Abstract
Post-exposure prophylaxis (PEP) for healthcare workers is one of the effective strategies for preventing nosocomial outbreaks of influenza. However, PEP adherence in healthcare workers is rarely analysed, and no strategies have been established to improve adherence to PEP for healthcare workers. We aimed to retrospectively analyse adherence to PEP and the factors associated with non-adherence in healthcare workers. A survey of 221 healthcare workers who were eligible for PEP at Tokushima University Hospital in the 2016/2017 season was conducted. Once-daily oseltamivir (75 mg for 10 d) was used as the PEP regimen. Of the 221 healthcare workers, 175 received PEP and were surveyed for adherence using a questionnaire. Of the 130 healthcare workers who responded to the questionnaire, 121 (93.1%) had been vaccinated. In this survey, 82 healthcare workers (63.1%) did not fully complete PEP. Multiple logistic regression analysis revealed that physicians (odds ratio: 4.62, 95% confidence interval [CI]: 2.08–10.25) and non-vaccination (odds ratio: 9.60, 95% CI: 1.12–82.25) were the factors for non-adherence to PEP. Of the 47 healthcare workers who responded to the item regarding reasons for non-adherence, 36 (76.6%) reported forgetting to take oseltamivir or discontinuing it due to a misguided self-decision that continuation of PEP was unnecessary, and 5 (10.6%) reported discontinuing treatment due to adverse effects. In conclusion, healthcare workers, particularly physicians, had low PEP adherence owing to forgetting or stopping to take oseltamivir due to a misguided self-decision. To obtain the maximum preventive effect of PEP, medication education should be provided to endorse PEP compliance.
INTRODUCTION
Influenza causes nosocomial outbreaks through large respiratory droplets, direct or indirect contact, and small particle aerosol transmission.1) Prevention of nosocomial outbreaks of influenza is important because some patients, such as immunosuppressed and elderly patients, in healthcare settings, are at high risk of becoming severely ill due to influenza.2) Healthcare workers have frequent contact with patients with influenza and can easily become vectors for influenza transmission; thus, appropriate influenza outbreak prevention measures are needed for healthcare workers.3)
One of the effective strategies for preventing influenza outbreaks among healthcare workers is influenza vaccination.4) As influenza vaccination is approximately 40% effective at preventing hospitalization and 60% effective at preventing death, vaccination does not completely prevent the onset of influenza.5) In particular, the effectiveness of the vaccination is reduced in seasons where antigenic mutations of influenza are predicted or have been identified.6,7) Therefore, The Japanese Association of Infectious Disease recommends that if healthcare workers are thought to be involved in influenza outbreaks in a healthcare setting or if influenza outbreaks occur among healthcare workers, post-exposure prophylaxis (PEP) of anti-influenza drugs for healthcare workers is recommended regardless of whether healthcare workers have already received the vaccination.8) Moreover, the Infectious Diseases Society of America (IDSA) guidelines mention that, during institutional outbreaks, clinicians may consider PEP for staff who were not vaccinated or received an inactivated influenza vaccine.9)
A previous study reported that PEP with oseltamivir for 7–10 d reduces influenza outbreaks in clinical settings.10–12) Once-daily 75 mg oseltamivir for at least 7–10 d has generally been recommended for PEP in the IDSA guidelines.9) However, PEP with oseltamivir administration is long-lasting (more than a week). Moreover, maintaining the motivation to continue PEP with oseltamivir in healthcare workers is more difficult compared with that in patients with influenza because PEP is a prophylactic method for healthcare workers who have no influenza symptoms. Thus, the PEP strategy encompasses factors that make adherence worse. However, PEP adherence has rarely been analysed in healthcare workers, and no strategies have been established to improve their adherence to PEP. In this study, we aimed to retrospectively analyse adherence to PEP in healthcare workers by using questionnaires and determine the factors that prevent PEP adherence.
MATERIALS AND METHODS
Ethics Approval and Consent to ParticipateThe analysis was performed in conformance with the ethical guidelines of the Declaration of Helsinki. The study protocol was approved by the Tokushima University Hospital Ethics Committee (Ethics Committee Registration No. 3834). This study was implemented following the stipulations on the handling of patient personal information. We used an opt-out method on our official website (http://www.tokushima-hosp.jp/about/disclosure_document.html, in Japanese) as Japanese law does not require individual informed consent from participants in a non-invasive observational trial such as the present study (https://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanboukouseikagakuka/0000153339.pdf, in Japanese).
