003 by the International Labour Office/International Council of Nurses/World Health Organization/Public Service International13). The questionnaire had three parts: In the first part, the questionnaire covered the demographic characteristics of the participants (gender, age, marital status, work experience, having children or not, and occupation), and the type of setting. In the second part, we assessed the experiences of violence and harassment perpetrated by patients and/or their relatives towards HCWs within the last 12 months, whether the incidents had been reported, and if not, the reasons for not reporting them. The HCWs were also asked to report frequency of aggressive behavior, the reactions of victims and the person who provided social support, if any. The last part of the questionnaire specifically addressed perceived reasons for WPV and possible solutions in a blank description space. As shown in Fig. 1, there were 2,211 questionnaires returned (response rate: 99%); one questionnaire was excluded from our analysis because of missing data.

Flow chart of the study population.
The study followed the Helsinki Declaration and was approved by the Research Ethics Committee of the University of Lubumbashi.
Measurements of WPVFor the purpose of this study, the definition of WPV was modified from the ILO's definition3). WPV was defined as “incidents where staff are abused, threatened or assaulted in circumstances related to their work by an individual other than coworkers”. We used this definition excluding coworkers to facilitate the survey, as there might be an administrative barrier to the investigation of violence committed by coworkers in a country with extensive human rights abuses19).
Victims were defined as anyone reporting a positive answer to at least one of the following 11 questions:
In this study, the terms “aggression” and “violence” are synonymous. “Physical violence” includes any type of physical assault such as slapping, hitting, pinning, biting, confinement, hair-pulling, scratching, kicking, pushing, choking, grabbing and assault or threat with dangerous objects such as knives. Verbal aggression referred to insults, yelling or swearing directed at staff, using harmful words, name calling with intention to hurt, and the use of mistrustful words4). Another category of aggression used in the questionnaire was harassment, which was defined as making a persistent demand of a sexual nature, and it also included telephone calls, messages or any other correspondence that could cause a nuisance20). These definitions were briefly explained to the HCWs in a local language by investigators directly or through their supervisors.
The following questions were asked to assess perceived reasons for WPV:
The gathered answers from the HCWs regarding perceived reasons for WPV were reviewed by authors and classified in one of the following six categories:
We used the Stata 10 software (StataCorp LP, College Station, TX, USA), and p<0.05 was considered significant. The results of quantitative variables are presented as the mean ± standard deviation of the mean or as frequencies and percentages. The Chi-squared test was applied to evaluate differences in categorical variables, while the Student's t-test and nonparametric Mann-Whitney test were used to evaluate differences among continuous variables. Odds ratios and 95% confidence intervals were calculated using logistic regression analysis in order to determine predictors of aggressive behaviors.
Table 1 shows the demographics of the enrolled HCWs. The majority of the HCWs were married (63.5%). The mean age of the HCWs was 33 ± 8 years, with men being older than women (34 ± 8 vs. 32.5 ± 8, p<0.001, Student's t-test). Most of the HCWs were nurses (58%), 35% of them being men. Sixty-two percent of the HCWs had less than 5 years of work experience. HCWs in both the public and private sectors participated in this study, with 19.8 and 80.2% of the HCWs in the public and private sector, respectively. HCWs from the public health-care facilities had significantly less work experience (8 vs. 5 years, Mann-Whitney test, p<0.001) as compared with those in the private sector. The majority of the HCWs (62.1%) worked in Community Health Centers, whereas others (37.9%) were serving in hospitals, clinics and dispensaries.
