Volume 53
Displaying 1-50 of 71 articles from this issue
-
1999 Volume 53 Pages 1-20
Published: 1999
Released on J-STAGE: December 17, 2014
Download PDF (20035K)
Clinical study
-
1999 Volume 53 Pages 53-57
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (701K) -
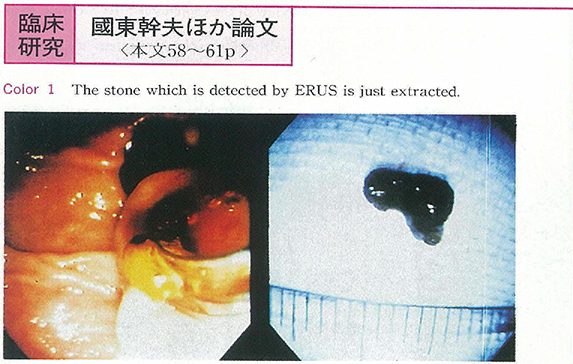
1999 Volume 53 Pages 58-61
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1292K)
Case report
-
1999 Volume 53 Pages 62-65
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (815K) -
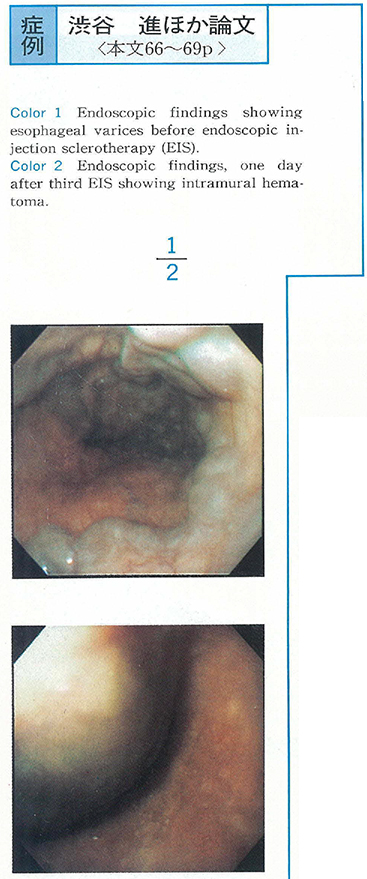
1999 Volume 53 Pages 66-69
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1632K) -
1999 Volume 53 Pages 70-72
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (306K) -
1999 Volume 53 Pages 73-75
