Volume 47
Displaying 1-50 of 77 articles from this issue
-
1995 Volume 47 Pages 1-20
Published: 1995
Released on J-STAGE: May 01, 2015
Download PDF (25759K)
Clinical study
-
1995 Volume 47 Pages 48-51
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (497K) -
1995 Volume 47 Pages 52-55
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (442K) -
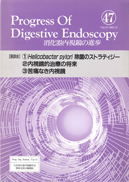
1995 Volume 47 Pages 56-59
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (2055K) -
1995 Volume 47 Pages 60-63
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (649K) -
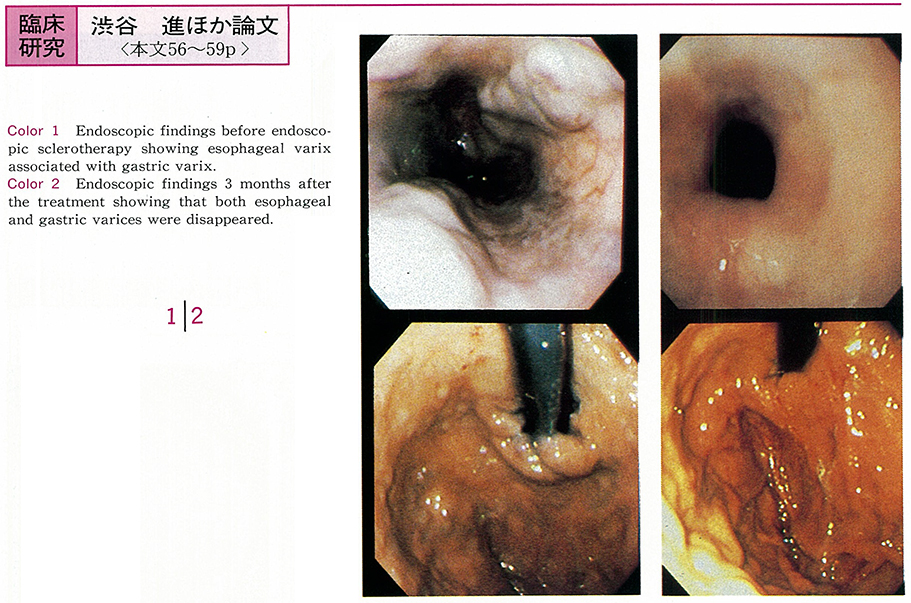
1995 Volume 47 Pages 64-68
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (607K) -
1995 Volume 47 Pages 69-72
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (529K) -