| Variable | N | % | |
|---|---|---|---|
| Gender | Men | 989 | 44.75 |
| Women | 1,221 | 55.25 | |
| Age (years) | 18–19 | 5 | 0.23 |
| 20–29 | 838 | 37.92 | |
| 30–39 | 934 | 42.26 | |
| 40–49 | 328 | 14.84 | |
| 50–59 | 80 | 3.62 | |
| 60–68 | 25 | 1.13 | |
| Employer | Public | 438 | 19.82 |
| Private | 1,772 | 80.18 | |
| Workplace | Hospital | 270 | 12.22 |
| Clinic | 415 | 18.79 | |
| Community health center | 1,371 | 62.06 | |
| Dispensary | 153 | 6.92 | |
| Profession | Receptionists | 216 | 9.91 |
| Nurses | 1,267 | 58.15 | |
| Laboratory technicians | 264 | 12.12 | |
| Radiology technicians | 31 | 1.42 | |
| Doctors | 271 | 12.44 | |
| Pharmacists | 76 | 3.49 | |
| Physical therapists | 11 | 0.50 | |
| Administrators | 43 | 1.97 | |
| Marital status | Married | 1,403 | 63.48 |
| Single | 706 | 31.95 | |
| Divorced | 49 | 2.22 | |
| Widower/widow | 52 | 2.35 | |
| Have children | Yes | 1,496 | 67.72 |
| No | 709 | 32.10 | |
| No answer | 4 | 0.18 | |
| Work experience (years) | 0–5 | 1,357 | 61.46 |
| 6–10 | 540 | 24.46 | |
| 11–15 | 173 | 7.84 | |
| 16–45 | 138 | 6.25 |
Approximately 80.1% (1,770/2,210) of the HCWs had experienced one or more instances of aggressive behavior in the preceding year, and only 19.9% (440/2,210) of the HCWs were not affected. Out of 1,770 HCWs who experienced instances of aggressive behavior, 24.9% (440/1,770) of the HCWs experienced it once, while 63.6% (1,125/1,770) experienced instances of aggressive behavior more than two times (from two to thirty times); the data were missing for 11.5% of the HCWs (205/1,770).
Perpetrators, frequencies and types of aggressive behaviorsNearly half of the HCWs (41%) reported having been victims of violence by patients. Nearly 28 and 31% reported having been victims of violence by someone responsible for a patient at the hospital or a patient's relative, respectively (Fig. 1).
As shown in Fig. 2, HCWs were victims of various aggressive behaviors. The fraction of HCWs experiencing verbal aggression alone (1,086/1,573; 69.1%) was the greatest, followed by harassment alone (190/1,573; 12.1%) and physical violence alone (109/1,573; 6.9%). Approximately 11.9% of the HCWs experienced a combination of aggressive behaviors. Three hundred thirty-five (15.2%) HCWs reported having been victims of harassment and 63.6% (213/335) of these HCWs were women reporting sexually oriented harassment. When comparing aggressive behaviors in the workplace, we found that the frequencies of verbal aggression, harassment and physical aggression were similar at all types of health-care facilities. When scrutinizing aggressive behaviors in relation to working experience, we found a higher frequency of physical violence among health-care professionals with less than 5 years of work experience (Table 2). Patients were the major perpetrators of verbal aggression and harassment, whereas patients' relatives were mainly responsible for physical violence. There was no significant difference in aggressive behaviors between professions. However, nurses were more likely to be victims of verbal aggression (749/1,269; 59.0%), physical violence (89/166; 53.6%) and harassment (212/335; 63.3%) (Table 2).
