2016 Volume 58 Issue 5 Pages 482-488
2016 Volume 58 Issue 5 Pages 482-488
Objectives: Occupational exposure to paraffin is an infrequent cause of lipoid pneumonia (LP) and related data are scare. We investigated the possible relationship between three rare cases of chronic LP and occupational exposure to paraffin aerosol in an iron foundry. Methods: The three cases of LP and their workplaces were investigated using data from field investigations, air monitoring, pulmonary radiological examinations, cell staining, and lung biopsies. Results: The patients had long-term occupational exposure to paraffin. X-ray diffraction testing revealed that the raw material from the workshop was paraffin crystal. The air concentrations of paraffin aerosol in workplaces were significantly higher than outdoor background levels. Small diffuse and miliary shadows with unclear edges were observed throughout the whole lungs via radiography. Computed tomography revealed diffuse punctate nodules and a high density of stripe-like shadows in both lungs (ground-glass opacity in a lower lobe, and a mass-like lesion and high translucent area near the bottom of the lung). Lipid-laden macrophages were found in the sputum and bronchial lavage. A broadened alveolar septum and local focal fibrosis were also discovered via lung biopsy. The inflammatory reaction in the lung tissues appeared to resolve over time. Conclusions: These three rare cases of chronic LP in workers during molding and repair processes were associated with occupational paraffin aerosol exposure. Therefore, primary prevention is essential for molding or repairing workers in the iron foundry, and a differential diagnosis of occupational chronic LP (vs. pneumoconiosis) should be considered when treating these workers.
Lipoid pneumonia (LP) is a rare form of pneumonia that results from the pulmonary accumulation of fat-like compounds from animal, vegetable, or mineral origins1). Chronic endogenous LP is a major form of LP, and usually results from long-term exposure to oil steam2). The lipid materials that lead to exogenous LP are usually present in food, radiography contrast media, or oil-based medications, such as laxatives and nasal drops.
Occupational exposure to paraffin is an infrequent cause of LP, and only a few well-documented cases of occupational LP have been reported2). One case of LP was caused by paraffin oil droplet exposure (from a filling process in a cardboard crockery factory)3), and another case of LP was caused by chronic paraffin exposure during the cleaning of new cars (which are protected using paraffin)4). Among 44 cases of LP, only four cases with chronic inhalation of paraffin aerosol or oil steam were found in a French retrospective study5). However, these case reports are limited by their focus on the patients' clinical characteristics, as exposure data are needed to confirm a diagnosis of occupational LP.
The pathological sign of LP is a chronic foreign body reaction to inhaled/aspirated mineral oil, which is characterized by the presence of lipid-laden macrophages6). Mineral oil inhalation is usually unnoticed, as it does not induce an obvious reactive response in the airways. However, this inhalation may impair mucociliary transport and reduce the clearance of the oil droplets from the respiratory tract. Thus, chronic LP usually presents as an insidious condition with diverse and non-specific clinical and radiological characteristics that can mimic many other lung diseases, including lung tumors, pulmonary tuberculosis, and fibrosis7). Therefore, chronic LP is readily misdiagnosed as other lung diseases, or its diagnosis can be missed altogether, as it is usually not considered during the differential diagnoses. The diagnosis of exogenous LP is generally based on a history of oil exposure, with radiological findings that are consistent with the disease and the presence of lipid-laden macrophages in sputum or bronchoalveolar lavage samples8).
The workers in iron foundries may be frequently exposed to silica dust and have a high risk of developing pneumoconiosis. Furthermore, pulmonary tuberculosis is a common complication of pneumoconiosis9). In this study, we investigated three rare cases of LP in workers at an iron foundry, which were originally suspected as pneumoconiosis with pulmonary tuberculosis by the treating physicians. We also evaluated the patients' occupational paraffin exposures using qualitative and quantitative analysis. The results from this study may provide a scientific basis for the diagnosis and prevention of occupational LP.