1995 Volume 47 Pages 73-77
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (641K) -
1995 Volume 47 Pages 78-81
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (507K) -
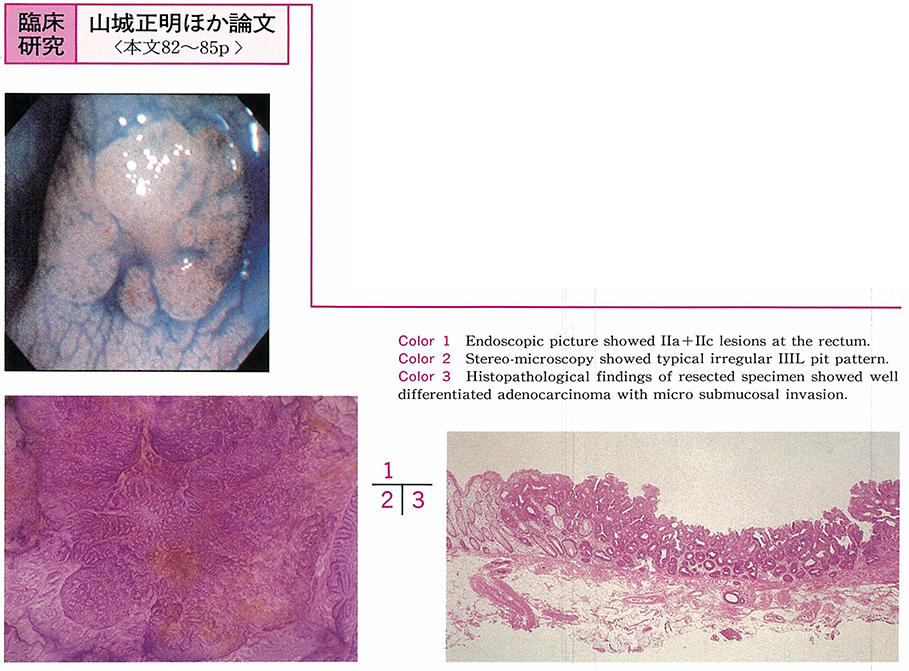
1995 Volume 47 Pages 82-85
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (562K) -
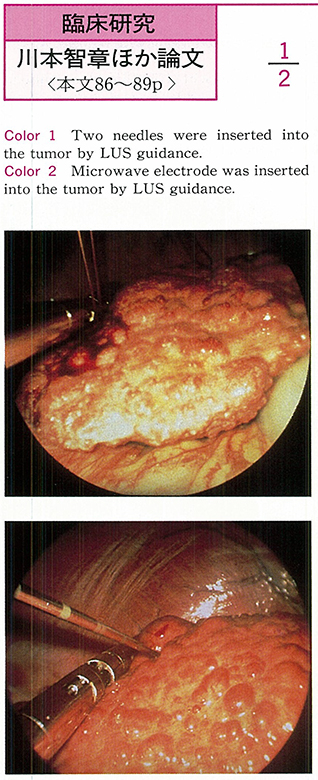
1995 Volume 47 Pages 86-89
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (454K) -
1995 Volume 47 Pages 90-93
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (581K) -
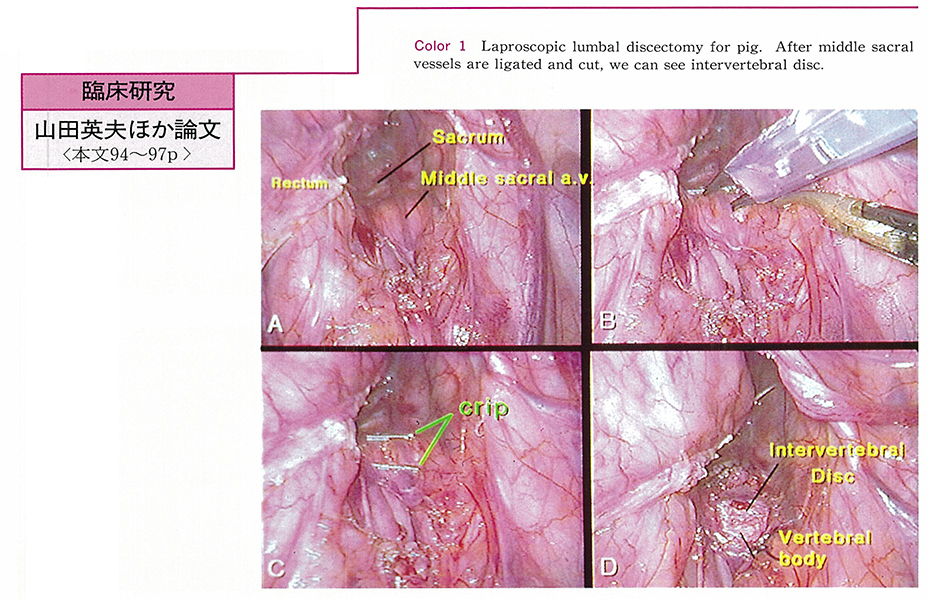
1995 Volume 47 Pages 94-97
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1587K)
Case report
-
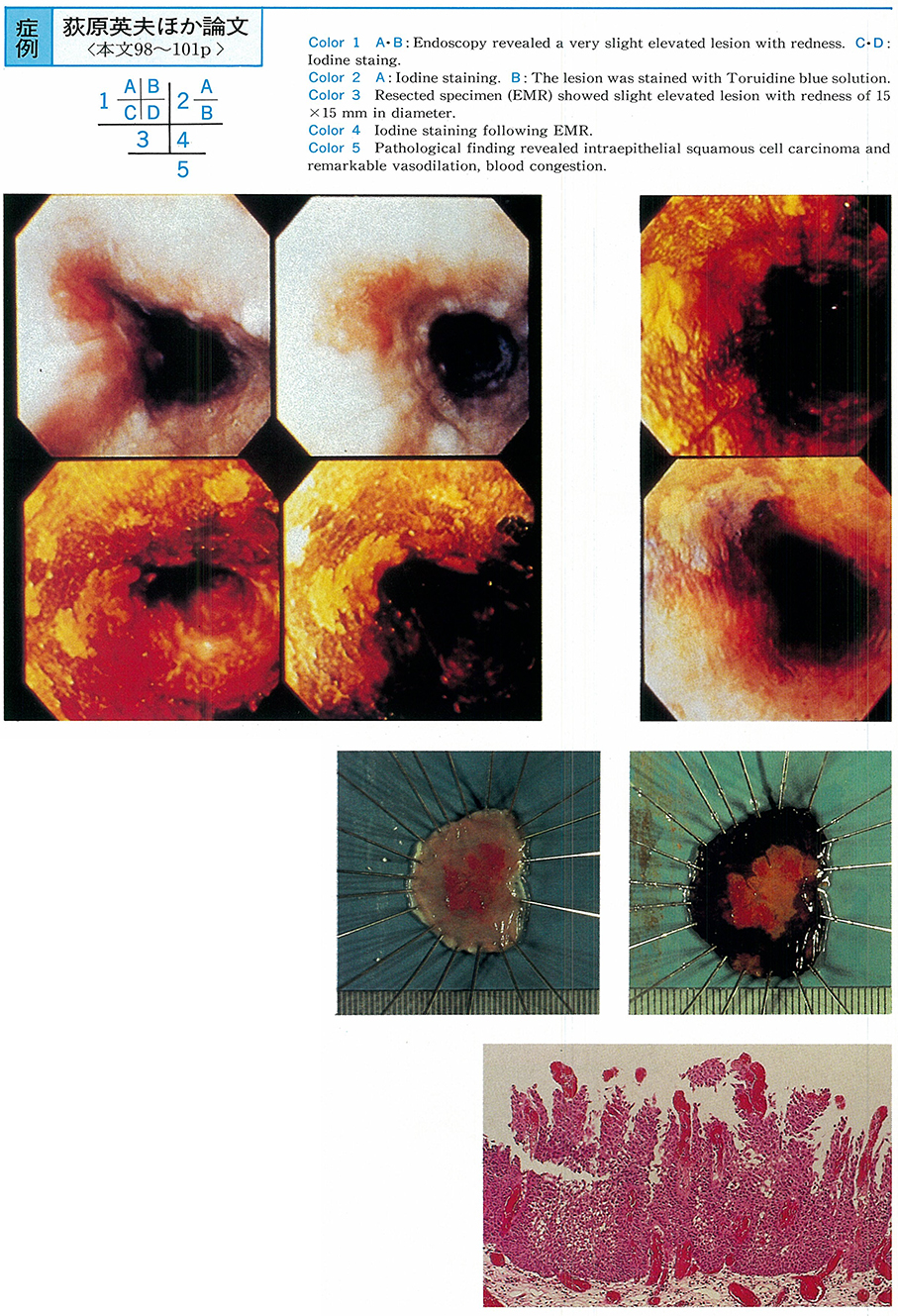
1995 Volume 47 Pages 98-101
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1229K) -