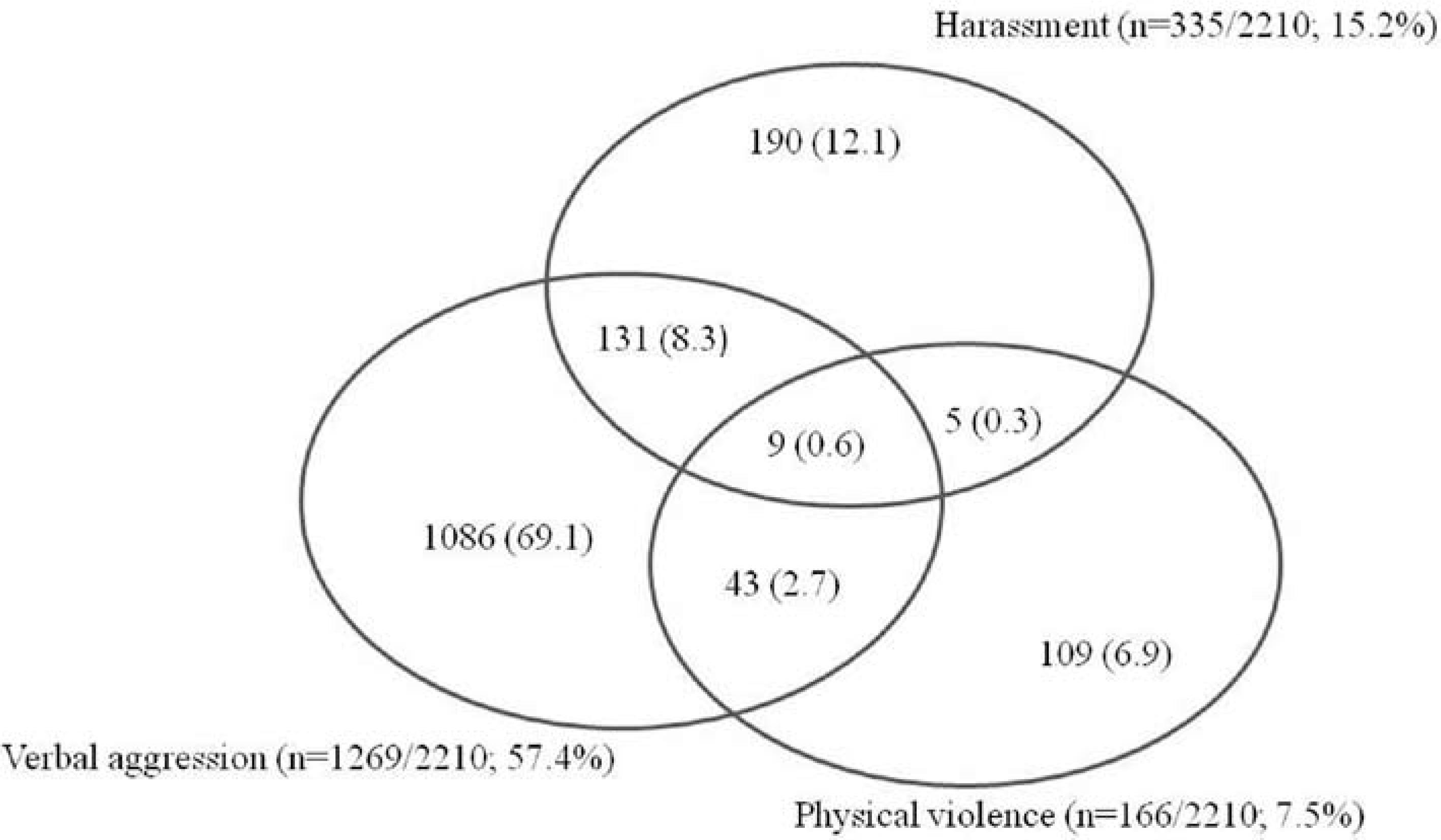
Combination of health-care workers' experiences of workplace violence by patients, patients' guardians and patients' relatives (n=1,770).