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1005K) -
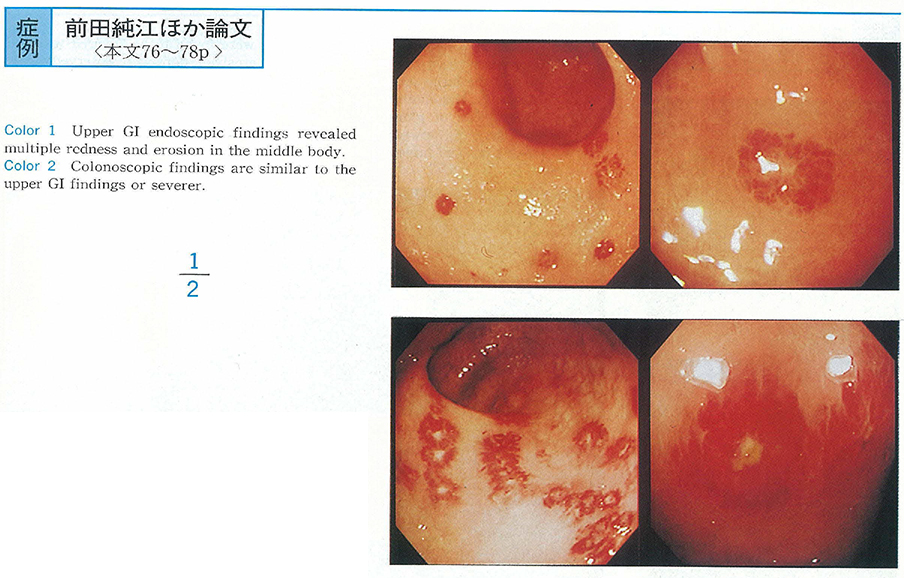
1999 Volume 53 Pages 76-78
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1080K) -
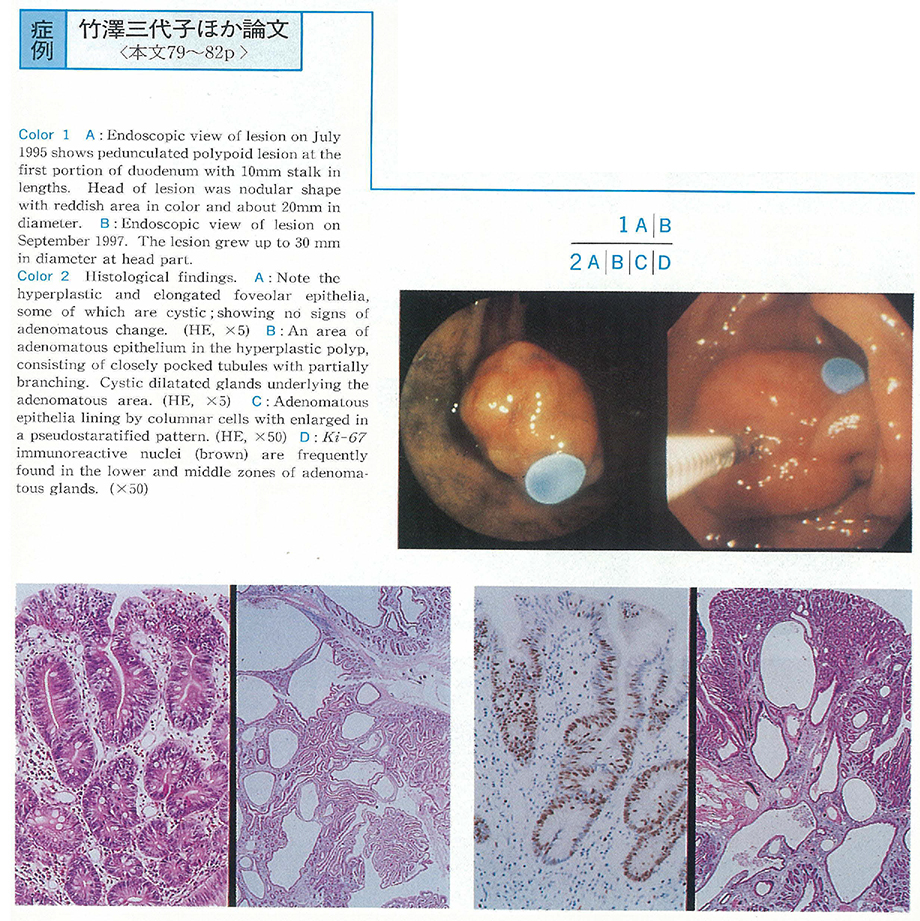
1999 Volume 53 Pages 79-82
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1021K) -
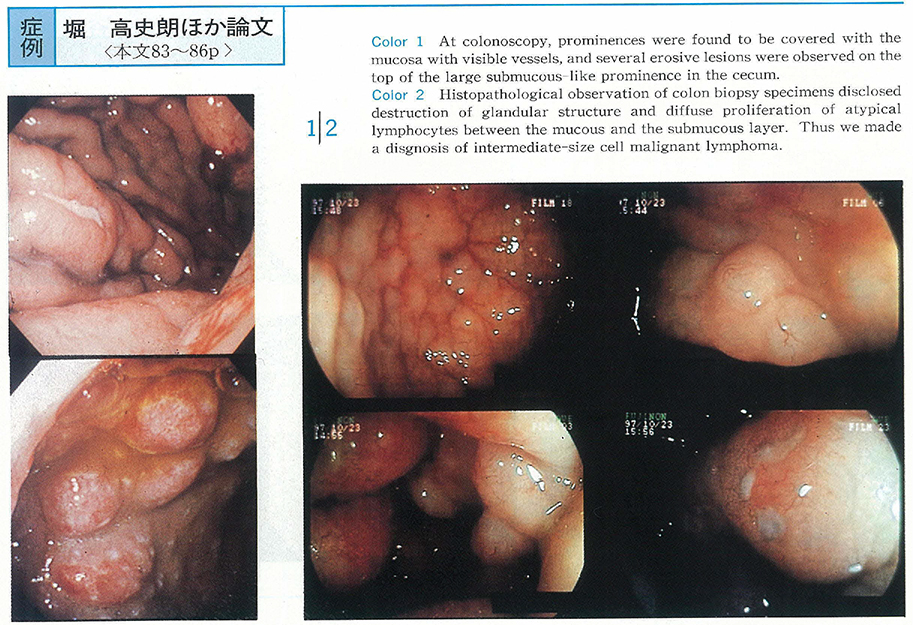
1999 Volume 53 Pages 83-86
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1623K) -
1999 Volume 53 Pages 87-90
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (2065K) -
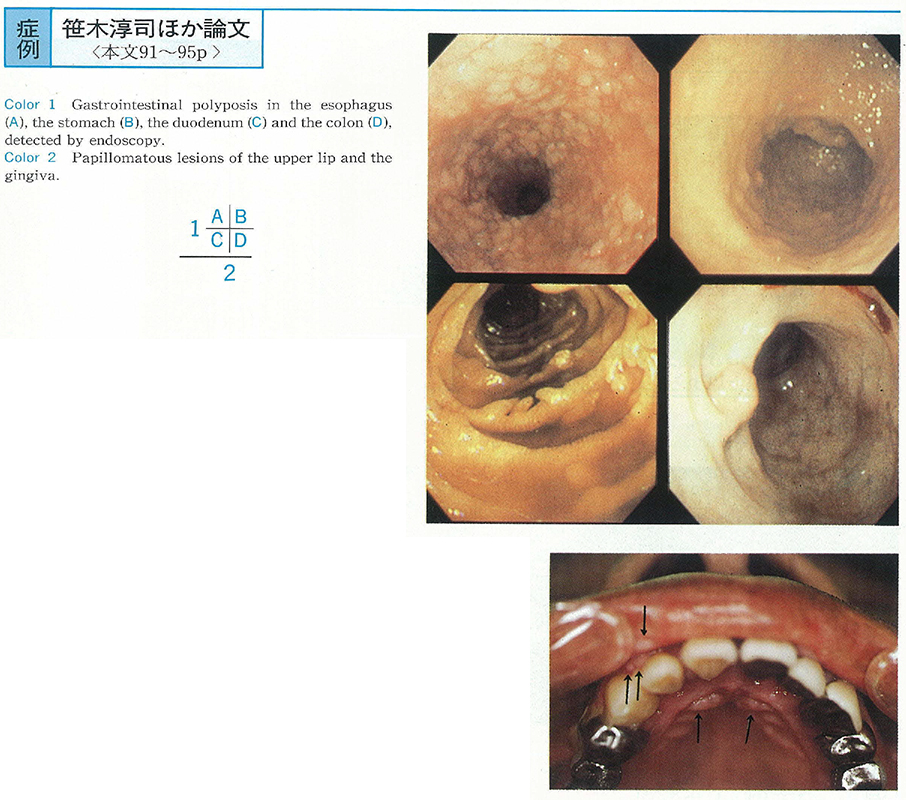
1999 Volume 53 Pages 91-95
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1811K) -
1999 Volume 53 Pages 96-100
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1692K) -
