Volume 54
Displaying 1-49 of 49 articles from this issue
- |<
- <
- 1
- >
- >|
-
1999 Volume 54 Pages 1-11
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (11424K)
Clinical study
-
1999 Volume 54 Pages 40-42
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (361K) -
1999 Volume 54 Pages 43-47
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (765K) -
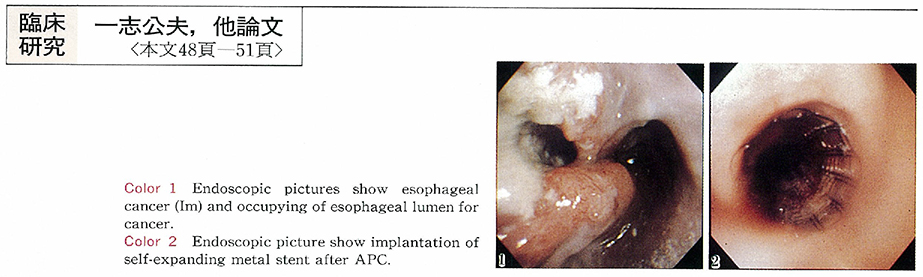
1999 Volume 54 Pages 48-51
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (407K) -
1999 Volume 54 Pages 52-56
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (573K) -
1999 Volume 54 Pages 57-61
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1337K)
Case report
-
A Case of Esophageal Web in Plummer-Vinson Syndrome Treated by Endoscopic Balloon Dilatation Therapy1999 Volume 54 Pages 62-64
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (677K) -
1999 Volume 54 Pages 65-68
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (782K) -
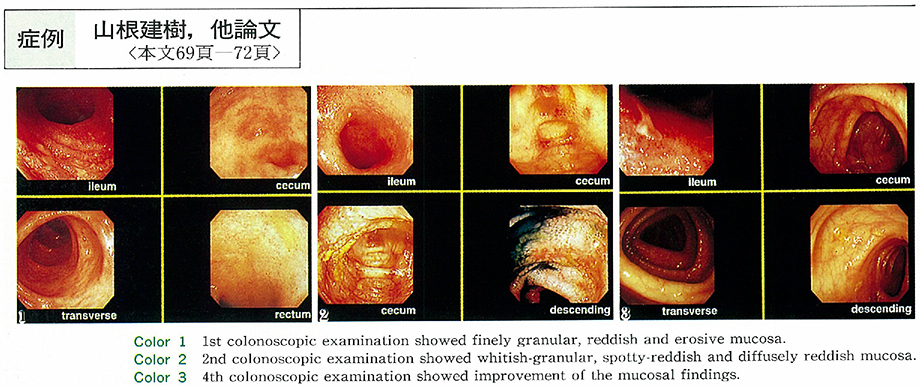
1999 Volume 54 Pages 69-72
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (897K) -