| Victims | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Verbal aggression (1,269) | Physical violence (n=166) | Harassment (n=335) | |||||||
| Variables | Men | Women | Chi-square | Men | Women | Chi-square | Men | Women | Chi-square |
| p value | p value | p value | |||||||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| Perpetrators | |||||||||
| Violence perpetrated by patients | 2.063 | 0.307 | 5.651 | ||||||
| Yes | 221 (17.4) | 289 (22.8) | 0.151 | 28 (16.9) | 28 (16.9) | 0.579 | 87 (26.0) | 129 (38.5) | 0.017* |
| No | 360 (28.4) | 399 (31.4) | 50 (30.1) | 60 (36.1) | 64 (19.1) | 55 (16.4) | |||
| Violence perpetrated by patients' guardians | 0.965 | 1.178 | 8.329 | ||||||
| Yes | 158 (12.5) | 216 (17.0) | 0.326 | 19 (11.4) | 15 (9.0) | 0.278 | 19 (5.7) | 40 (11.9) | 0.004* |
| No | 405 (31.9) | 490 (38.6) | 60 (36.1) | 72 (43.4) | 146 (43.6) | 130 (38.8) | |||
| Violence perpetrated by patients' relatives | 0.356 | 1.489 | 13.400 | ||||||
| Yes | 203 (16.0) | 182 (14.3) | 0.55 | 41 (24.7) | 35 (21.1) | 0.222 | 16 (4.8) | 44 (13.1) | <0.001* |
| No | 450 (35.5) | 434 (34.2) | 40 (24.1) | 50 (30.1) | 145(43.3) | 130 (38.8) | |||
| Work experience (years) | 0.005 | 5.089 | 0.266 | ||||||
| 0–5 | 326 (25.7) | 411 (32.4) | 0.94 | 42 (25.3) | 41 (24.7) | 0.024* | 65 (19.4) | 134 (40.0) | 0.606 |
| 6–45 | 238 (18.8) | 293 (23.1) | 52 (31.3) | 31 (18.7) | 54 (16.1) | 82 (24.5) | |||
| Workplace | 1.377 | 4.467 | 5.542 | ||||||
| Hospital | 70 (5.5) | 103 (8.2) | 0.848 | 14 (8.4) | 4 (2.4) | 0.346 | 15 (4.5) | 27 (8.1) | 0.236 |
| Clinic | 80 (6.3) | 147 (11.6) | 21 (12.7) | 17 (10.2) | 19 (5.7) | 47 (14.0) | |||
| Community health center | 367 (29.0) | 421 (33.2) | 51 (30.7) | 48 (28.9) | 74 (22.1) | 125 (37.3) | |||
| Dispensary | 45 (3.6) | 32 (2.6) | 8 (4.8) | 3 (1.8) | 11 (3.3) | 17 (5.1) | |||
| Health-care facility sector | 1.146 | 1.663 | 0.123 | ||||||
| Public | 106 (8.3) | 166 (13.1) | 0.286 | 26 (15.7) | 17 (10.2) | 0.197 | 26 (7.8) | 50 (15.0) | 0.726 |
| Private | 458 (36.1) | 539 (42.5) | 68 (41.0) | 55 (33.1) | 93 (27.8) | 166 (49.6) | |||
| Profession | 0.362 | 2.717 | 2.471 | ||||||
| Nurse | 267 (21.0) | 482 (38.0) | 0.547 | 42 (25.3) | 47 (28.3) | 0.099 | 56 (16.7) | 156 (46.6) | 0.116 |
| Others | 287 (22.6) | 214 (16.9) | 52 (31.3) | 25 (15.1) | 63 (18.8) | 60 (17.9) | |||
| Marital status | 6.792 | 0.873 | 7.712 | ||||||
| Unmarried | 161 (12.7) | 243 (19.1) | 0.009* | 25 (15.0) | 25 (15.0) | 0.350 | 38 (11.3) | 95 (28.4) | 0.005* |
| Married | 403 (31.8) | 462 (36.4) | 69 (41.6) | 47 (28.4) | 81 (24.2) | 121 (36.1) | |||
| Have children | 2.409 | 1.553 | 4.366 | ||||||
| Yes | 409 (32.2) | 505 (39.8) | 0.121 | 73 (44.0) | 52 (31.3) | 0.213 | 84 (25.1) | 139 (41.5) | 0.037* |
| No | 155 (12.2) | 200 (15.8) | 21 (12.7) | 20 (12.0) | 35 (10.4) | 77 (23.0) | |||
Perceived reasons for WPV were assessed in a blank description space. Our findings showed that a large majority (1,392/2,021; 68.8%) cited disrespect for medical deontology as the major cause of aggressive behaviors towards HCWs by patients or their relatives. There was no significant difference in perceived reasons for WPV between genders (Table 3).