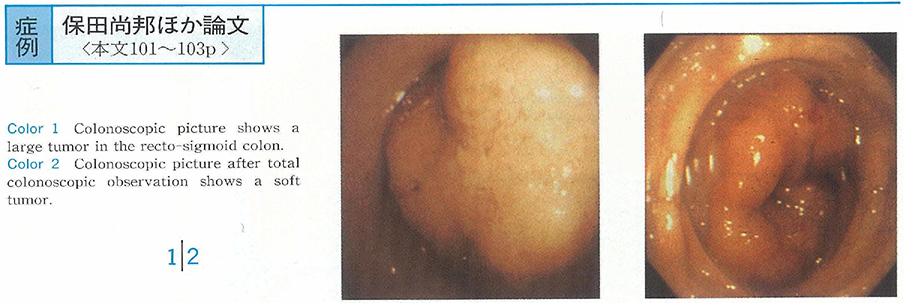
1999 Volume 53 Pages 101-103
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1132K) -
1999 Volume 53 Pages 104-107
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1554K) -
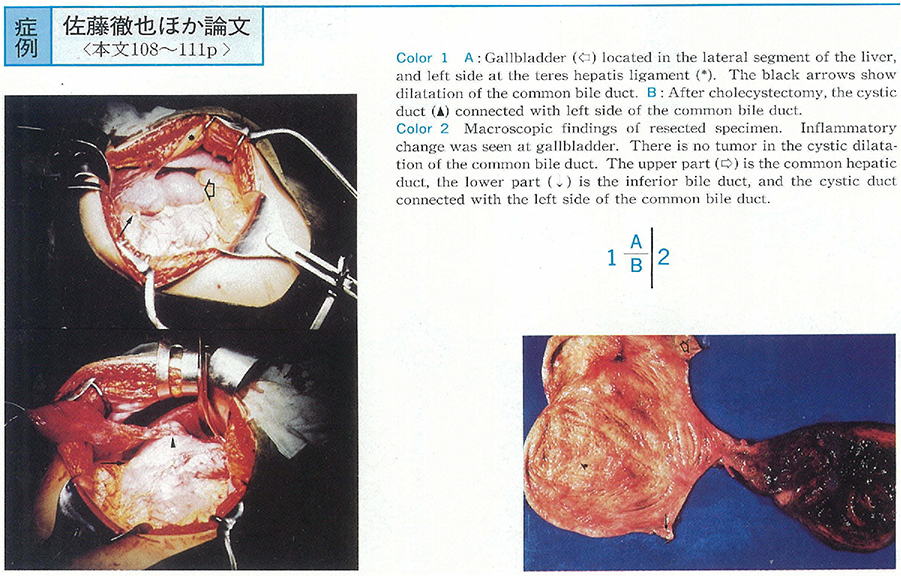
1999 Volume 53 Pages 108-111
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1125K) -
1999 Volume 53 Pages 112-115
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1444K)
Technology and instrument
-
1999 Volume 53 Pages 116-117
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (264K) -
1999 Volume 53 Pages 118-119
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (786K) -
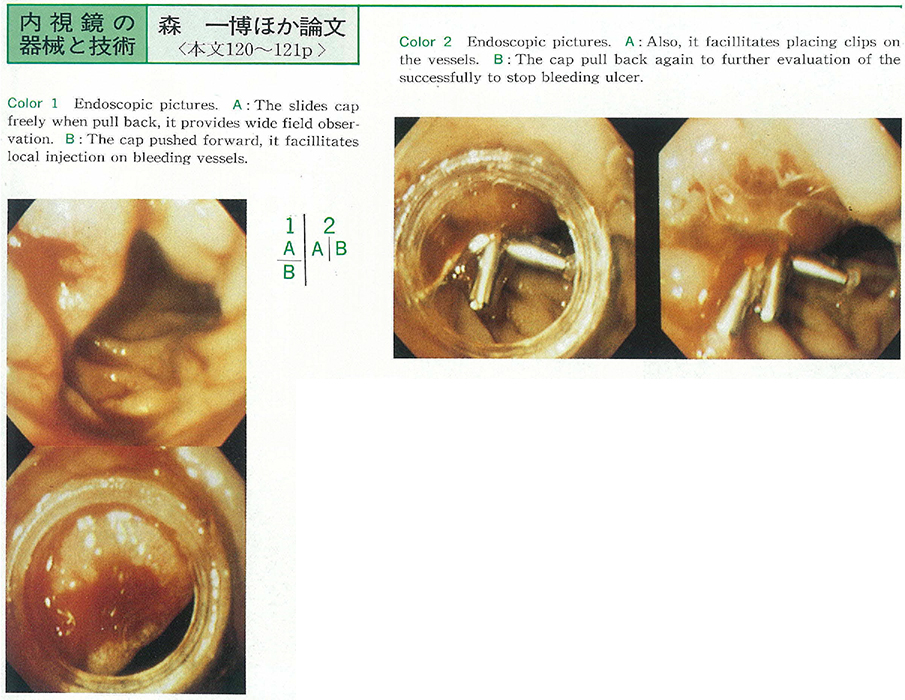
1999 Volume 53 Pages 120-121
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (969K) -