Study Design and PopulationWe conducted a retrospective survey of 221 healthcare workers who were eligible for PEP at Tokushima University Hospital (697 beds) in the 2016/2017 season. Our hospital infection control committee approved the PEP with an oseltamivir regimen for all healthcare workers who had close contact with influenza persons in the 2016/2017 season. In this PEP strategy, we defined healthcare workers who had contact with influenza persons within 2 m without a surgical mask regardless of vaccination as subjects for PEP. No PEP was administered to healthcare workers who wore appropriate personal protective equipment. Index cases were quarantined or restricted to work as soon as they were diagnosed with influenza. PEP was initiated within 24 h after close contact with index cases, and once-daily oseltamivir (75 mg) was prescribed for 10 d as a PEP regimen. Healthcare workers who were eligible for PEP were briefed in writing by physicians who were members of the hospital infection control committee for the purpose of PEP and the dosage of oseltamivir. They started taking oseltamivir after they agreed to PEP implementation. Healthcare workers who did not agree to PEP implementation were included in the non-PEP group. At the end of the PEP—namely, 10 d after the start of the PEP—a questionnaire was distributed to the PEP implementers by hand by the researcher after obtaining their verbal consent to participate. The questionnaire was collected on the same day after being completed by the subjects. The questionnaire consisted of items to investigate the type of occupation, exposure status, vaccination status, duration of administration of oseltamivir, reasons for discontinuation of oral administration, and the presence or absence of symptoms that were perceived as adverse effects (Supplementary Table 1). We also retrospectively investigated the positive rate of influenza within 10 d after close contact with the indexed cases in 221 subjects who were eligible for PEP. The incidence of influenza in healthcare workers was diagnosed by clinical symptoms or a rapid influenza antigen test in our study.
Statistical AnalysisComparisons of oseltamivir adherence between the type of occupations and differences in the influenza-positive ratio between the PEP and non-PEP groups were compared using the chi-square test or Fisher’s exact-square test. In multiple logistic regression analysis, the model was constructed by the forced-entry method using the questionnaire items. The p-value was adjusted by the Bonferroni method when more than three groups were compared. For all statistical analyses, values of p < 0.05 (two-tailed) were considered significant. All analyses were performed using JMP® version 14.3.0 (SAS Institute, Cary, NC, U.S.A.) and R statistical software version 4.0.2.
RESULTS
Study PopulationOf the 221 subjects who were eligible for PEP, 175 agreed to PEP implementation and were prescribed 75 mg oral oseltamivir once daily for 10 d. Questionnaires were distributed to 175 individuals who received PEP and were collected back from 131 individuals. One hundred and thirty healthcare workers (74.2%) were included in the questionnaire analysis, excluding one healthcare worker whose questionnaire was inadequately described (Fig. 1).
Details of the healthcare workers who responded to the questionnaire are shown in Table 1. Sixty-one physicians, 44 nurses, and 25 other healthcare workers responded to the questionnaire. Of the healthcare workers analysed, 121 (93.1%) had been vaccinated against influenza before PEP. One hundred and twenty-two healthcare workers (93.8%) had PEPs due to close contact with other healthcare workers without proper personal protective equipment in the hospital.
Table 1. Characteristics of Healthcare Workers
| Number (%) |
|---|
| Population |
| Physicians | 61 (46.9) |
| Nurses | 44 (33.8) |
| Other healthcare workers | 25 (19.2) |
| Administration of influenza vaccine |
| Yes | 121 (93.1) |
| No | 9 (6.9) |
| Close contact with |
| Other healthcare workers | 122 (93.8) |
| Patients | 8 (6.2) |
| Adherence to PEP |
| Complete | 48 (36.9) |
| Incomplete | 82 (63.1) |
Of the subjects analysed, 82 (73.1%) did not complete the PEP regimen. Physicians (21.3%) had significantly lower adherence than nurses (54.5%) and other healthcare workers (44.0%) (Fig. 2a) (p < 0.01, p = 0.19, respectively). The median duration of treatment with oseltamivir was 6 d (interquartile range (IQR): 3.75–10) in all subjects and 5 d (IQR: 3–5) in the non-adherence group (Fig. 2b). Multiple logistic regression analysis revealed that physicians (β: 1.53, odds ratio: 4.62, 95% confidence interval (CI): 2.08–10.25) and non-vaccination (β: 2.26, odds ratio: 9.60, 95% CI: 1.12–82.25) were the independent factors for non-adherence to PEP (Table 2). Of the 82 non-adherence healthcare workers, 47 (57.3%) stated the reason for discontinuing PEP (Table 3). Among them, 36 (76.6%)—including 25 physicians, 6 nurses, and 5 other healthcare workers—stated that they forgot to take the medication or discontinued it due to a misguided self-decision that continuation of PEP was not necessary. Five (10.6%) healthcare workers discontinued PEP due to adverse effects of oseltamivir. Dizziness and drowsiness were expressed in two patients, and palpitations, fatigue, chills, and headaches were expressed in one patient.