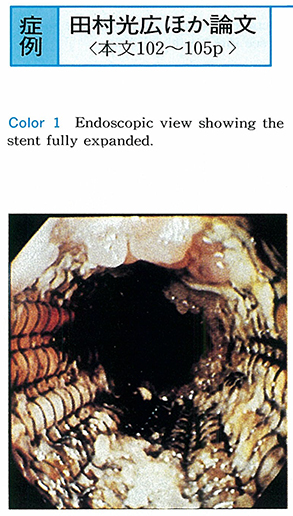
1995 Volume 47 Pages 102-105
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1627K) -
1995 Volume 47 Pages 106-108
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1248K) -
1995 Volume 47 Pages 109-112
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1807K) -
1995 Volume 47 Pages 113-116
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1328K) -
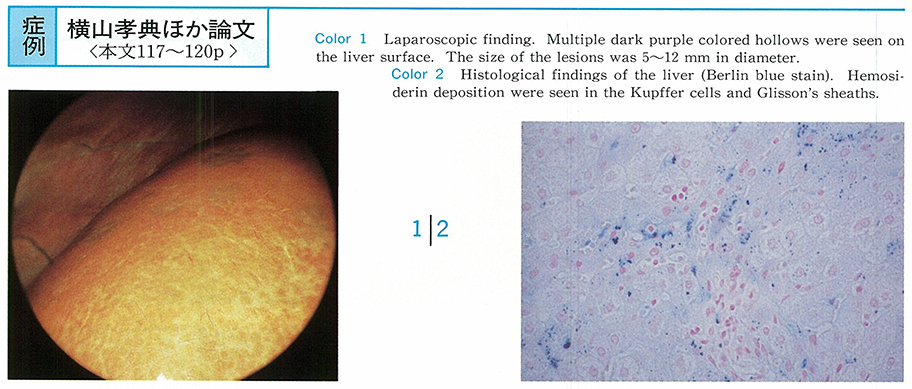
1995 Volume 47 Pages 117-120
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (584K)
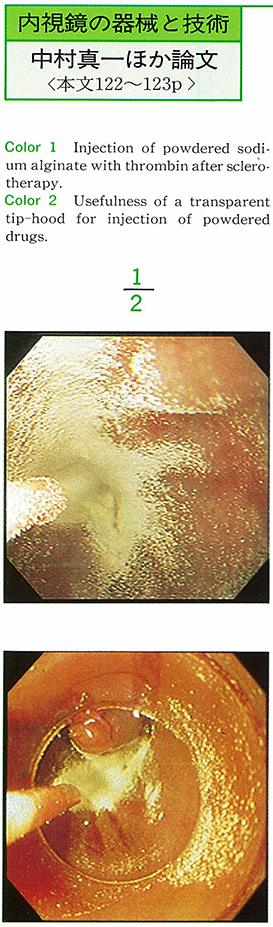
Technology and instrument
-
1995 Volume 47 Pages 122-123
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (733K)
Clinical study
-
1995 Volume 47 Pages 124-125