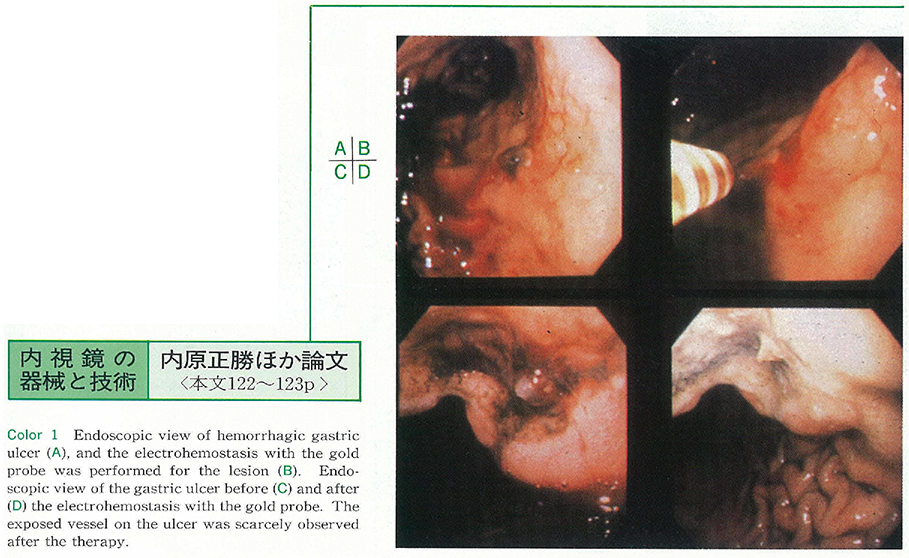
1999 Volume 53 Pages 122-123
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (392K) -
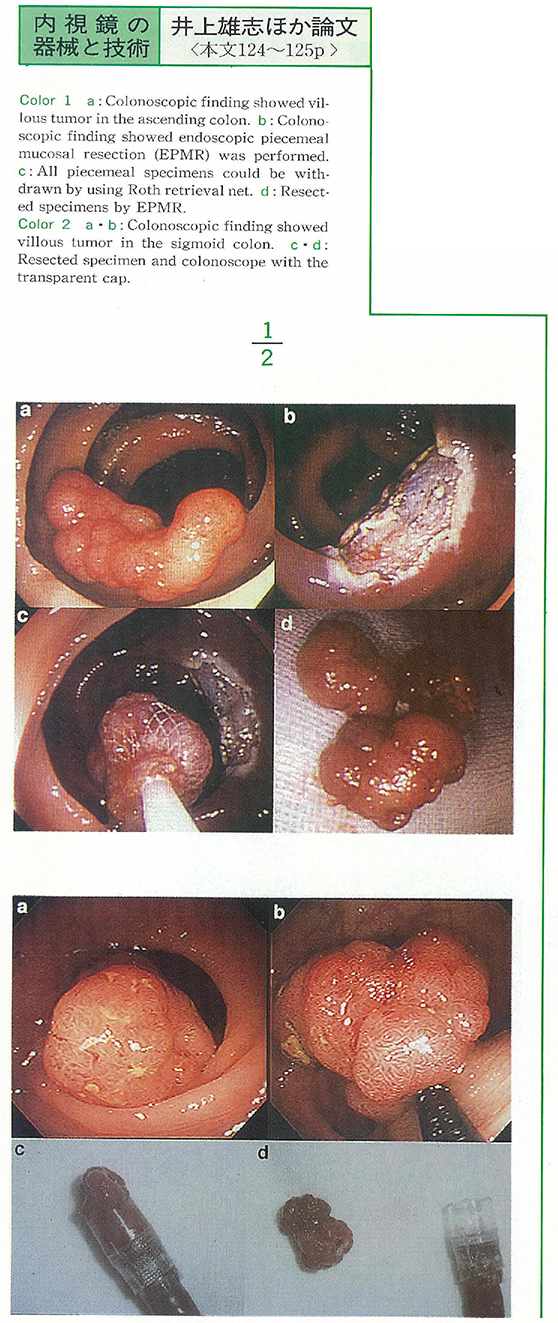
1999 Volume 53 Pages 124-125
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (884K) -
1999 Volume 53 Pages 126-127
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (273K)
Clinical study
-
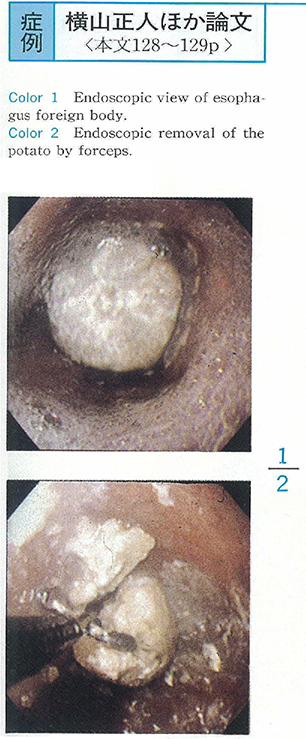
1999 Volume 53 Pages 128-129
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (574K) -
1999 Volume 53 Pages 130-131
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (267K) -
1999 Volume 53 Pages 132-133
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (294K)
Case report
-
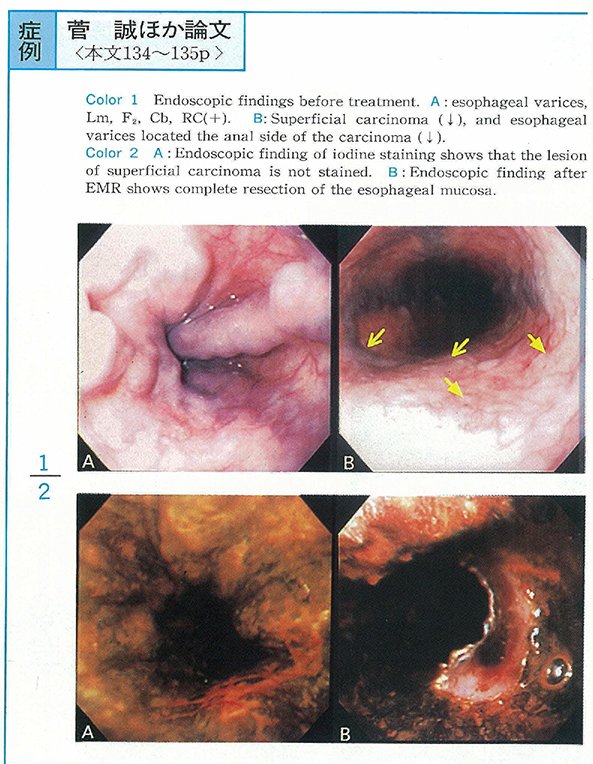
