Objectives: The pre-operative diagnostic value of detecting lateral pelvic lymph node (LPLN) metastasis with magnetic resonance imaging, multidirectory computed tomography, and positron emission tomography/computed tomography was investigated in lower rectal cancer patients.
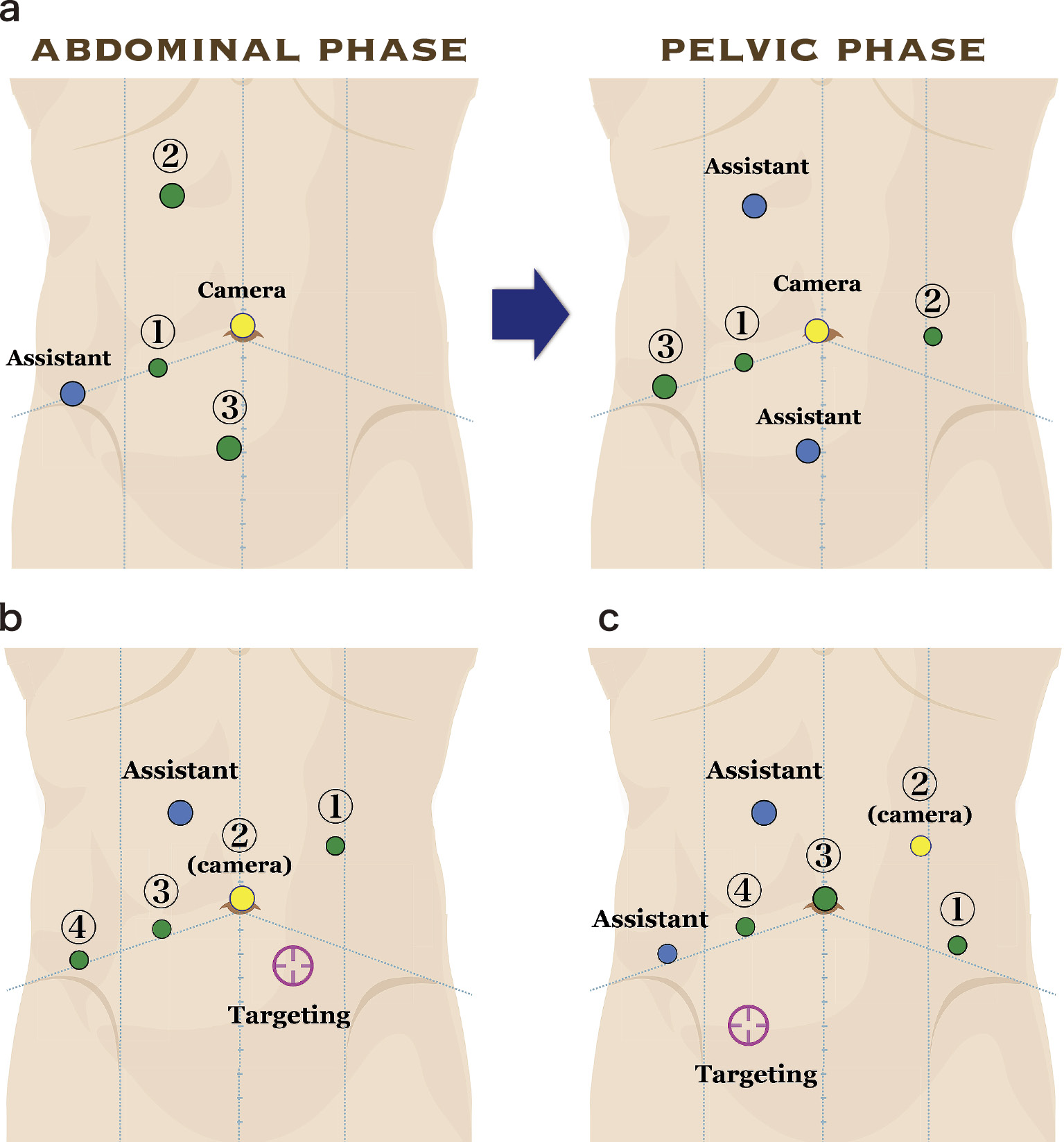
Methods: We retrospectively evaluated, using the three different modalities, the metastatic status of LPLNs in four regions, including both the internal iliac and the obturator, in 46 patients affected by lower rectal cancer patients who underwent LPLN dissection. The size inclusion criterion for LPLN metastasis was set at 6 mm in the short axis diameter. Histological examination was performed for determining the false positive and negative rate of LPLNs metastasis detection.
Results: Among 184 LPLNs regions, 17 (9%) were positive for metastasis. The region-based sensitivity, specificity, and accuracy rate did not differ among the three tested diagnostic modalities. Moreover, a significant increase in these rates could not be observed when the modalities were combined. Of 184 regions, 8 (4.4%) were false negative, whereas 2 (1.1%) were false positive. The histological pattern of metastatic regions did not differ in 8 false negative LPLNs.
Conclusions: Each modality had a similar detection power for LPLNs metastasis, with a cut-off value at 6 mm in the short axis diameter. However, the sensitivity of all the modalities was slightly low, along with the number of false negative LPLNs. Further reduction of the false negative rate with these modalities may be difficult because of an inherent limitation of current imaging technologies to accurately detect lymph node metastases.
View full abstract