Three patients (ages: 41, 45, and 49 years) underwent occupational health check-ups in April 2014, and were suspected as having pneumoconiosis with tuberculosis by a local hospital. The patients' clinical symptoms included occasional coughing, mild chest tightness, shortness of breath, minimal phlegm, no fever, and no chest pain. The three patients underwent 6 months of anti-tuberculosis therapy from April to September, 2014. However, the clinical syndromes were not improved during the anti-tuberculosis therapy. The patient's history is illustrated in Fig. 1. All three patients were female, and none of them had smoking and drinking habits. They were molding and mold repair operators (7, 8, and 11 years of exposure), and did not have other occupational histories. The patients were informed of the objective of this study, and consented to participate in this investigation. The ethical committee of Lishui Center for Disease Control and Prevention (CDC) in Zhejiang province of China approved the research schedule used in this investigation (No. LSCDCLL2015-001).
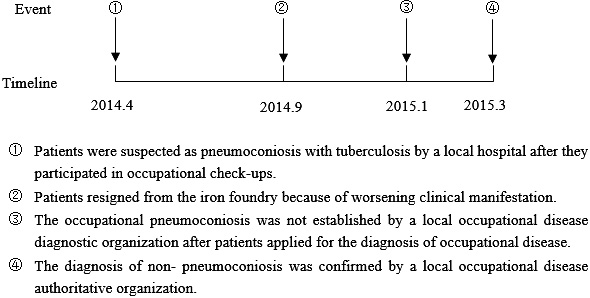
Timeline of patient's history.
The private small-scale iron foundry specialized in producing components for mining machinery, and was located in a mountainous area in southwest Zhejiang province (China). The molding and mold repair workshops, where mechanical ventilation measures and natural ventilation were poor, employed 32 workers (27 women) including 3 patients. The morbidity of LP was 9.4%. None of the workers wore effective personal protective equipment.
The production processes were: (1) melting the raw solid paraffin in a separate workshop and piping the melted paraffin into insulated barrels in the molding workshop; (2) injecting the liquid paraffin into the molds under high pressure and cooling the mold with water; (3) manually repairing paraffin models with rough surfaces or minor defects using small amounts of liquid paraffin that were prepared in a small bowl on an electric stove; (4) sand blasting the paraffin models with quartz and refractory sands; (5) casting the molten iron; and (6) cleaning the products' surfaces. Three processes, i.e., high-pressure injection, temporary storage in insulated barrels, and repairing, could produce paraffin aerosol. No dust release was observed during the molding or mold repair processes. Silica dust release was obvious during the sand blasting and product formation in the other workshops.
Qualitative analysis of the raw materials and air samplesX-ray diffraction (XRD; PANalytical Empyrean, Netherland) was used to analyze paraffin crystals from the raw material and air samples that were collected via a sampling pump with a flow rate of 15 L/min and a sampling time of 8 h. The XRD detection conditions were: a Cu K-alpha ray, an acceleration voltage of 40 kV, and a current of 40 mA. In addition, parallel samples were analyzed for free silica, according to the Chinese occupational health standard (the GBZ/T 192.4-2007 "Determination of dust in the air of workshops-Part 4: free silica content in dust" ).
Air monitoringDuring June 2015, individual and area samples were obtained to evaluate the air concentrations of paraffin aerosol over 3 consecutive days. According to the Chinese occupational health standard (the GBZ159-2004 "Specifications for air sampling of hazardous substances in the workplace" ), individual samples were obtained from molding and mold repair workers to monitor their exposure to paraffin aerosol with a flow rate of 2 L/min and a sampling time of 8 h. The individual concentrations of paraffin aerosol were calculated based on the weights of the filter membranes. A real-time aerosol monitor (DustTrak 8530, TSI, USA) was also used to monitor the respirable concentrations of paraffin aerosol (<1 μm) in the molding and mold repair workshops, with a sampling time of 4 h. At the same time, outdoor concentrations were monitored to determine the background levels of paraffin aerosol.
ImagingA digital X-ray system (DR; DRX-Evolution, Carestream Health, Canada) was used to obtain chest radiographs from the patients in April 2014. Computed tomography (CT; Brilliance ICT SP, Philips, Netherlands) was also used to examine the patients' chests, and the changes in the CT findings were evaluated in April, June, and September 2014 and February 2015.