1999 Volume 53 Pages 134-135
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (690K) -
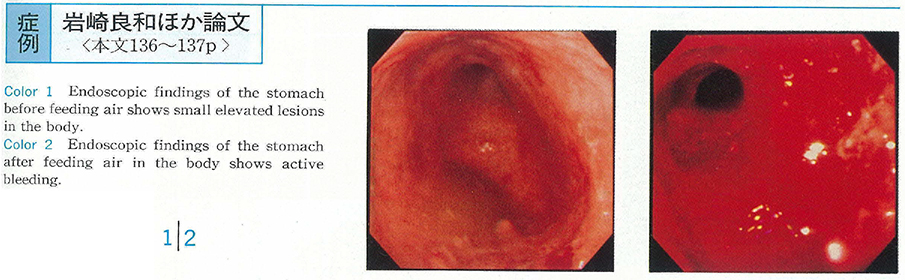
1999 Volume 53 Pages 136-137
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1148K) -
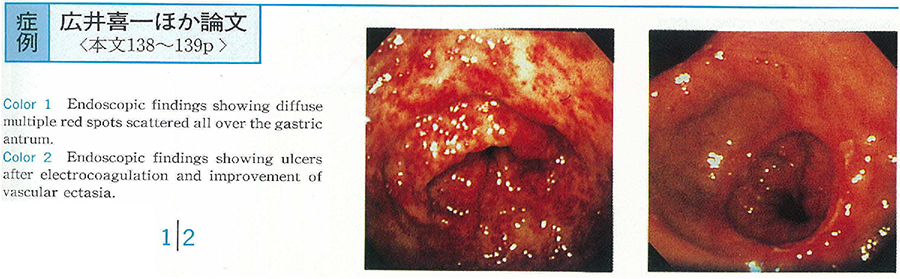
1999 Volume 53 Pages 138-139
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (525K) -
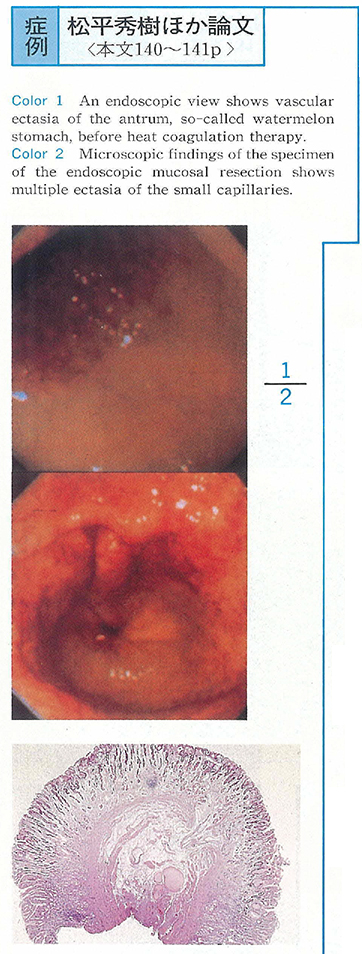
1999 Volume 53 Pages 140-141
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (248K) -
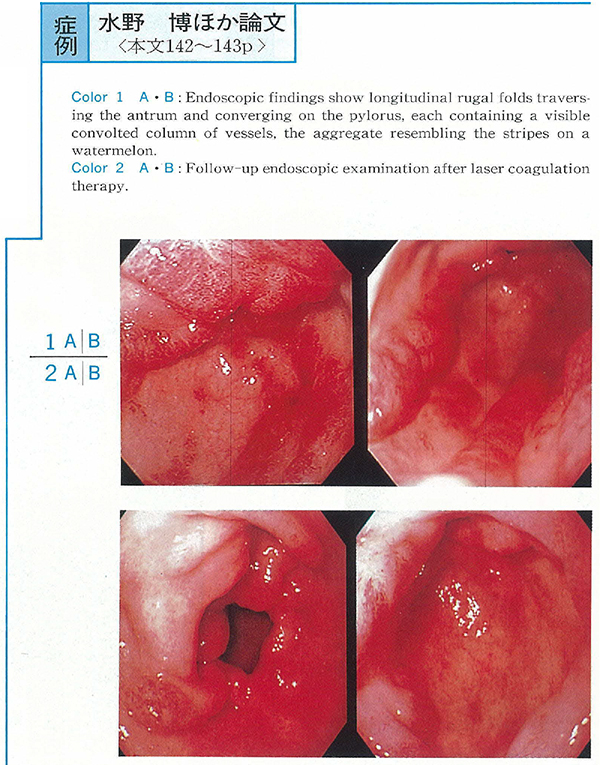
1999 Volume 53 Pages 142-143
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (711K) -
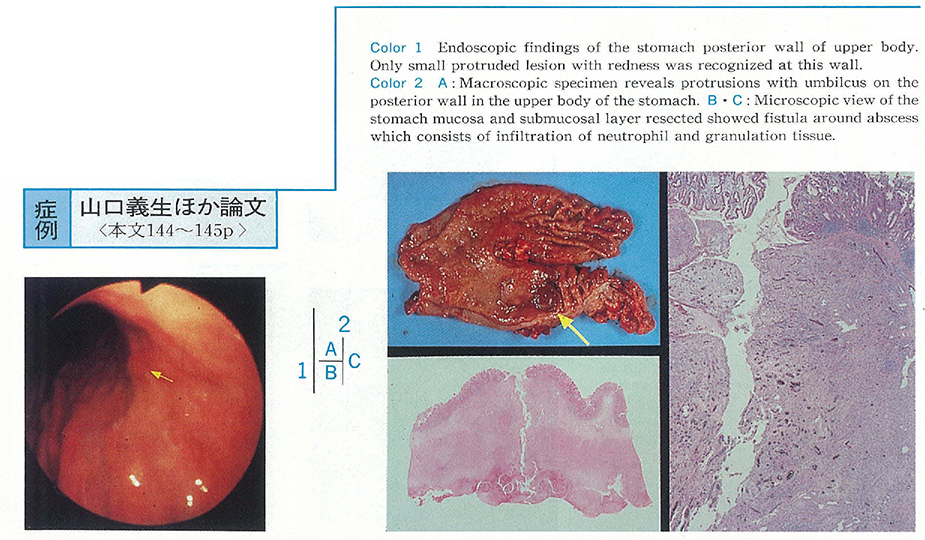
1999 Volume 53 Pages 144-145
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (984K) -
1999 Volume 53 Pages 146-147