Table 2. Factors of Non-adherence to PEP
| Factors | β | Odds ratio | 95% CI | p-Value |
|---|
| Physicians | 1.53 | 4.62 | 2.08–10.25 | <0.01 |
| Non-vaccination | 2.26 | 9.60 | 1.12–82.25 | 0.039 |
| Close contact with healthcare workers | −0.76 | 0.47 | 0.082–2.63 | 0.39 |
CI: confidence interval; PEP, post-exposure prophylaxis.
Table 3. Reasons for Non-adherence to PEP
| Reasonsa) | Number (%) |
|---|
| Forgetting to take | 20 (42.6) |
| Stopping due to misguided self-decision | 16 (34.0) |
| Afraid of the adverse effects of anti-influenza agents | 6 (12.8) |
| Occurrence of adverse effects (multiple answers allowed) | 5 (10.6) |
| Dizziness | 2 |
| Drowsiness | 2 |
| Palpitations | 1 |
| Fatigue | 1 |
| Chills | 1 |
| Headaches | 1 |
a) Forty-seven healthcare workers answered. PEP, post-exposure prophylaxis.
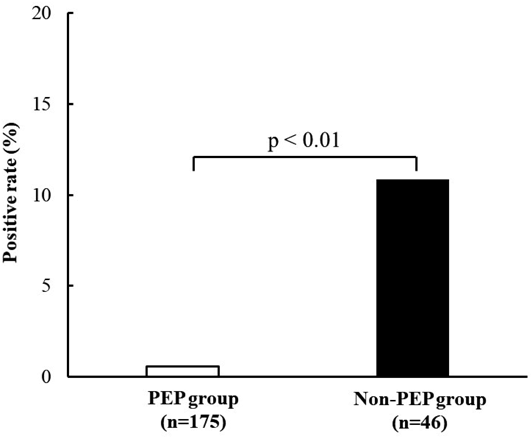
In the PEP (n = 175) and non-PEP groups (n = 46), the number of healthcare workers diagnosed with influenza within 10 d after close contact with indexed cases was 1 (0.6%) in the PEP group and 5 (10.9%) in the non-PEP group (Fig. 3); a significant difference was observed between the two groups (p < 0.01).
DISCUSSION
This analysis showed that the adherence to PEP with oseltamivir among healthcare workers was low, especially among physicians, and that the primary factor for preventing PEP adherence was self-directed discontinuation of PEP.
Our retrospective study showed that the adherence to PEP with oseltamivir treatment was low in healthcare workers. Belmaker et al.13) reported that adherence to PEP with oseltamivir treatment during the H5N1 avian influenza outbreak in Israel was 87.6%, and adherence to PEP was higher than that in the present results. This may be because our study focused on PEP for a seasonal influenza outbreak, whereas their report focused on PEP for the global outbreak of avian influenza, which may lead to differences in the risk cognition of influenza outbreaks among healthcare workers. The Japanese have lower adherence to oral medication than other racial groups, and the low adherence in the present study may be a racial factor.14) When PEP with oseltamivir is implemented in healthcare workers who are asymptomatic and have less risk cognition of the outbreaks, we need to be aware that adherence to oseltamivir treatment may be poor. In this analysis, the most common reasons for discontinuation of PEP were forgetting to take oseltamivir or stopping PEP due to misguided self-decisions that continuation of PEP was not necessary. Although the physician who was a member of the hospital infection control committee had explained the details of PEP such as its purpose and dosage of oseltamivir at the start of PEP, adherence to oseltamivir may have been low because of an inadequate understanding of the significance of PEP. This indicates that medication education, including the significance of taking anti-influenza agents for PEP, is important to increase PEP adherence.