Cell stainingThe patients' sputum samples were collected in sterilized glass bottles within 24 h. A 50-mL volume of saline solution was injected during the bronchoscopic examination, and the lavage fluid was collected. The sputum and bronchoalveolar lavage fluid were set on slides, and mononuclear macrophages were observed using Gram staining, Giemsa staining, and Sudan red staining, under an optical microscope.
Tissue biopsyFiber optic bronchoscopy was performed to obtain lung tissue biopsy samples, which were evaluated using hematoxylin and eosin staining under an optical microscope.
Diagnostic methodThe diagnosis of exogenous LP is based on a history of exposure to oil with radiological findings in keeping with the disease and the presence of lipid-laden macrophages on sputum or bronchoalveolar lavage analysis2). In this study, we also investigated the exposure data in detail, including workplaces, qualitative analysis of the raw materials and air samples, and air monitoring. A differential diagnosis was considered.
Statistical methodOne-way analysis of variance with the least significant difference post-hoc test (equal variances) was used to analyze the differences of respirable concentrations of paraffin aerosol concentrations between workshop and background samples.
The XRD test results revealed that the raw material was paraffin, with a molecular formula of (CH2) x (i.e., n-paraffin) (Fig. 2). The air samples did not contain any paraffin crystals or free silica. Table 1 shows the individual paraffin aerosol concentrations for molding and mold repair operators (0.95±0.13 and 1.58±0.13 mg/m3, respectively). The real-time paraffin aerosol concentrations at the molding and mold repair locations were significantly higher than the background concentration (P<0.01).
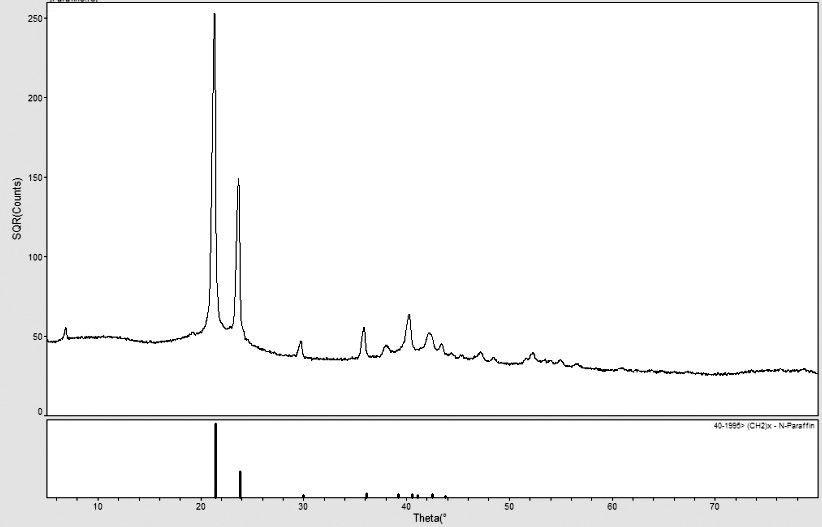
X-ray diffraction graph for the raw material.
| Location | Individual sampling | Area sampling | Background (mg/m3) | ||
|---|---|---|---|---|---|
| Concentration (mg/m3) | n | Concentration (mg/m3) | n | ||
| a compared to background concentration, p<0.01 | |||||
| Molding | 0.95 ± 0.13 | 4 | 0.15 ± 0.03a | 3 | 0.07 ± 0.01 |
| Mold repairing | 1.58 ± 0.13 | 4 | 0.16 ± 0.03a | 3 | |
A representative chest radiograph from one of the patients is shown in Fig. 3a. The whole lung (especially in the lower and middle lobes) exhibited diffuse miliary, punctate, and small shadows with unclear edges, which were significantly different from the characteristics of a normal chest radiograph. A representative CT image of one of the patient's chest is shown in Fig. 3b, which reveals diffuse punctate nodules and a high density of stripe-like shadows with unclear edges in both lungs. The lower part of the left lower lobe exhibited ground-glass opacities (Fig. 3c), and the bottom of the lung exhibited a mass-like lesion and a high translucent area (Fig. 3d). The alveolar gas retention was caused by terminal pulmonary bronchiole spasms.