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (217K) -
1995 Volume 47 Pages 126-127
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (257K) -
1995 Volume 47 Pages 128-129
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (250K) -
1995 Volume 47 Pages 130-131
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (302K) -
1995 Volume 47 Pages 132-133
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (320K) -
1995 Volume 47 Pages 134-135
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (312K) -
1995 Volume 47 Pages 136-137
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (442K) -
1995 Volume 47 Pages 138-139
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (313K) -
1995 Volume 47 Pages 140-141
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (722K) -
1995 Volume 47 Pages 142-143
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (453K) -
1995 Volume 47 Pages 144-145
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (355K) -
1995 Volume 47 Pages 146-147
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (245K) -
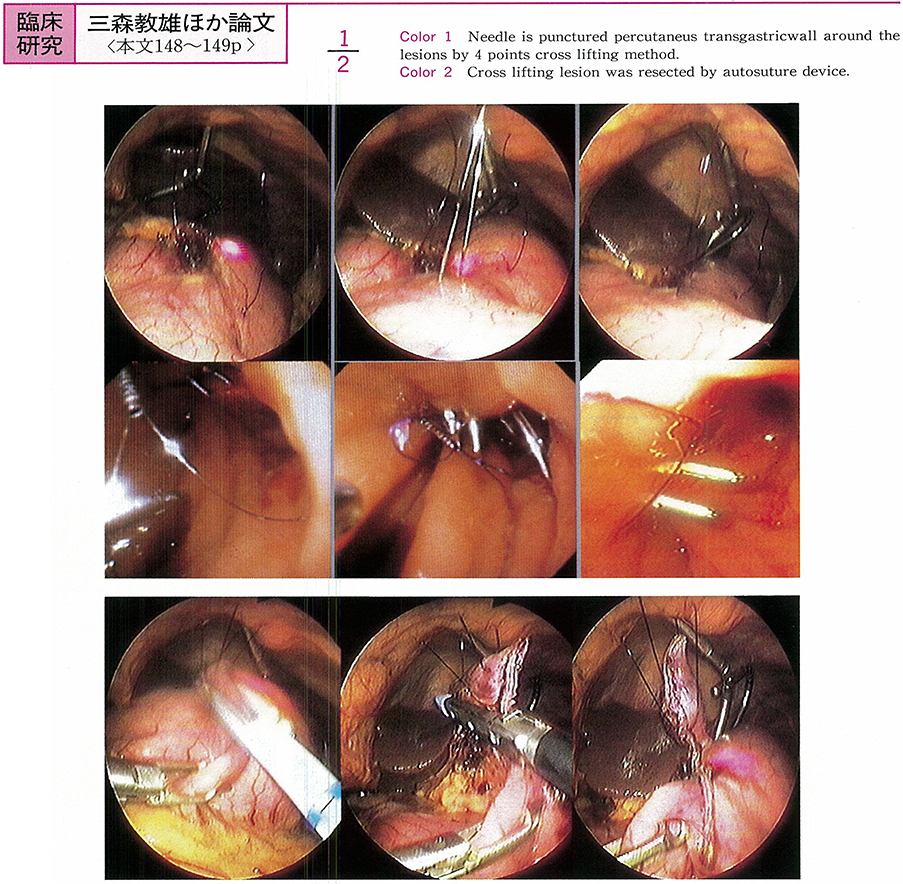
1995 Volume 47 Pages 148-149
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1048K)
Case report
-
1995 Volume 47 Pages 150-151
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (228K) -
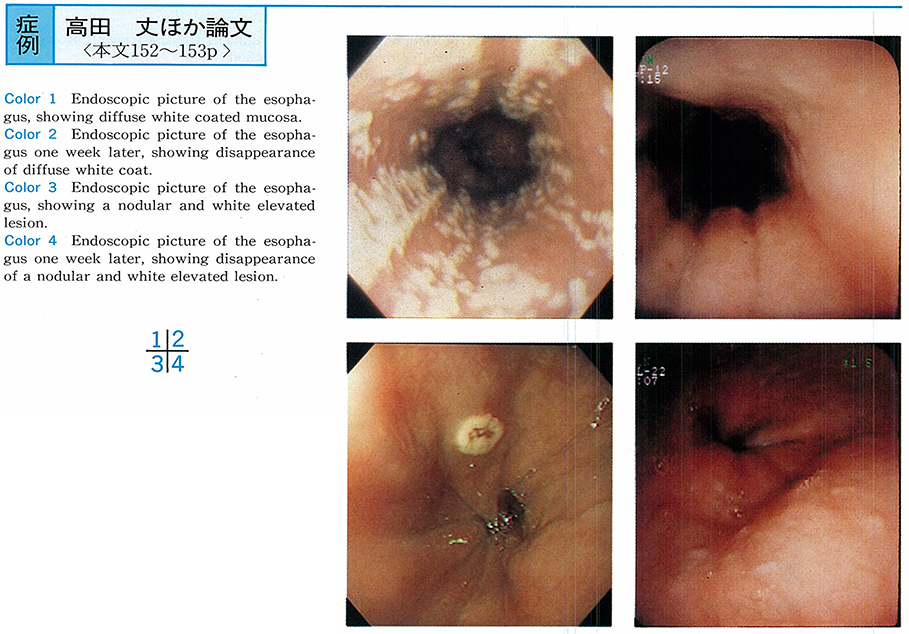
1995 Volume 47 Pages 152-153
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (721K) -
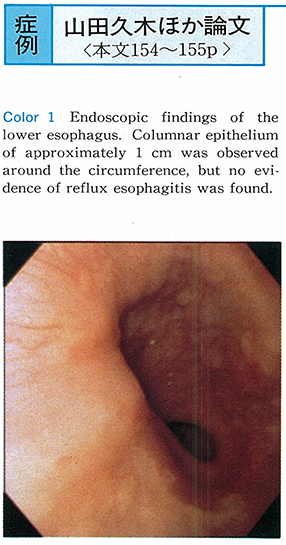
1995 Volume 47 Pages 154-155
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (528K) -
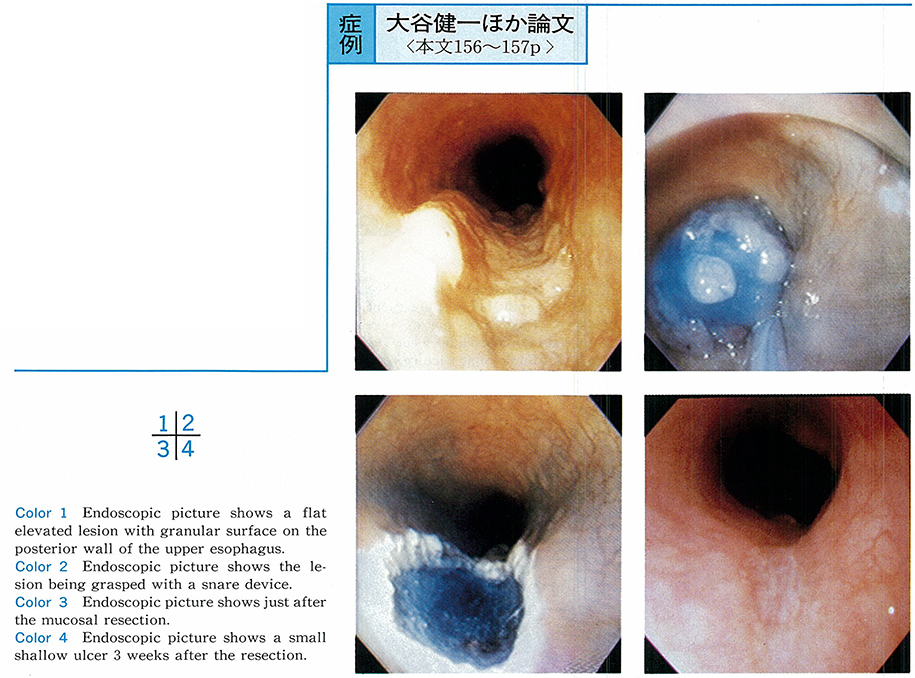