In our study, physicians had significantly lower adherence compared with other healthcare workers; physicians were an independent factor of non-adherence to PEP (Fig. 2a, Table 2). This finding suggests that the risk of non-adherence to PEP may differ between occupations. The most common reason for non-adherence among physicians was forgetting to take the drug or discontinuation due to misguided self-decision (25 physicians (89.3%) stated this as the reason for discontinuing PEP). Therefore, continuous medication monitoring to check for adherence to PEP may be required for physicians for PEP completion. For monitoring PEP adherence, a web application may be useful because of its continuity and immediacy. Moreover, our study revealed that non-vaccination was an independent factor of non-adherence to PEP (Table 2). This indicates that the healthcare workers with low adherence to vaccination have poor adherence to PEP as well. In the 2016/2017 season, the period of this analysis, influenza vaccination was voluntary at our institution. During the same period, there were no cases wherein applicants could not be vaccinated because of allergies. No specific education on infection prevention was provided to healthcare workers who did not receive influenza vaccinations. Thus, healthcare workers who had not been vaccinated may have been less aware of infection prevention in this study. Such workers, being at a higher risk for influenza, may require closer observation and intervention than the others. In this analysis, a large number of healthcare workers needed PEP because they did not wear personal protective equipment properly. Proper use of personal protective equipment is necessary to reduce the need for PEP. Additionally, educating healthcare workers to wear appropriate personal protective equipment during an influenza epidemic is important.15)
In this study, 10.6% of the healthcare workers discontinued PEP because of adverse effects of oseltamivir. Kato et al.16) reported that the incidence of adverse effects of anti-influenza agents in PEP was 22.5%, which was slightly higher than that in our study. On the other hand, whereas gastrointestinal symptoms were common adverse events in PEP in the previous reports,16) these symptoms were not reported in the present study—with atypical adverse effects of oseltamivir such as dizziness and drowsiness being mainly reported. These adverse events may not have occurred due to oseltamivir but may be symptoms associated with influenza. Nevertheless, in this study, 6 (12.8%) healthcare workers discontinued PEP because of fear of the adverse events of oseltamivir. The initial symptoms of adverse effects of anti-influenza agents need to be explained carefully to remove the anxiety associated with PEP. No previous studies have analysed the reasons for non-adherence to PEP, and this study is the first to elucidate the causes of poor PEP adherence.
Despite the lower adherence to oseltamivir treatment in the PEP group, the positive rate of influenza within 10 d after close contact with a person with influenza in the PEP group was significantly lower than that in the non-PEP group. In this analysis, once-daily oseltamivir was administered for 10 d as a PEP regimen. Previous reports indicated that the maximum virus excretion occurs 1–3 d after the onset of influenza.17,18) Previous studies also showed that short-term PEP regimens in which oseltamivir is administered only for 3 or 5 d have been effective in preventing infection with influenza.19,20) A significantly lower positive rate of influenza was observed in the PEP group, even though approximately 25% of the PEP group had discontinued PEP by day 3, and approximately 50% had discontinued PEP by day 5 in this study (Figs. 2b, 3). This indicates that a short-term regimen of oseltamivir for 3–5 d as a PEP for healthcare workers may be effective. However, it is unclear whether the occurrence of influenza infection in this analysis was caused by close contact with index cases or not. Moreover, the accurate vaccination status between the two groups was unclear. The usefulness of short-term PEP needs to be further investigated.
This study has several limitations. First, this is a retrospective single-centre study, and adherence to PEP may be influenced by institutional bias. A multicentre study is needed to analyse PEP adherence in more detail. Second, we did not analyse sex, age, and comorbidities, as well as other factors related to poor adherence. Age differences may have affected adherence to oseltamivir treatment for PEP.21) Third, in this study, anti-influenza agents other than oseltamivir were not used as PEP, and adherence to PEP using other anti-influenza agents remains unknown. Laninamivir is an anti-influenza agent that completes PEP in a shorter period than oseltamivir.22,23) Moreover, single-dose baloxavir showed significant PEP efficacy in preventing influenza in household contacts of patients with influenza.24) Although these drugs can be expected to have high adherence, they are more expensive than oseltamivir. Anti-influenza agents with a PEP should be inexpensive as the PEP is administered to a large number of healthcare workers. Fourth, although 46 patients did not consent to PEP in this analysis, we could not analyse the vaccination or prescription status of anti-influenza drugs at other hospitals for the non-PEP group. Given the high rate of subsequent influenza positivity among the non-PEP group, education about the risk of nosocomial infection should be provided to them. Further, it would be useful to provide guidance on the necessity of prophylactic administration of anti-influenza agents and infection prevention methods not only from physicians but also from pharmacists, nurses, and other professionals. Finally, we were unable to analyse the development of oseltamivir resistance in the influenza virus among healthcare workers diagnosed with influenza. Whether infection with the oseltamivir-resistant influenza virus occurred in our study is unknown. Outbreaks of the oseltamivir-resistant influenza virus have occurred in Japan, and the emergence of resistant viruses should be noted.25,26)
CONCLUSION
This study revealed that the adherence to PEP with oseltamivir among healthcare workers was low, especially among physicians. The most common reason for PEP interruption was forgetting to take the medication or stopping the medication due to a misguided self-decision that continuation of PEP was not necessary. To maximize the therapeutic benefits of PEP, medication education should be provided to ensure treatment compliance when PEP is administered. Moreover, proper use of personal protective equipment is necessary to reduce the need for PEP.