| Variable | Total (n=2,021) n (%) | Men (n=989) n (%) | Women (n=1,221) n (%) | Chi-square test value (p value) |
|---|---|---|---|---|
| Disrespect for medical deontology | 1,392 (68.8) | 617 (62.4) | 775 (63.5) | 0.276 (0.599) |
| Lack of good manners towards patients, their guardians or relatives | 275 (13.6) | 137 (13.9) | 138 (11.3) | 3.261 (0.071) |
| Lack of protection from the government | 135 (6.7) | 58 (5.9) | 77 (6.3) | 0.186 (0.666) |
| Violence perceived as an unavoidable part of their work | 97 (4.8) | 35 (3.5) | 62 (5.0) | 3.083 (0.079) |
| Poor collaboration between patients and health-care workers | 119 (5.9) | 49 (5.0) | 70 (5.7) | 0.650 (0.420) |
| Combination of disrespect for medical ethics and insufficiency of government spending on the health system | 3 (0.2) | 2 (0.2) | 1 (0.1) | 0.583 (0.445) |
Odds ratios were calculated using logistic regression analysis in order to determine predictors of aggressive behaviors (Table 4). The results revealed that married HCWs were more likely to be involved in verbal aggression. Male HCWs were mainly victims of physical violence, whereas female HCWs were the prime target for harassment.
| Variables | Verbal aggression (n=1,269) | Physical violence (n=166) | Harassment (n=335) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes, n (%) | Adjusted OR (95% CI)† | p value | Yes, n (%) | Adjusted OR (95% CI)† | p value | Yes, n (%) | Adjusted OR (95% CI)† | p value | |
| Gender | |||||||||
| Men | 564 (44.4) | 1.00 | 94 (56.6) | 1.00 | 119 (35.5) | 1.00 | |||
| Women | 705 (55.6) | 0.91 (0.70,1.17) | 0.488 | 72 (43.4) | 0.57 (0.41,0.79) | 0.001* | 216 (64.5) | 1.49 (1.16,1.92) | 0.002* |
| Age (years) | |||||||||
| ≤29 | 428 (33.7) | 1.00 | 54 (32.5) | 1.00 | 128 (38.2) | 1.00 | |||
| ≥30 | 841 (66.3) | 1.12 (0.98,1.28) | 0.085 | 112 (67.5) | 0.99 (0.83,1.18) | 0.98 | 207 (61.8) | 0.92 (0.81,1.05) | 0.251 |
| Work experience (years) | |||||||||
| 0–5 | 737 | 1.00 | 0.57 | 83 (50.0) | 1.00 | 0.243 | 199 (59.4) | 1.00 | 0.229 |
| 6–45 | 531 | 0.98 (0.93,1.03) | 83 (50.0) | 1.03 (0.97,1.10) | 136 (40.6) | 1.03 (0.98,1.08) | |||
| Health-care facility sector | |||||||||
| Public | 272 (21.4) | 1.00 | 43 (26.0) | 1.00 | 76 (22.7) | 1.00 | |||
| Private | 997 (78.6) | 1.22 (0.90,1.66) | 0.187 | 123 (74) | 0.83 (0.56,1.22) | 0.354 | 259 (77.3) | 0.87 (0.64,1.81) | 0.384 |
| Workplace | |||||||||
| Community Health Center | 788 (62.1) | 1.00 | 99 (59.6) | 1.00 | 199 (56.1) | 1.00 | |||
| Others | 480 (37.8) | 0.97 (0.84,1.12) | 0.723 | 67 (40.4) | 0.98 (0.81,1.18) | 0.876 | 136 (38.3) | 0.92 (0.80,1.06) | 0.296 |
| Matrimonial status | |||||||||
| Unmarried | 404 (32) | 1.00 | 50 (30.1) | 1.00 | 133 (39.7) | 1.00 | |||
| Married | 865 (68) | 0.72 (0.55,0.95) | 0.021* | 116 (69.9) | 0.98 (0.68,1.41) | 0.931 | 202 (60.3) | 1.26 (0.97,1.64) | 0.078 |
| Profession | |||||||||
| Nurse | 749 (59.0) | 1.00 | 89 (53.6) | 1.00 | 212 (63.3) | 1.00 | |||
| Others | 501 (39.5) | 1.12 (0.86,1.46) | 0.364 | 77 (46.4) | 0.87 (0.62,1.22) | 0.440 | 123 (36.7) | 1.09 (0.84,1.41) | 0.508 |
| Have children | |||||||||
| No | 355 (28.0) | 1.00 | 41 (24.7) | 1.00 | 112 (33.4) | 1.00 | |||
| Yes | 914 (72.0) | 0.83 (0.61,1.12) | 0.228 | 125 (75.3) | 0.95 (0.63,1.44) | 0.832 | 223 (66.6) | 1.13 (0.84,1.51) | 0.394 |
Seventy-five percent (1,329/1,770) of those who had been victims of aggressive behavior indicated that they had informed third persons about the violent episodes, but only 34.3% (608/1,770) reported the incident to senior staff. About 54.2% (721/1,329) of the HCWs indicated they had verbally shared information about the incident in an attempt to get support. Help mainly came from coworkers (27.2%), followed by a spouse or partner (16.0%), friends (13.0%), and family members (8.2%) and 5.0% of the HCWs indicated that they had kept the incident secret.