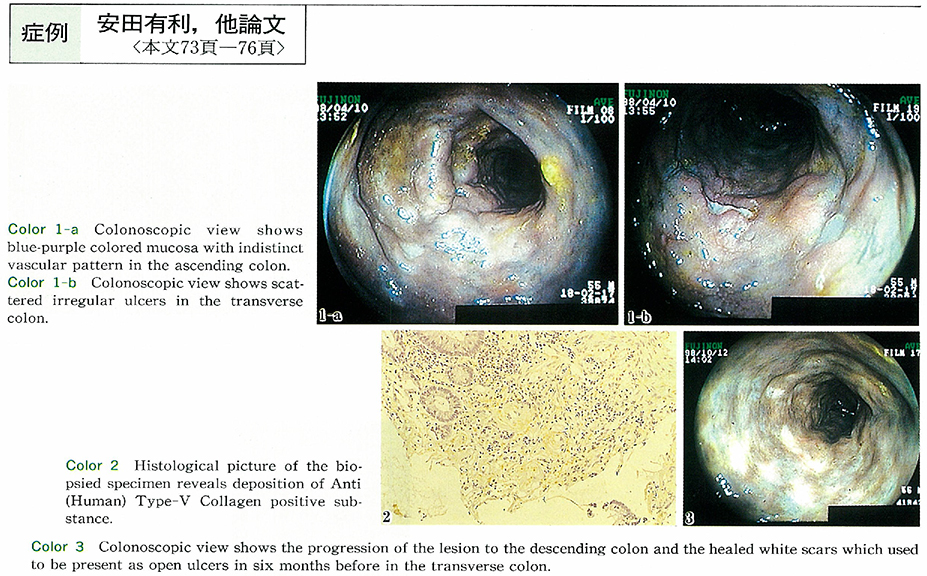
1999 Volume 54 Pages 73-76
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (956K) -
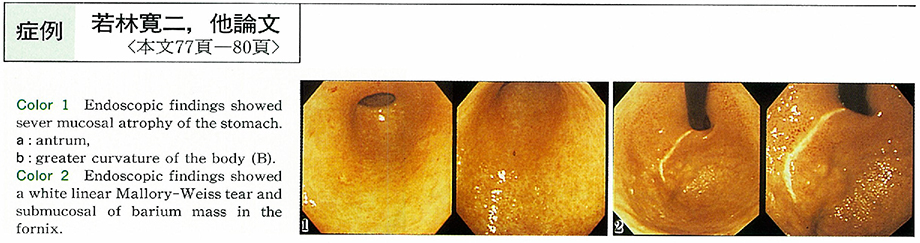
1999 Volume 54 Pages 77-80
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (843K) -
1999 Volume 54 Pages 81-84
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (757K)
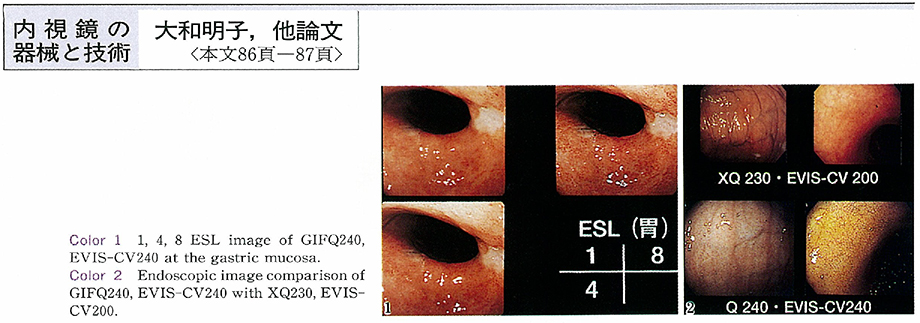
Technology and instrument
-
1999 Volume 54 Pages 86-87
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (257K)
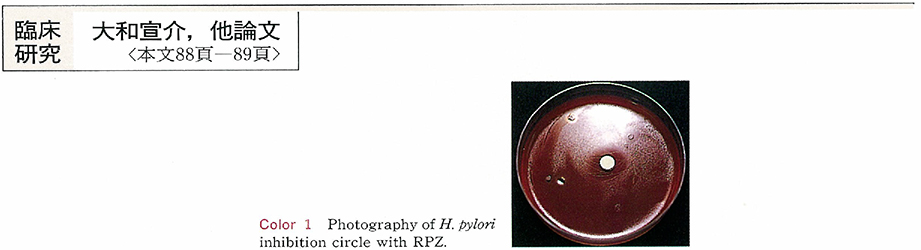
Clinical study
-
1999 Volume 54 Pages 88-89
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (254K) -
1999 Volume 54 Pages 90-91
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (263K) -
1999 Volume 54 Pages 92-93
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (240K) -
1999 Volume 54 Pages 94-95
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (409K) -
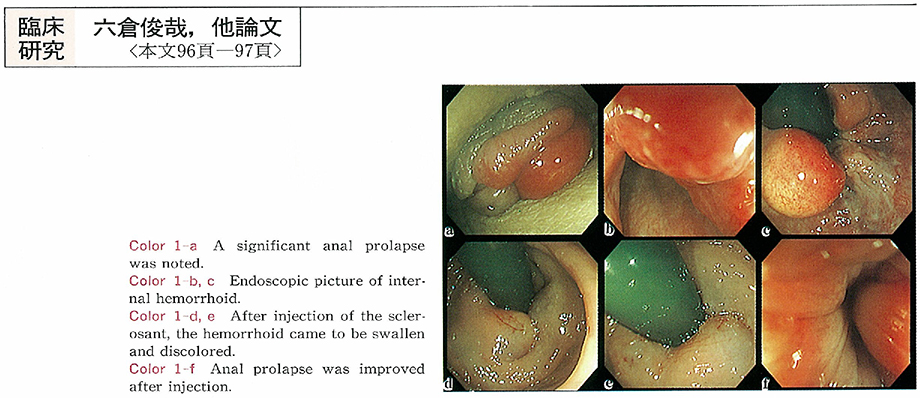
1999 Volume 54 Pages 96-97
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (249K) -
1999 Volume 54 Pages 98-99
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (251K) -