Acknowledgments
This study was supported by JSPS KAKENHI (Grant No. 19K16414).
Conflict of Interest
The authors declare no conflict of interest.
Supplementary Materials
The online version of this article contains supplementary materials.
REFERENCES
- 1) Smieszek T, Lazzari G, Salathe M. Assessing the dynamics and control of droplet- and aerosol-transmitted influenza using an indoor positioning system. Sci. Rep., 9, 2185 (2019).
- 2) Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, Fukuda K. Influenza-associated hospitalizations in the United States. JAMA, 292, 1333–1340 (2004).
- 3) Rule AM, Apau O, Ahrenholz SH, Brueck SE, Lindsley WG, de Perio MA, Noti JD, Shaffer RE, Rothman R, Grigorovitch A, Noorbakhsh B, Beezhold DH, Yorio PL, Perl TM, Fisher EM. Healthcare personnel exposure in an emergency department during influenza season. PLOS ONE, 13, e0203223 (2018).
- 4) Jefferson T, Rivetti D, Rivetti A, Rudin M, Di Pietrantonj C, Demicheli V. Efficacy and effectiveness of influenza vaccines in elderly people: a systematic review. Lancet, 366, 1165–1174 (2005).
- 5) Monto AS, Hornbuckle K, Ohmit SE. Influenza vaccine effectiveness among elderly nursing home residents: a cohort study. Am. J. Epidemiol., 154, 155–160 (2001).
- 6) Seki Y, Onose A, Sugaya N. Influenza vaccine effectiveness in adults based on the rapid influenza diagnostic test results, during the 2015/16 season. J. Infect. Chemother., 23, 615–620 (2017).
- 7) Belongia EA, Simpson MD, King JP, Sundaram ME, Kelley NS, Osterholm MT, McLean HQ. Variable influenza vaccine effectiveness by subtype: a systematic review and meta-analysis of test-negative design studies. Lancet Infect. Dis., 16, 942–951 (2016).
- 8) Hagihara M, Kato Y, Kurumiya A, Takahashi T, Sakata M, Kato H, Sakanashi D, Yamada A, Suematsu H, Hirai J, Nishiyama N, Koizumi Y, Yamagishi Y, Mikamo H. The prophylactic effect of anti-influenza agents for an influenza outbreak in a university hospital. Intern. Med., 57, 497–501 (2018).
- 9) Uyeki TM, Bernstein HH, Bradley JS, Englund JA, File TM Jr, Fry AM, Gravenstein S, Hayden FG, Harper SA, Hirshon JM, Ison MG, Johnston BL, Knight SL, McGeer A, Riley LE, Wolfe CR, Alexander PE, Pavia AT. Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin. Infect. Dis., 68, e1–e47 (2019).
- 10) Welliver R, Monto AS, Carewicz O, Schatteman E, Hassman M, Hedrick J, Jackson HC, Huson L, Ward P, Oxford JS. Effectiveness of oseltamivir in preventing influenza in household contacts: a randomized controlled trial. JAMA, 285, 748–754 (2001).
- 11) Hayden FG, Belshe R, Villanueva C, Lanno R, Hughes C, Small I, Dutkowski R, Ward P, Carr J. Management of influenza in households: a prospective, randomized comparison of oseltamivir treatment with or without postexposure prophylaxis. J. Infect. Dis., 189, 440–449 (2004).
- 12) Shinjoh M, Takano Y, Takahashi T, Hasegawa N, Iwata S, Sugaya N. Postexposure prophylaxis for influenza in pediatric wards oseltamivir or zanamivir after rapid antigen detection. Pediatr. Infect. Dis. J., 31, 1119–1123 (2012).