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (271K) -
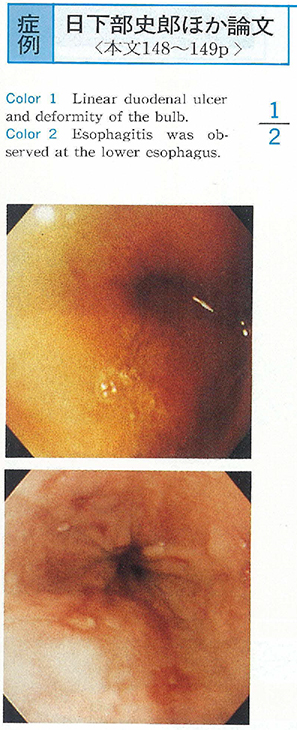
1999 Volume 53 Pages 148-149
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (633K) -
1999 Volume 53 Pages 150-151
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1018K) -
1999 Volume 53 Pages 152-153
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (742K) -
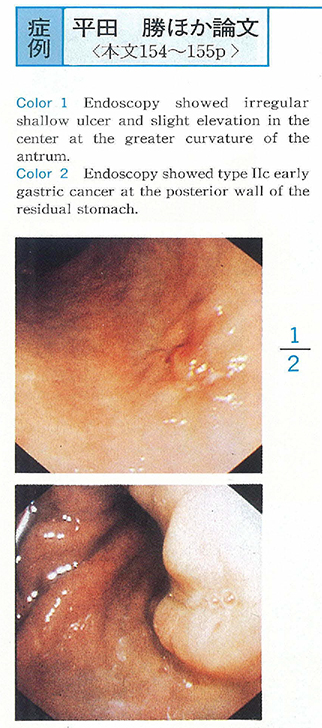
1999 Volume 53 Pages 154-155
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1185K) -
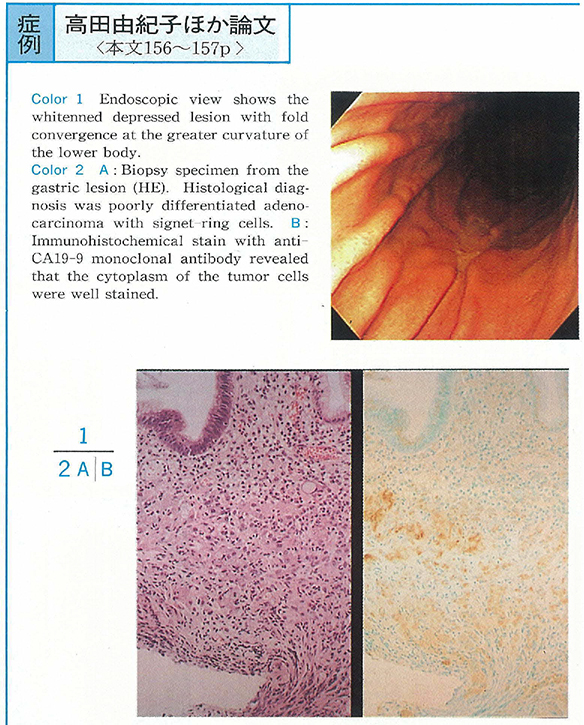
1999 Volume 53 Pages 156-157
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1057K) -
1999 Volume 53 Pages 158-159
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (973K) -