1999 Volume 54 Pages 100-101
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (154K)
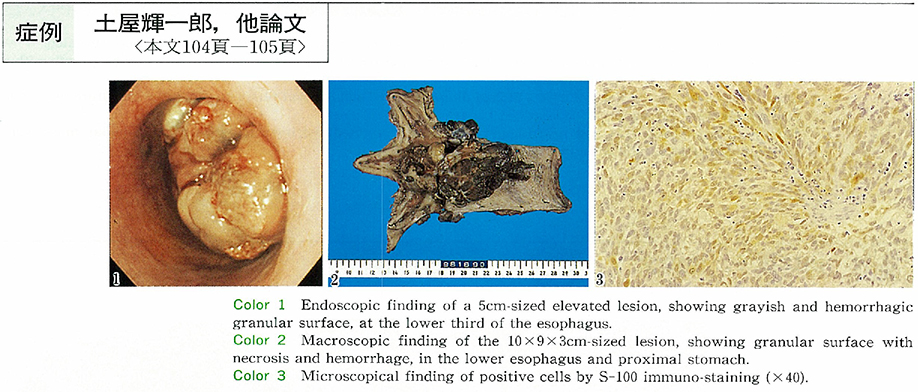
Case report
-
1999 Volume 54 Pages 102-103
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1038K) -
1999 Volume 54 Pages 104-105
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (914K) -
1999 Volume 54 Pages 106-107
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (714K) -
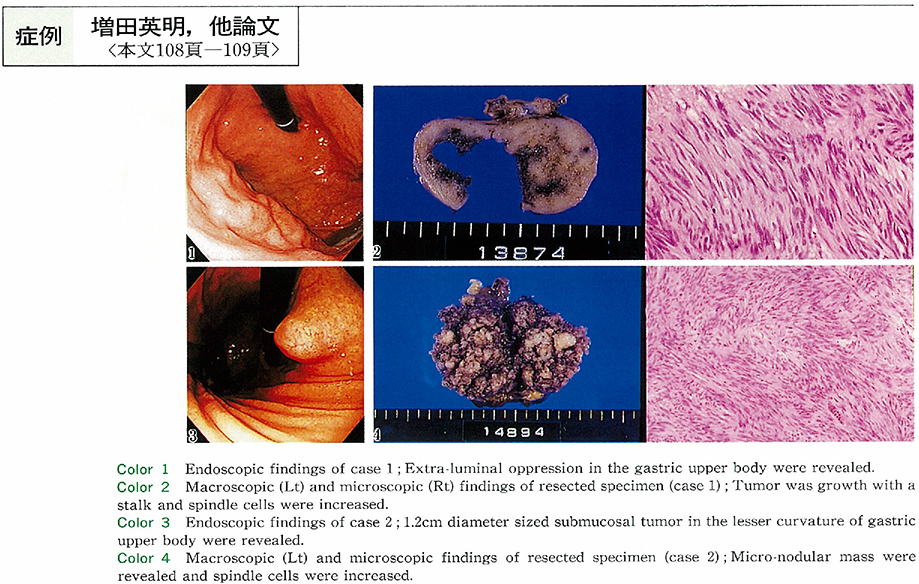
1999 Volume 54 Pages 108-109
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (567K) -
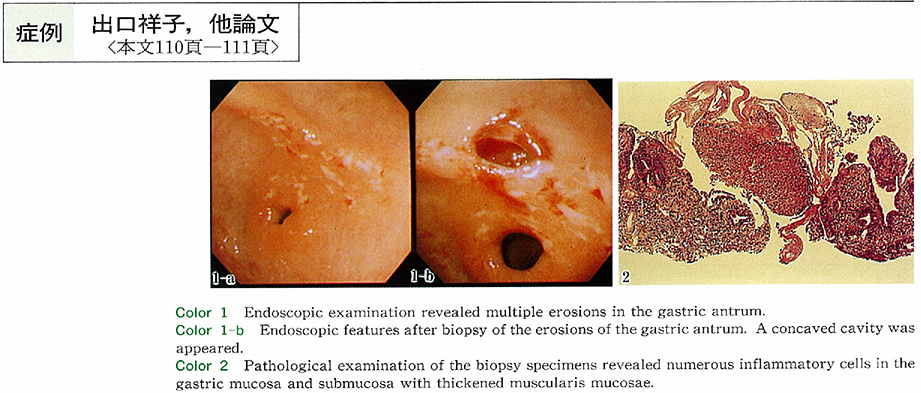
1999 Volume 54 Pages 110-111
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (402K) -
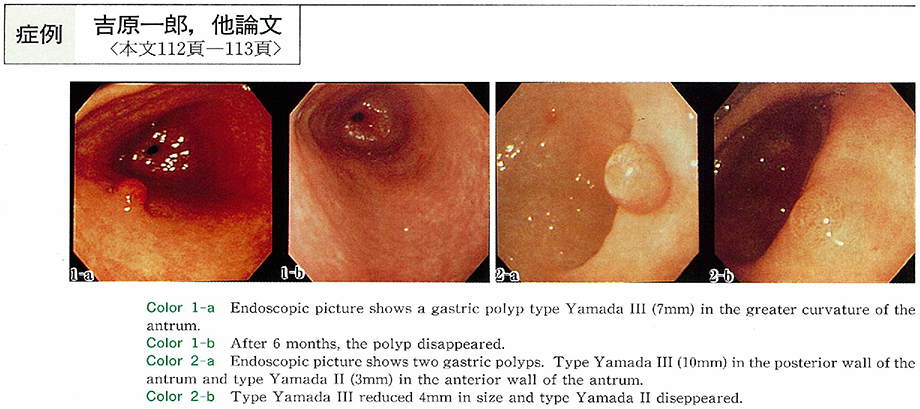
1999 Volume 54 Pages 112-113
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (456K) -
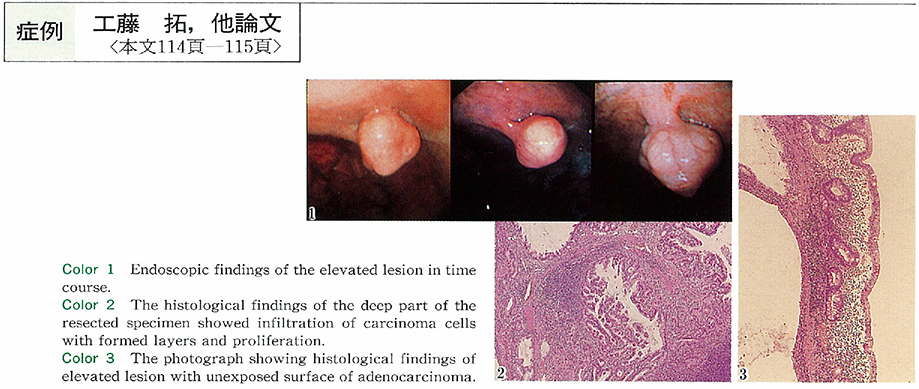
1999 Volume 54 Pages 114-115
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1028K) -
1999 Volume 54 Pages 116-117
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (470K) -
1999 Volume 54 Pages 118-119