Radiological manifestations. (a) A representative chest radiograph for the three patients. (b) A representative computed tomography image of a patient's chest, which exhibits diffuse punctate nodules and a high density of stripe-like shadows with unclear edges in both lungs. (c) A ground-glass like change in the lower part of the left lower lobe. (d) A mass-like lesion and a high translucent area near the bottom lung. (e) Shadows in the initial computed tomography image from April 2014. (f) The shadows increase in the image from June 2014. (g) The shadows reach a peak in September 2014. (h) The shadows decrease gradually in February 2015.
Fig. 3e-h shows the changes in CT findings for a single patient from April 2014 to February 2015. The patient resigned her job in April 2014, which discontinued her exposure to paraffin, although she did not receive any medical treatment. The lung shadows gradually increased during April-June 2014 (Fig. 3e and 3f), peaked in September 2014 (Fig. 3g), and subsequently decreased until February 2015 (Fig. 3h).
Cell stainingFig. 4a and 4b shows the Gram and Giemsa staining for monocytes in the patients' sputum, respectively. The monocytes' cytoplasms contained large numbers of small vacuoles, which suggested that the monocytes had phagocytized a large number of lipid droplets. These results were confirmed by Giemsa staining for monocytes in the bronchoalveolar lavage fluid (Fig. 4c). Furthermore, dark-orange lipid droplets in the cytoplasm were observed after Sudan red staining (Fig. 4d). These staining results indicated that lipid-laden macrophages were present in the patients' sputum and bronchoalveolar lavage fluid.

Cell staining, bronchoscopy, and tissue biopsy. (a) Lipid-laden macrophages with Gram staining in sputum. (b) Lipid-laden macrophages with Giemsa staining in sputum. (c) Lipid-laden macrophages with Giemsa staining in bronchoalveolar lavage fluid. (d) Lipid-laden macrophages with Sudan red staining in bronchoalveolar lavage fluid. (e) Diffuse mucosal hyperemia is visible in the upper or lower lobe bronchus. (f) Widened alveolar space, cell reaction, and localized fibrosis in lung tissues. A tissue biopsy sample was stained using hematoxylin and eosin.
Fig. 4e shows the bronchoscopy findings, which revealed diffuse mucosal hyperemia in the upper or lower lobe bronchus, and suggested that inflammation existed in the bronchus.
Lung biopsyThe alveolar space was widened, and no obviously inflammatory cells were present. However, a cell reaction and localized fibrosis were observed in the lung tissues, although no silicotic nodes were observed (Fig. 4f).
Paraffin is a solid-state advanced alkane mixture, which is mainly comprised of linear alkanes with 18-30 carbon atoms. Our XRD findings (Fig. 2) confirmed that the raw material was indeed paraffin crystals. However, no paraffin was detected on the air sampling filter membranes, although this could be due to the fact that the paraffin did not form crystals on the filter membrane. Other appropriate methods should be used to detect the paraffin content in the air sample in the future. Nevertheless, the air samples did not contain free silica, which suggested that the patients were not exposed to silica dust and had not developed silicosis. Therefore, these findings suggest that the patients were exposed to paraffin aerosol, rather than silica dust.
In addition to confirming the presence of paraffin, we used field investigation and quantitative determination to collect exposure data, including exposure history, scenario, and concentrations. The three patients were molding and mold repair operators with long-term occupational exposures. The paraffin aerosol might be generated via three processes: high-pressure molding, unclosed storage of liquid paraffin, and paraffin melting for the repair process. This finding is similar to the findings of previous studies, in which some processes, including machine maintenance and filling, cleaning with compressed air jets, and cutting, could generate paraffin aerosol3-5). We also found that high levels of paraffin aerosol were inhaled by the molding and mold repair workers. Moreover, the average year of exposure (8.67±2.08 years) in the three patients was significantly higher than that (2.94±1.97 years) of other exposed workers who did not suffer LP (P<0.05). The longer exposure duration of paraffin aerosol may explain why only three workers suffered from LP, whereas other exposed workers did not suffer from LP. These findings suggest qualitative and quantitative monitoring for paraffin in air or raw materials is very important for the diagnosis of occupational LP, and this exposure should be considered by occupational physicians.