To the best of our knowledge, this is the first study conducted in the DRC to investigate health-care workers' experiences of WPV by patients, patients' guardians and patients' relatives. This study reveals that the prevalence of WPV in the DRC is an issue of public concern; the prevalence of WPV was very high and can be classified among the highest in the world. The disrespect for medical deontology by HCWs was the major perceived reason for WPV. Furthermore, this study found that the majority of violent episodes were underreported. As the first study scrutinizing WPV among HCWs, it helps to give an overview of WPV towards HCWs in the Congolese economic, political and cultural contexts. Although a large number of HCWs thought that they were at fault for being victims of WPV in this study, aggressive behaviors towards HCWs might be the consequence of various factors but can be attributed to a large degree to distal determinants such as the Congolese decade-long armed conflict21), which has led to an alarming decline in the economy, political instability, food insecurity and collapse of the health-care system.
In order to comprehend WPV perpetrated by patients and their relatives in Congolese health-care facilities, it is important to understand the reality of the unequal access to medical care between the haves and have-nots. Access to basic health-care is financially difficult for less privileged patients because of the country's mismanagement combined with the decade-long armed conflict22). Up until the autumn of 2012, the Congolese government did not provide citizens with health insurance and social welfare at the national level. With only a small percentage of Congolese earning a sufficient wage23), taking care of patients is a financial challenge. As a result, HCWs tend to place more emphasis on more lucrative activities; with some exception in emergency cases, patients are required to buy a medical chart (fiche in French) prior to consulting a nurse or a doctor. In addition, patients need to purchase all the medicines necessary for their treatments even when they are admitted to the hospital. To make matters worse, nurses sometimes sell those medicines. Another culprit is the hospital discharge fee. In some instances, patients are locked in the hospital and prevented from leaving when they cannot afford the discharge fee. This situation sometimes leads to quarrels between HCWs and patients or their relatives. This is the background to the high prevalence of WPV found in this study.
Our results show a challenging level of WPV (80.1%). As previously reported9, 24–27), the prevalence of WPV found in this study shows that HCWs are highly exposed to violence from patients while on duty; this risk of WPV among HCWs is even comparable to that of policemen2). This study indicates that patients (including their relatives and guardians) are committing violence towards HCWs in the DRC; this situation is quite surprising, as Congolese society is traditionally a nonviolent society and HCWs have been highly respected in Congolese society. Although detailed data regarding the perpetrators' gender and age were not available as this study did not investigate them, it would be worthwhile to discuss who the perpetrators were in order to work toward prevention of WPV. Most perpetrators were patients (Fig. 1); this is proof that the relationship between patients and HCWs is not always amicable in the Congolese context. Patients are certainly the first people to witness errors or unethical actions performed by HCWs; accumulation of a degree of frustration by patients can probably lead to violence. In addition, the relationship between aggressive behaviors and mental illness cannot be ignored. Some patients might have psychiatric health problems and might therefore be more likely to be predisposed to perpetrate violence towards HCWs especially when the HCWs do not react adequately to their needs. In this context, HCWs have to be trained to improve their skills to identify patients who are predisposed to perpetrate aggressive behaviors and to recognize situations that could lead to aggressive behaviors.