1995 Volume 47 Pages 156-157
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (827K) -
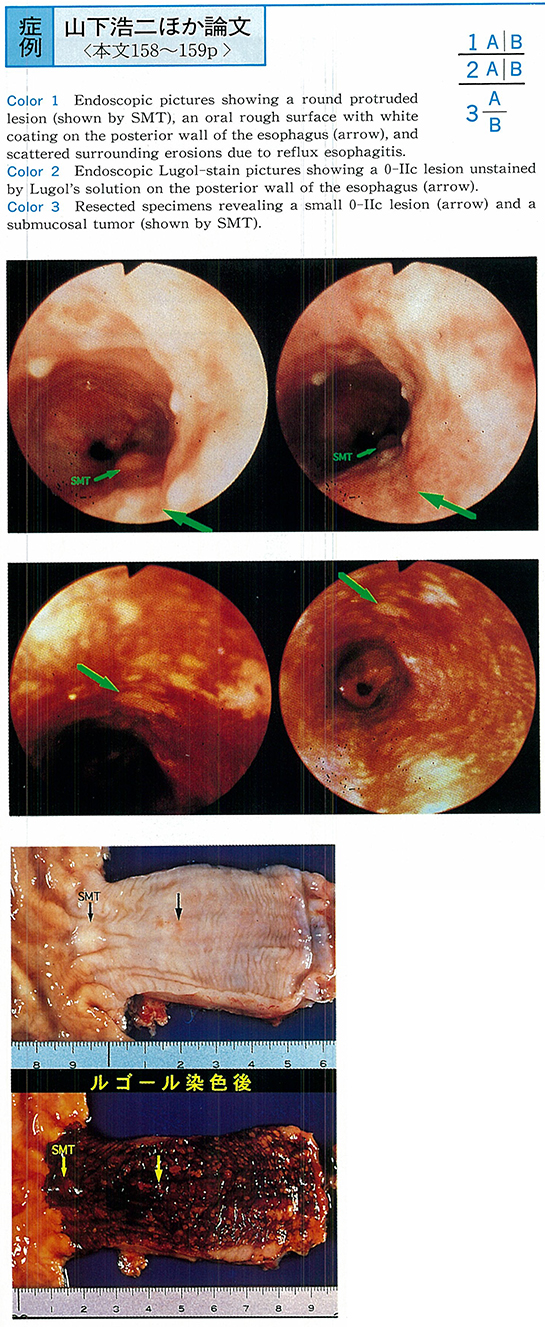
1995 Volume 47 Pages 158-159
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1183K) -
An Endoscopically Resected Case of Early Gastric Carcinoma Located at Esophago-Gastric Juncton (EGJ)1995 Volume 47 Pages 160-161
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1279K) -
1995 Volume 47 Pages 162-163
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (563K) -
1995 Volume 47 Pages 164-165
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1107K) -
1995 Volume 47 Pages 166-167
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (508K) -
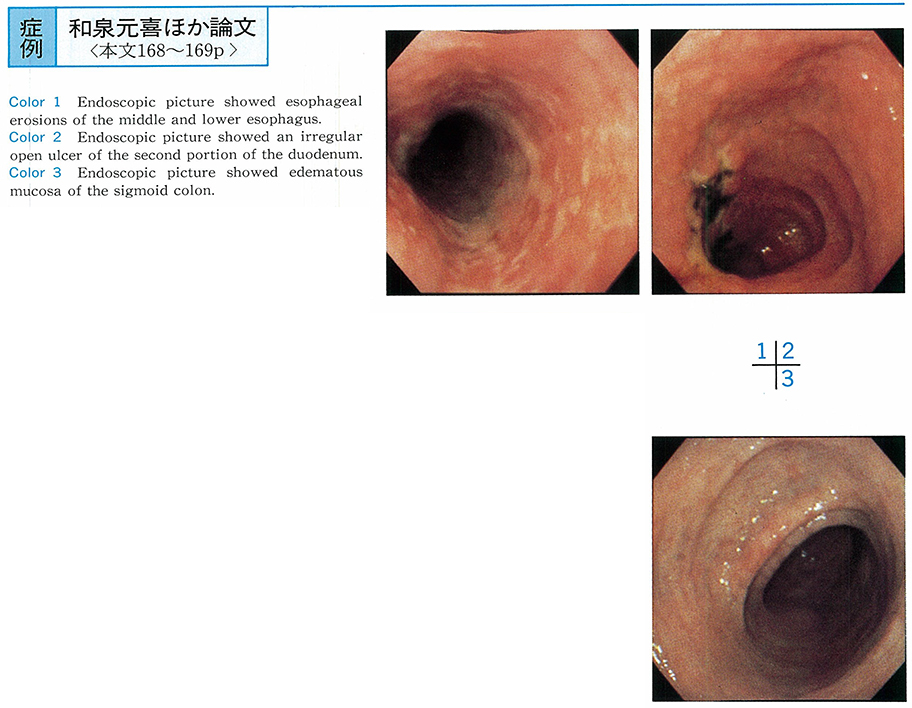
1995 Volume 47 Pages 168-169