- 13) Belmaker I, Lyandres M, Bilenko N, Dukhan L, Mendelson E, Mandelboim M, Shahar-Rotberg L, Bitran E, Yossef Y, Grotto I. Adherence with oseltamivir chemoprophylaxis among workers exposed to poultry during avian influenza outbreaks in southern Israel. Int. J. Infect. Dis., 13, 261–265 (2009).
- 14) Pechère JC, Hughes D, Kardas P, Cornaglia G. Non-compliance with antibiotic therapy for acute community infections: a global survey. Int. J. Antimicrob. Agents, 29, 245–253 (2007).
- 15) Fiore AE, Fry A, Shay D, Gubareva L, Bresee JS, Uyeki TM. Antiviral agents for the treatment and chemoprophylaxis of influenza—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep., 60, 1–24 (2011).
- 16) Kato H, Hagihara M, Kato Y, Kurumiya A, Takahashi T, Sakata M, Nishiyama N, Asai N, Koizumi Y, Furui T, Yamagishi Y, Mikamo H. Adverse events of prophylactic anti-influenza agents in medical staffs. J. Infect. Chemother., 23, 683–686 (2017).
- 17) Ip DKM, Lau LLH, Chan KH, Fang VJ, Leung GM, Peiris MJS, Cowling BJ. The dynamic relationship between clinical symptomatology and viral shedding in naturally acquired seasonal and pandemic influenza virus infections. Clin. Infect. Dis., 62, 431–437 (2016).
- 18) Lau LL, Cowling BJ, Fang VJ, Chan KH, Lau EH, Lipsitch M, Cheng CK, Houck PM, Uyeki TM, Peiris JS, Leung GM. Viral shedding and clinical illness in naturally acquired influenza virus infections. J. Infect. Dis., 201, 1509–1516 (2010).
- 19) Lepen L, Blagus R, Veluscek M, Saletinger R, Petrovec M, Bajrovic FF, Stupica D. Five-day vs. 10-day postexposure chemoprophylaxis with oseltamivir to prevent hospital transmission of influenza: a noninferiority randomized open-label study. Open Forum Infect. Dis., 7, ofaa240 (2020).
- 20) Ishiguro N, Oyamada R, Nasuhara Y, Yamada T, Miyamoto T, Imai S, Akizawa K, Fukumoto T, Iwasaki S, Iijima H, Ono K. Three-day regimen of oseltamivir for postexposure prophylaxis of influenza in wards. J. Hosp. Infect., 94, 150–153 (2016).
- 21) Skrabal Ross X, Gunn KM, Suppiah V, Patterson P, Olver I. A review of factors influencing non-adherence to oral antineoplastic drugs. Support. Care Cancer, 28, 4043–4050 (2020).
- 22) Kashiwagi S, Watanabe A, Ikematsu H, Awamura S, Okamoto T, Uemori M, Ishida K. Laninamivir octanoate for post-exposure prophylaxis of influenza in household contacts: a randomized double blind placebo controlled trial. J. Infect. Chemother., 19, 740–749 (2013).
- 23) Kashiwagi S, Watanabe A, Ikematsu H, Uemori M, Awamura S. Long-acting neuraminidase inhibitor laninamivir octanoate as post-exposure prophylaxis for influenza. Clin. Infect. Dis., 63, 330–337 (2016).
- 24) Ikematsu H, Hayden FG, Kawaguchi K, Kinoshita M, de Jong MD, Lee N, Takashima S, Noshi T, Tsuchiya K, Uehara T. Baloxavir marboxil for prophylaxis against influenza in household contacts. N. Engl. J. Med., 383, 309–320 (2020).
- 25) Takashita E, Kiso M, Fujisaki S, Yokoyama M, Nakamura K, Shirakura M, Sato H, Odagiri T, Kawaoka Y, Tashiro M. Characterization of a large cluster of influenza A(H1N1)pdm09 viruses cross-resistant to oseltamivir and peramivir during the 2013–2014 influenza season in Japan. Antimicrob. Agents Chemother., 59, 2607–2617 (2015).
- 26) Fujita M, Matsumoto H, Inafuku Y, Toyama J, Fujita J. A retrospective observational study of the treatment of a nosocomial infection caused by oseltamivir-resistant influenza virus A with baloxavir marboxil. Respir. Investig., 58, 403–408 (2020).