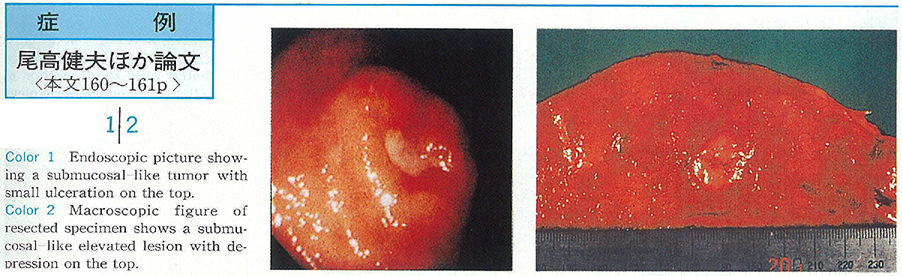
1999 Volume 53 Pages 160-161
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (840K) -
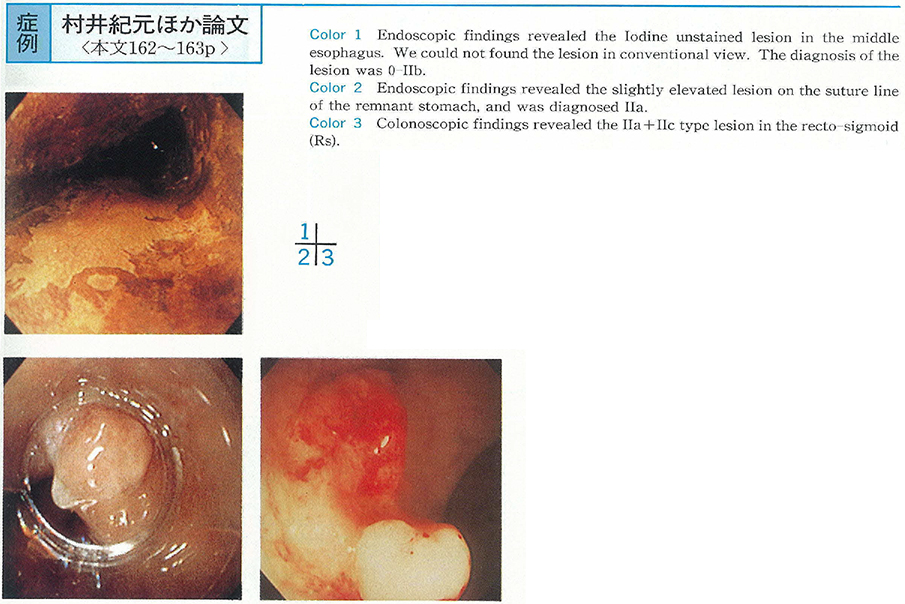
1999 Volume 53 Pages 162-163
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (263K) -
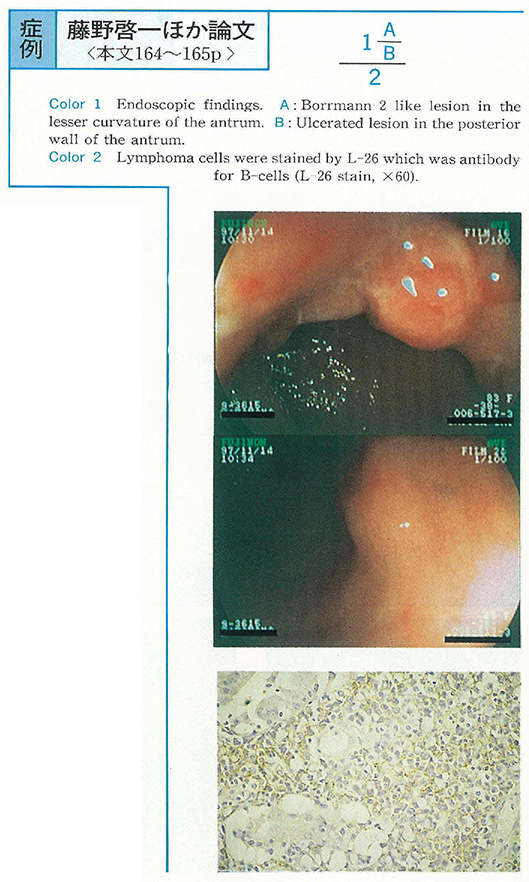
1999 Volume 53 Pages 164-165
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (877K) -
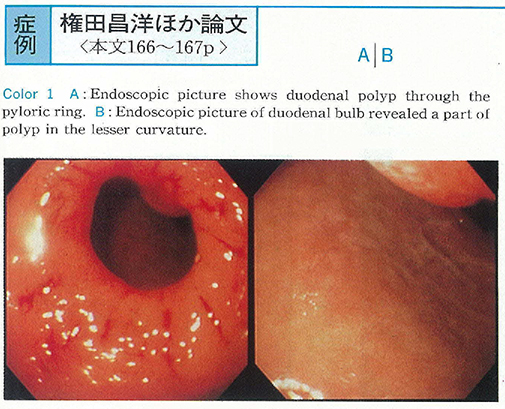
A Case of Complicated Mental Dreamy State after Endoscopic Polypectomy of the Polyp of Duodenal Bulb1999 Volume 53 Pages 166-167
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (401K) -
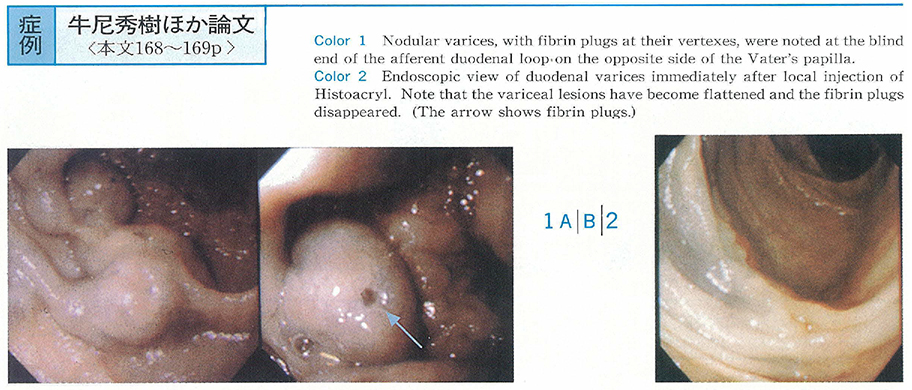
1999 Volume 53 Pages 168-169
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (453K) -