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (462K) -
1995 Volume 47 Pages 170-171
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1242K) -
1995 Volume 47 Pages 172-173
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (867K) -
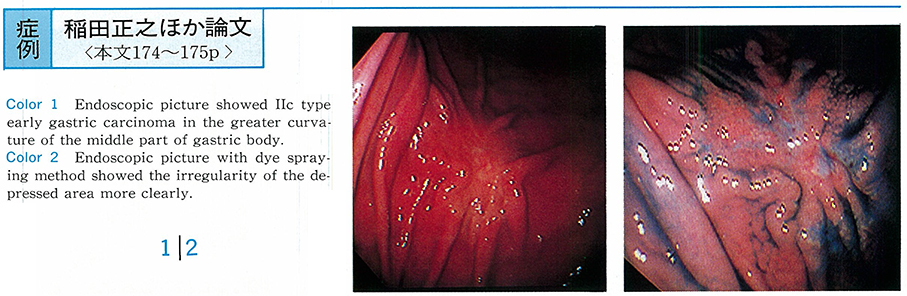
1995 Volume 47 Pages 174-175
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1713K) -
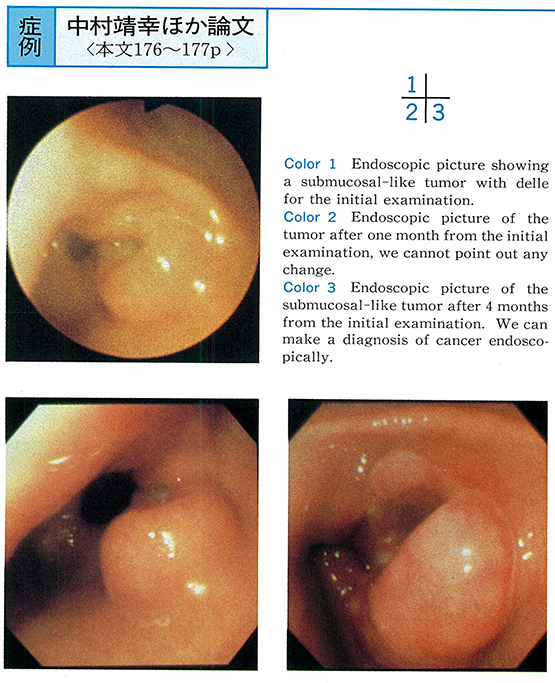
1995 Volume 47 Pages 176-177
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (1066K) -
1995 Volume 47 Pages 178-179
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (702K) -
1995 Volume 47 Pages 180-181
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (992K) -
1995 Volume 47 Pages 182-183
Published: December 08, 1995
Released on J-STAGE: May 01, 2015
Download PDF (194K)