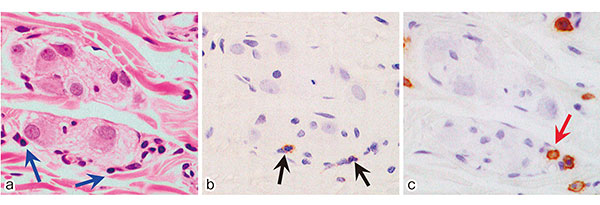
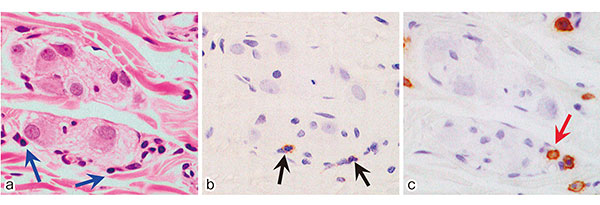
Objectives: To assess the predictive values of myenteric and submucosal plexitis for postoperative endoscopic recurrence of Crohn's disease (CD). Methods: A retrospective study of CD patients who underwent intestinal resection between 1995 and 2013 in the Department of Surgery 2, Tokyo Women's Medical University was performed. Proximal resection margins were analyzed and plexitis was evaluated by counting the number of inflammatory cells in myenteric and submucosal plexuses. The sizes of the most severely inflamed ganglion (MIG) were measured. Multiple regression analysis was used to identify independent risk factors for postoperative endoscopic recurrence. Results: Of the 51 included patients, 40 patients underwent colonoscopy after surgery. Endoscopic recurrence was observed in 21 patients (52.5%). Mean duration (±standard deviation) from surgery to recurrence was 49.7±34.7 months. Endoscopic recurrence rates at 1, 3, and 5 years were 5.0%, 24.1%, and 45.1%, respectively. Submucosal plexitis and myenteric plexitis were observed in 36 (90.0%) and 37 patients (92.5%), respectively. On multivariate analysis, initial intestinal resection, rate of plexitis <50%, size of the MIG in the myenteric plexus ≥867 μm2, and total number of inflammatory cells in the submucosal plexus ≥8 were independent risk factors for postoperative endoscopic recurrence. Conclusions: Pathological findings of proximal resection margins, especially submucosal plexitis and large sizes of myenteric plexus, are predictive of postoperative endoscopic recurrence in CD.
View full abstract