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (494K) -
1999 Volume 54 Pages 120-121
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (277K) -
1999 Volume 54 Pages 122-123
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (537K) -
1999 Volume 54 Pages 124-125
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (652K) -
1999 Volume 54 Pages 126-127
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (569K) -
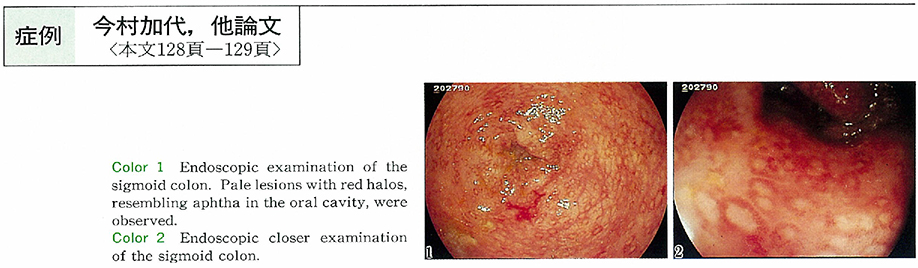
1999 Volume 54 Pages 128-129
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (407K) -
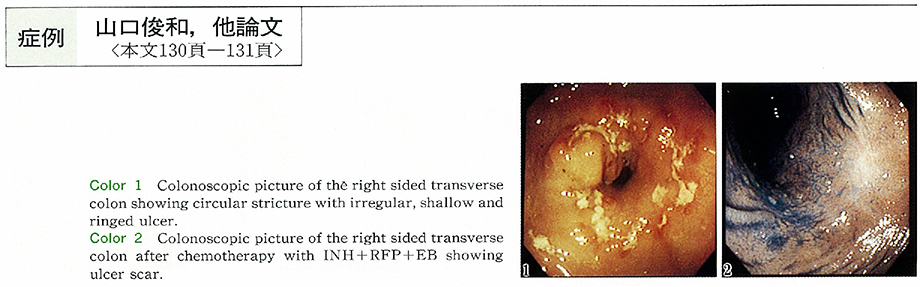
1999 Volume 54 Pages 130-131
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (939K) -
1999 Volume 54 Pages 132-133
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (801K) -
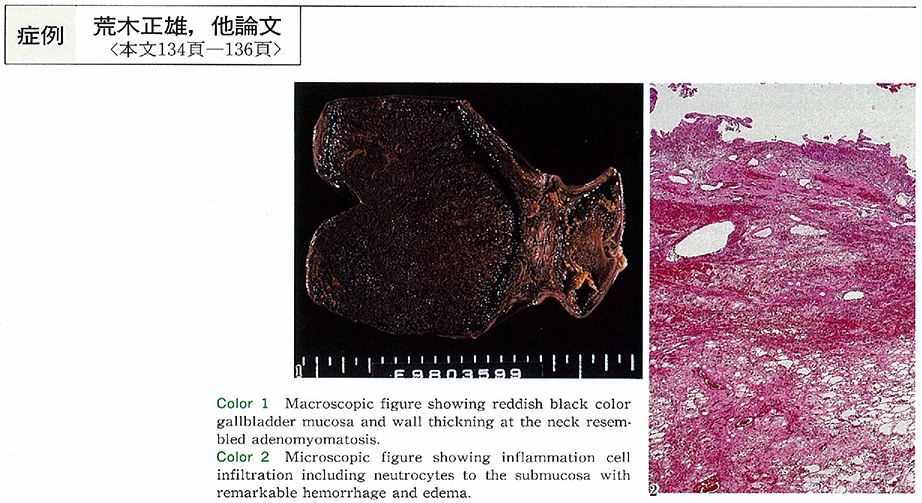
1999 Volume 54 Pages 134-136
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (498K) -
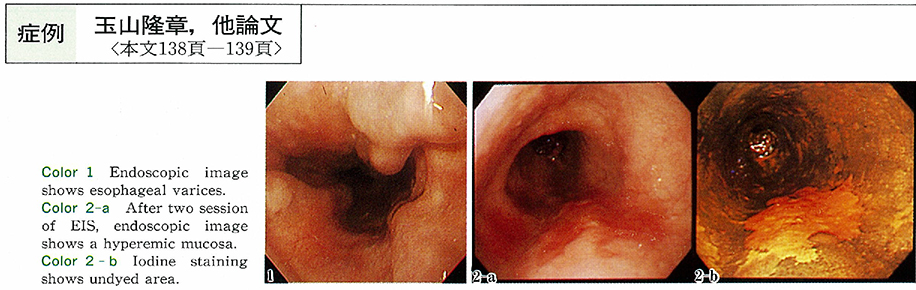
1999 Volume 54 Pages 138-139
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (378K) -
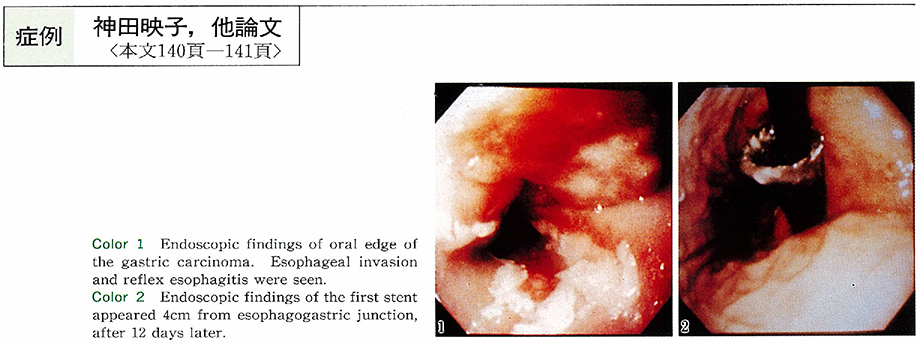
Removal of covered WALLSTENT which was fallen into the stomach lumen using fiberscope, A case report1999 Volume 54 Pages 140-141
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (561K) -
1999 Volume 54 Pages 142-143
Published: August 15, 1999
Released on J-STAGE: October 28, 2014
Download PDF (719K)
-
1999 Volume 54 Pages 144-146
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (1479K)
-
1999 Volume 54 Pages 146-148
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (1010K) -
1999 Volume 54 Pages 149-150
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (300K)
-
1999 Volume 54 Pages 151-152
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (1225K) -
1999 Volume 54 Pages 152-153
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (955K) -
1999 Volume 54 Pages 154-155
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (313K) -
1999 Volume 54 Pages 156-157
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (308K)
-
1999 Volume 54 Pages 158-159
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (315K)
-
1999 Volume 54 Pages 160-193
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (7045K)
- |<
- <
- 1
- >
- >|