In this study, our radiography and CT findings revealed that the patients exhibited diffuse nodules with unclear edges in both lungs. The CT findings also revealed ground-glass opacities, a mass-like lesion, and alveolar gas retention in the lower lobes. These results suggested that inflammation was present and that fluid was exuded into the lung; the presence of long-term inflammation might have led to pulmonary fibrosis. Similar radiological symptoms have been reported in many cases of exogenous LP10,11). Compared to the typical radiological characteristics, the clinical symptoms of LP in this study were non-specific, as the patients exhibited an occasional cough, mild chest tightness, shortness of breath, and minimal sputum; these findings are consistent with those of many LP case reports12).
There is no consensus regarding the best therapeutic option for treating exogenous LP, although it is important to identify and discontinue exposure to the lipid substance13). If the patient discontinues any exposure to the lipid substance, their radiographical abnormalities may resolve within months14). In this study, the dynamic change in the CT shadow's density revealed that the density reached a peak within 6 months after discontinuing paraffin exposure, and that it had decreased within 11 months after discontinuing exposure. This result confirms the reversibility of the inflammatory reaction that is induced by paraffin in the lung tissues.
In this study, the positive cell staining results indicated the presence of lipid-laden macrophages, which is a specific feature of LP. This phenomenon can be explained by a pathophysiological perspective, as LP is a result of a chronic foreign body reaction to inhaled or aspirated mineral oil. Once the mineral oil reaches the alveoli, the oil is phagocytized by alveolar macrophages (which cannot metabolize the lipids) and is subsequently released back into the alveoli after the death of the macrophages15). This repeated process (phagocytosis and release) induces a giant cell granulomatous reaction, chronic inflammation, and alveolar and interstitial fibrosis. This process likely explains the pulmonary inflammation and fibrosis that were present in the three patients.
The three cases were definitely diagnosed with chronic occupational LP due to paraffin aerosol, based on the patients' exposure data, specific radiographical features, and the presence of lipid-laden macrophages in their sputum and bronchoalveolar lavage fluid. Because chronic LP, especially chronic occupational LP, is a rare disease, its diagnosis is difficult and it is often misdiagnosed as other lung diseases. For example, all three cases were suspected as pneumoconiosis with tuberculosis by a local hospital. Several factors may affect this suspicion. Firstly, workers at casting and forming locations (e.g., iron foundries) have a high risk of developing pneumoconiosis due to silica dust exposure. Secondly, pneumoconiosis is also a form of pulmonary fibrosis. Thirdly, clinicians may not have access to sufficient exposure data, as they may rely on the patient's self-reporting (rather than a full field investigation). Fourthly, if there is no reason to suspect paraffin exposure, the clinician may not request cell staining or lung biopsy, which are necessary to reach the correct diagnosis.
In conclusion, the three rare cases of chronic LP were associated with occupational exposure to paraffin aerosol. Sufficient exposure data is necessary to reach a diagnosis of occupational LP, and to differentiate it from pneumoconiosis. Therefore, primary preventative measures are essential for protecting these workers, and the preventative measures should include technological process improvement, appropriate general and local ventilation, occupational health services, including air monitoring and occupational health surveillance, effective personal protective equipment, and the establishment of an occupational health management system.
Acknowledgments: This work was in part supported by the Natural Science Foundation of China (81472961) and the Co-constructed Projects by the National Health and Family Planning Commission of China and the Health Bureau of Zhejiang Province (No. WKJ2014-ZJ-0).
Conflicts of interest: The authors declare that they have no conflicts of interest.