The most common type of aggressive behavior found in this study was verbal aggression, providing further information that interpersonal relationships between patients and HCWs are sometimes poor in the Congolese context. The prevalence of verbal aggression found in this study is somewhat similar to that found in previous studies that demonstrated a higher level of WPV towards HCWs24, 28). One study found that 57.9% of Palestinian doctors and nurses experienced verbal aggression (vs. 57.4% in this study)24), with a similar percentage of nurses responding in both studies (59.2% in our study versus 65.8% in the Palestinian study). Along this line, another study carried out in Pakistan reported that 72.5% of nurses and doctors were victims of verbal aggression28). While our findings are consistent with these studies, there are several differences between these studies that deserve mentioning. Comparing our study to the Palestinian study, we targeted more HCWs in both private and public sectors (Table 1), whereas the Palestinian study24) included only doctors and nurses from the public sector. Compared with the Pakistani study, the Pakistani targeted only doctors and nurses in emergency departments28).
Similarly, the prevalence of physical violence found in this study (Fig. 2) was about half of that in the Pakistani study (16.5%) and a third of that in the Palestinian study (20.8%). It is difficult to compare statistics regarding WPV across countries because of the differences that might exist in the definition of the concept of WPV. However, it is relatively easy to compare physical violence at work across countries as compared to verbal violence and harassment because of the clarity of the definition regarding physical violence. Possible reasons for the difference in prevalence regarding physical violence in our study and studies carried out in Palestine24) and Pakistan28) might be related to the difference in cultural backgrounds. Within the context of economic crises and political instability, the prevalence of physical violence found in this study is lower than that found in studies in other countries such as the study carried out among Iraqi nurses29), which found higher levels of physical violence (42.2%) during the country's times of economic crisis and political instability. However, the prevalence of physical violence found in our survey is similar to that reported among Israel's doctors (9% vs. 7.5% in this study)30) and Spanish HCWs (11% vs. 7.5% in this study)31).
Our findings showed that female HCWs were more likely to be victims of harassment. Most of the harassment was sexually oriented in nature (63.6%), a taboo subject in Congolese society and most probably a source of stress for the victims. The frequency of sexual harassment found in this study is not exceptionally high. However, it deserves serious attention considering the fact that sexual harassment at work is morally reprehensible and might affect HCWs' productivity. Therefore, these findings reinforce the importance of the recognition of violence towards HCWs by Congolese health policy-makers, so that establishment of effective policies can occur.
In this study, only 34.3% of the violent episodes were reported to a supervisor, this being a common finding reported by researchers2, 32, 33) when studying WPV in general. A study of nurses in the Canadian provinces of Alberta and British Columbia also showed underreporting of aggressive behaviors, with only 30% being reported, as in our study33). As Milczarek34) suggested, HCWs thinking that a violent attack on them is their own fault plays a crucial role in the underreporting of WPV. In support of this view, our data show that a large majority (68.8%) of the HCWs felt they were at fault and that their disrespect for medical deontology was the cause of WPV. In regard to sexual harassment, incidents might not be disclosed for cultural reasons; usually people in Congolese society are afraid to talk about sex-related matters because of the sensitivity of the subject. Another more likely reason that might contribute to underreporting is the seriousness of the problem; if the HCWs think that a problem is not serious, they might not report it. One more reason could be the lack of an adequate WPV management system and the perception that even if an incident is reported, no action will be taken. One consequence of failure to report WPV is the absence of evidence that might help health policy-makers to be aware of WPV.