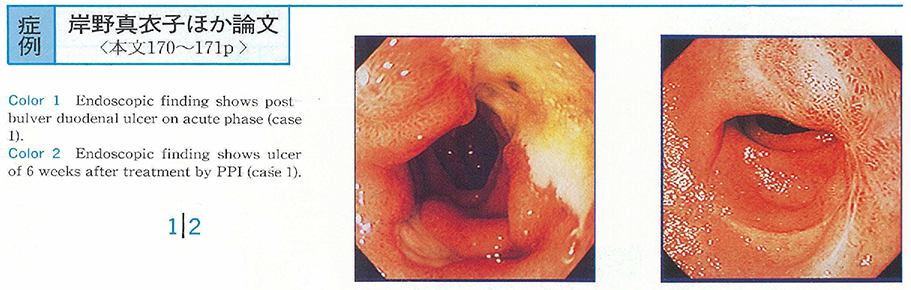
1999 Volume 53 Pages 170-171
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (238K) -
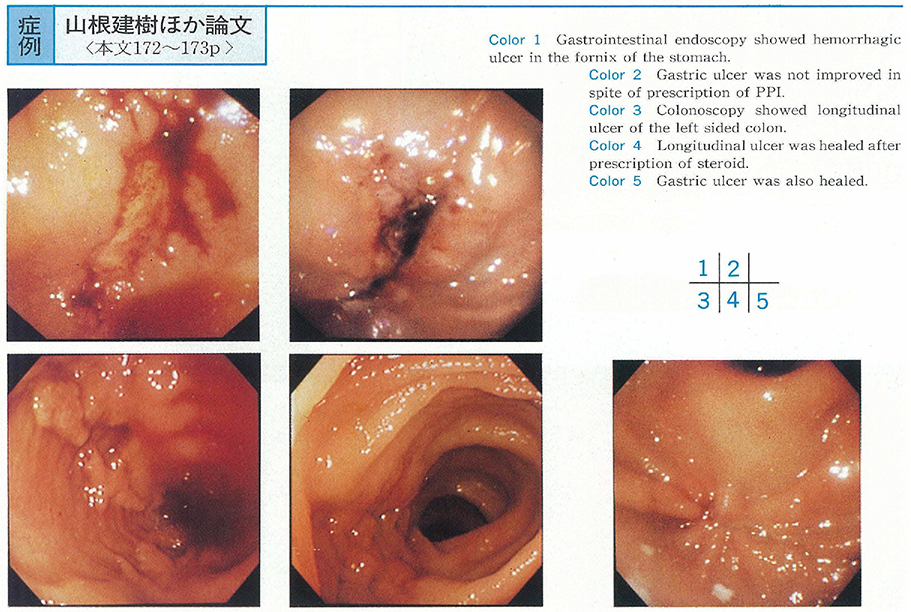
1999 Volume 53 Pages 172-173
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (482K) -
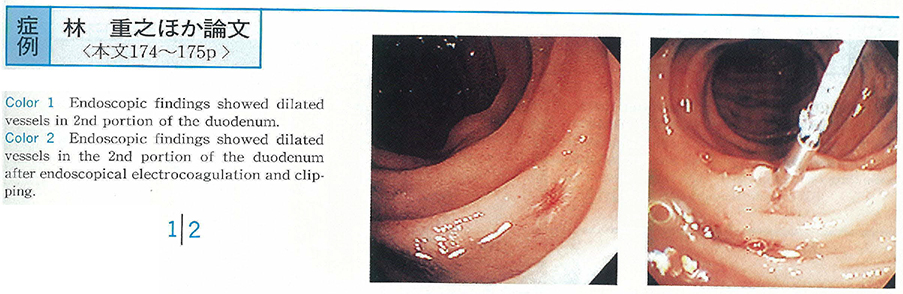
1999 Volume 53 Pages 174-175
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (419K) -
1999 Volume 53 Pages 176-177
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (808K) -
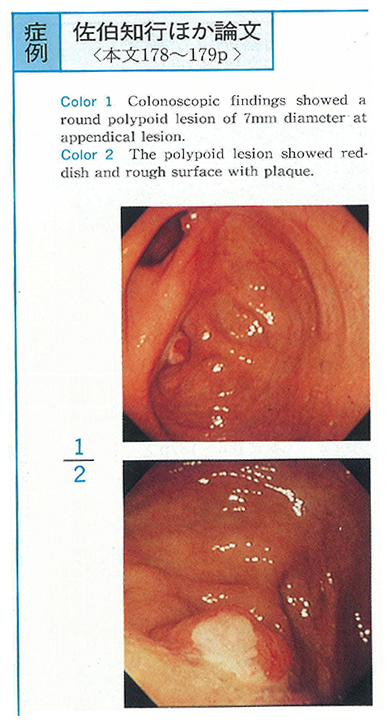
1999 Volume 53 Pages 178-179
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (831K) -
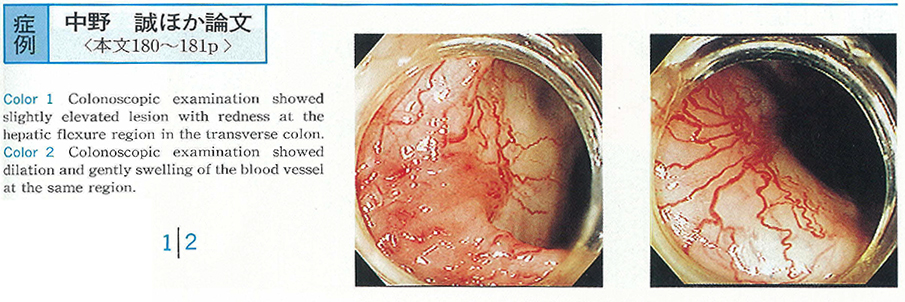
1999 Volume 53 Pages 180-181
Published: January 31, 1999
Released on J-STAGE: December 17, 2014
Download PDF (1024K)