Volume 50
Displaying 1-50 of 76 articles from this issue
-
1997 Volume 50 Pages 1-28
Published: 1997
Released on J-STAGE: February 17, 2015
Download PDF (36696K)
Clinical study
-
1997 Volume 50 Pages 147-151
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (573K) -
1997 Volume 50 Pages 152-156
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (569K) -
1997 Volume 50 Pages 157-159
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (367K) -
1997 Volume 50 Pages 160-163
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (730K) -
1997 Volume 50 Pages 164-167
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (737K) -
1997 Volume 50 Pages 168-172
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (630K) -
1997 Volume 50 Pages 173-176
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (379K)
Case report
-
1997 Volume 50 Pages 177-180
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1251K) -
1997 Volume 50 Pages 181-184
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (936K) -
1997 Volume 50 Pages 185-187
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (424K) -
1997 Volume 50 Pages 188-191
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1051K) -
1997 Volume 50 Pages 192-196
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (998K) -
1997 Volume 50 Pages 196-199
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1103K) -
1997 Volume 50 Pages 200-202
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1072K) -
1997 Volume 50 Pages 203-205
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (790K) -
1997 Volume 50 Pages 206-209
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1468K) -
1997 Volume 50 Pages 210-213
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1610K) -
1997 Volume 50 Pages 214-217
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1578K) -
1997 Volume 50 Pages 218-221
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (961K)
Clinical study
-
1997 Volume 50 Pages 222-223
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (409K) -
1997 Volume 50 Pages 224-225
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (729K) -
1997 Volume 50 Pages 226-227
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (794K) -
1997 Volume 50 Pages 228-229
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (516K) -
1997 Volume 50 Pages 230-231
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (450K) -
1997 Volume 50 Pages 232-233
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (256K) -
1997 Volume 50 Pages 234-235
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (303K) -
1997 Volume 50 Pages 236-237
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (259K) -
1997 Volume 50 Pages 238-239
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (702K)
Clinical study
-
1997 Volume 50 Pages 240-241
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (829K) -
1997 Volume 50 Pages 242-243
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (891K) -
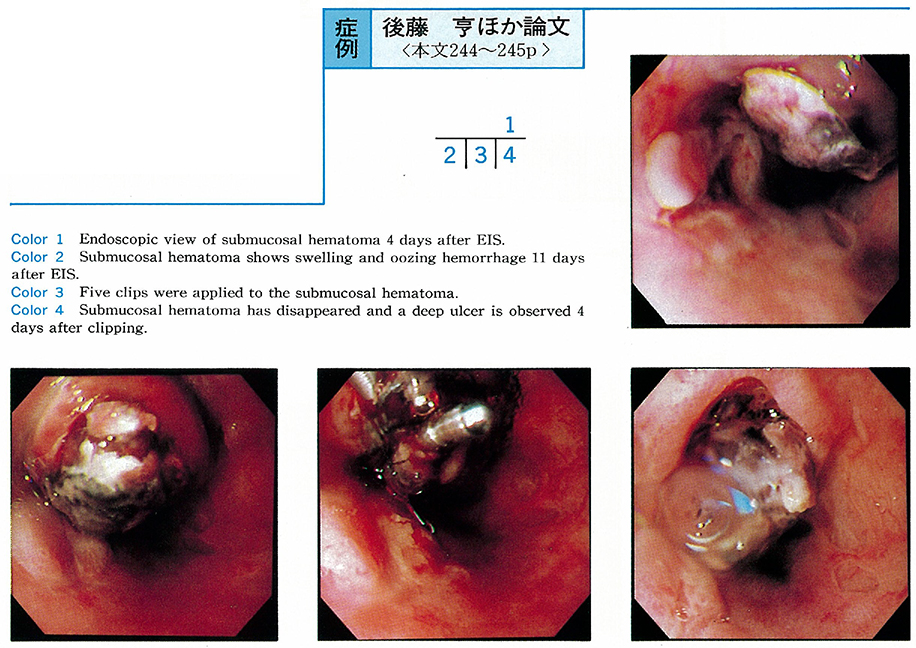
1997 Volume 50 Pages 244-245
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (213K) -
1997 Volume 50 Pages 246-247
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (665K) -
1997 Volume 50 Pages 248-249
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (433K) -
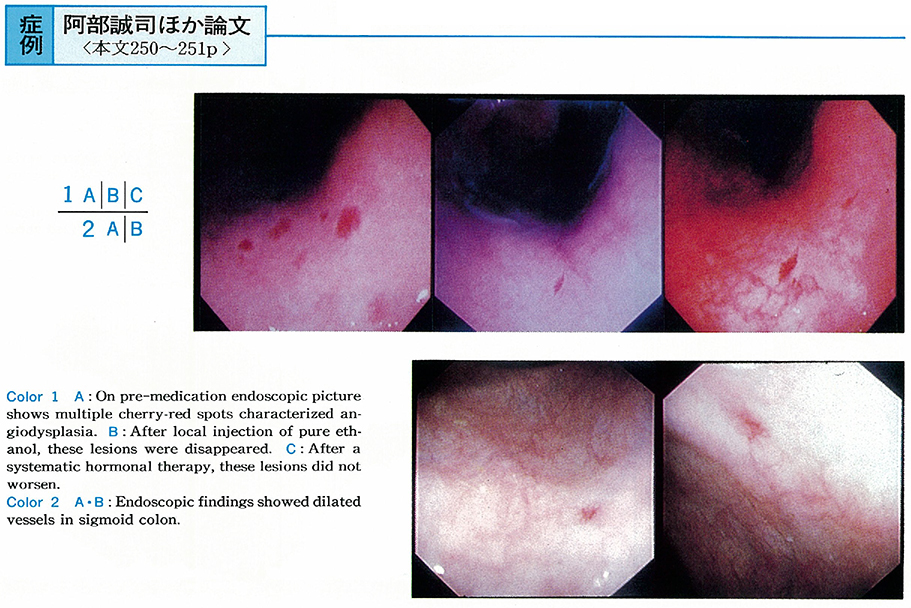
1997 Volume 50 Pages 250-251
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (452K) -
1997 Volume 50 Pages 252-253
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (264K) -
1997 Volume 50 Pages 254-255
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (256K) -
1997 Volume 50 Pages 256-257
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (268K) -
1997 Volume 50 Pages 258-259
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (247K) -
1997 Volume 50 Pages 260-261
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (695K) -
1997 Volume 50 Pages 262-263
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (764K) -
1997 Volume 50 Pages 264-265
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (778K) -
1997 Volume 50 Pages 266-267
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (799K) -
1997 Volume 50 Pages 268-269
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1062K) -
1997 Volume 50 Pages 270-271
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (857K) -
A Case of Gastric Hyperplastic Polyp with Malignant Transformation during Follow-up for Twelve Years1997 Volume 50 Pages 272-273
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (384K) -
1997 Volume 50 Pages 274-275
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1084K) -
1997 Volume 50 Pages 276-277
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (1088K) -
1997 Volume 50 Pages 278-279
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (796K) -
1997 Volume 50 Pages 280-281
Published: June 06, 1997
Released on J-STAGE: February 17, 2015
Download PDF (642K)