The response rate for the questionnaire was 99%. This excellent response rate is probably due to the large number of people involved in the data collection, as well as the study topic itself and its design. The results underscore the fact that the problem had reached a challenging level requiring action. Similar excellent response rates have been reported in previous studies conducted in Nigeria (90%)27), and Palestine (92%)24), which both have difficult living conditions similar to the DRC. In contrast, the excellent response rate in the present study clearly differs from what was previously found in a similar study conducted in Spain (28.3%)31), where living conditions are probably better than those in the DRC. Although there are differences in the response rates between the two studies, the study conducted in Spain31) showed a prevalence of physical violence (11%) similar to our findings (Fig. 2).
The impact of the prevalence of WPV found in this study can also be discussed in regard to its interference with the quality of health care5) and the shortage of HCWs that most countries are facing. The prevalence of WPV in Congolese HCWs is putting an extra burden on the already insufficient Congolese health-care system, which is losing HCWs, as many are migrating to other countries in search of greener pastures. In this regard, WPV towards HCWs is a threat that might contribute to a decline in the number of HCWs and a lowering of the quality of patient care in terms of increasing the risk of errors.
This study has evitable and inevitable limitations. First, in studying the prevalence of WPV and its determinants, several researchers32) have reported that it is difficult to compare and contrast statistics from different countries for several reasons, such as the discrepancy in the concepts being studied, inconsistencies in the methods used and cultural differences in the experience of violence32). As we could not find previously published research in the literature regarding WPV in the DRC, our findings were therefore cautiously compared with studies in countries where health-care systems, workplace environment, and cultural background regarding the understanding of verbal violence and harassment might be different from those of the DRC; examples of such differences include male nurses working in the female patient wards, wartime conditions in the country and cultural differences relating to the understanding of verbal violence or harassment. However, despite cultural differences concerning the definition of verbal violence and harassment, the fact that the concept of aggressive behaviors (verbal aggression and harassment) used in this study was defined according to previous international studies4, 20) allows us to compare our study with studies in other countries. Second, we did not assess WPV committed by coworkers; from our experience, however, there is no reason not to accept the possibility that coworkers are also committing violence against HCWs, since we have witnessed harassment by superiors in Congolese hospitals. In the future, violence by coworkers needs to be investigated and prevented. Third, we used a questionnaire to collect data, which may have led to recall bias and thus introduced the risk of missing some informative details; the reliability and validity of some responses are difficult to verify. Fourth, HCWs might not be completely representative of the HCWs in the DRC, as we did not use any predefined statistical sampling methods that would epidemiologically represent the health-care workforce in the DRC. Despite this fact, we assume that these results can reveal the reality of the current WPV situation in Congolese health-care facilities. These limitations would not change the magnitude of the problem given the fact that the DRC health-care system faces many challenges; the working conditions of HCWs are still precarious, especially in public hospitals.
The strength of this study is that it includes a great number of health-care facilities located in different cities and towns, and its results reflect most probably the situation of WPV in the DRC. For the first time, our data can be used by the Congolese authorities as a pilot study to recognize, analyze, and support further research aimed at providing answers concerning WPV in the Congolese health sector.
In a nutshell, the most important finding in this study is that patients and their relatives are committing violence towards Congolese HCWs despite the fact that HCWs have traditionally been highly esteemed in the DRC. These aggressive behaviors appear to be mainly due to misconduct of HCWs attributable to a large degree to distal determinants such as the collapse of the health-care system. The results from this study highlight the need for further studies on this issue to suggest opportunities for combating aggressive behaviors in Congolese health-care facilities.
Acknowledgments: This study was financially supported by the Department of Environmental Medicine of Kochi Medical School, Kochi University, Japan. The authors deeply thank all the participants of this study. We are also grateful to Ms Yasumitsu-Lovell Kahoko, Mr. Daniel Ribble, Mr Peter Duveen, Mr Mugo Andrew and Ms Mansongi Biyela Carine for helpful remarks on the draft of this manuscript.