Volume 56, Issue 2
Displaying 1-33 of 33 articles from this issue
- |<
- <
- 1
- >
- >|
-
2000 Volume 56 Issue 2 Pages 1-8
Published: 2000
Released on J-STAGE: October 27, 2014
Download PDF (8627K)
Technology and instrument
-
2000 Volume 56 Issue 2 Pages 26-28
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (411K)
Clinical study
-
2000 Volume 56 Issue 2 Pages 29-33
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (610K)
Case report
-
2000 Volume 56 Issue 2 Pages 34-37
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (1590K) -
2000 Volume 56 Issue 2 Pages 38-41
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (659K)
Technology and instrument
-
2000 Volume 56 Issue 2 Pages 42-43
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (241K)
-
2000 Volume 56 Issue 2 Pages 44-45
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (625K)
Clinical study
-
2000 Volume 56 Issue 2 Pages 46-47
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (238K) -
2000 Volume 56 Issue 2 Pages 48-49
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (268K) -
2000 Volume 56 Issue 2 Pages 50-51
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (272K) -
2000 Volume 56 Issue 2 Pages 52-53
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (388K) -
2000 Volume 56 Issue 2 Pages 54-55
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (600K)
Case report
-
2000 Volume 56 Issue 2 Pages 56-57
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (685K) -
2000 Volume 56 Issue 2 Pages 58-59
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (554K) -
2000 Volume 56 Issue 2 Pages 60-61
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (220K) -
2000 Volume 56 Issue 2 Pages 62-63
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (593K) -
2000 Volume 56 Issue 2 Pages 64-65
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (1150K) -
2000 Volume 56 Issue 2 Pages 66-67
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (462K) -
2000 Volume 56 Issue 2 Pages 68-69
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (686K) -
2000 Volume 56 Issue 2 Pages 70-71
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (574K) -
2000 Volume 56 Issue 2 Pages 72-73
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (517K) -
2000 Volume 56 Issue 2 Pages 74-75
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (393K) -
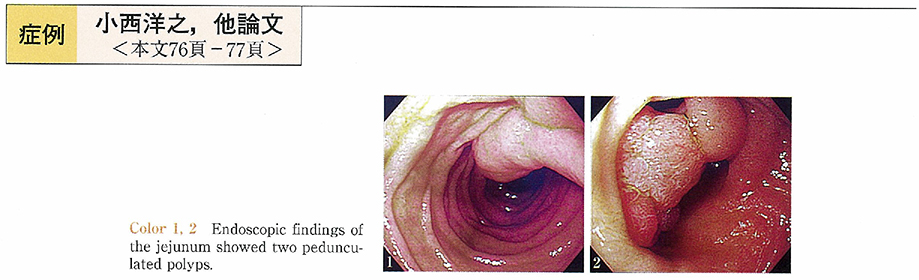
2000 Volume 56 Issue 2 Pages 76-77
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (619K) -
2000 Volume 56 Issue 2 Pages 78-79
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (618K) -
2000 Volume 56 Issue 2 Pages 80-81
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (555K) -
2000 Volume 56 Issue 2 Pages 82-83
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (467K) -
2000 Volume 56 Issue 2 Pages 84-85
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (455K) -
2000 Volume 56 Issue 2 Pages 86-87
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (665K) -
2000 Volume 56 Issue 2 Pages 88-89
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (621K) -
2000 Volume 56 Issue 2 Pages 90-91
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (672K) -
2000 Volume 56 Issue 2 Pages 92-93
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (441K) -
2000 Volume 56 Issue 2 Pages 94-95
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (512K) -
2000 Volume 56 Issue 2 Pages 96-97
Published: May 15, 2000
Released on J-STAGE: October 27, 2014
Download PDF (707K)
- |<
- <
- 1
- >
- >|