Volume 48
Displaying 1-50 of 81 articles from this issue
-
1996Volume 48 Pages 1-24
Published: 1996
Released on J-STAGE: March 20, 2015
Download PDF (32187K)
Technology and instrument
-
1996Volume 48 Pages 51-54
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1569K)
Clinical study
-
1996Volume 48 Pages 55-58
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1097K) -
1996Volume 48 Pages 59-63
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (615K) -
1996Volume 48 Pages 64-66
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (418K) -
1996Volume 48 Pages 67-70
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (537K) -
1996Volume 48 Pages 71-74
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (547K) -
1996Volume 48 Pages 75-79
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (627K) -
1996Volume 48 Pages 80-84
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1566K) -
1996Volume 48 Pages 85-88
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1244K)
Case report
-
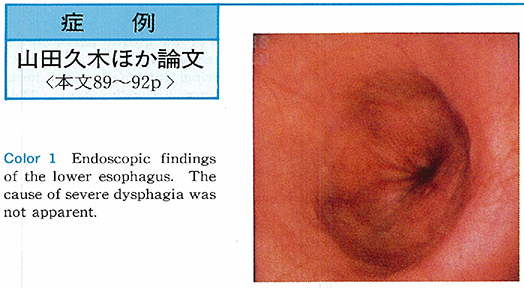
1996Volume 48 Pages 89-92
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1178K) -
1996Volume 48 Pages 93-96
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1455K) -
1996Volume 48 Pages 97-99
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (437K) -
1996Volume 48 Pages 100-103
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1574K) -
1996Volume 48 Pages 104-106
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1232K) -
1996Volume 48 Pages 107-110
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1192K) -
1996Volume 48 Pages 111-114
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1490K) -
1996Volume 48 Pages 115-118
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1336K) -
1996Volume 48 Pages 119-122
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1641K)
Technology and instrument
-
1996Volume 48 Pages 124-125
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1063K) -
1996Volume 48 Pages 126-127
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (795K) -
1996Volume 48 Pages 128-129
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (458K) -
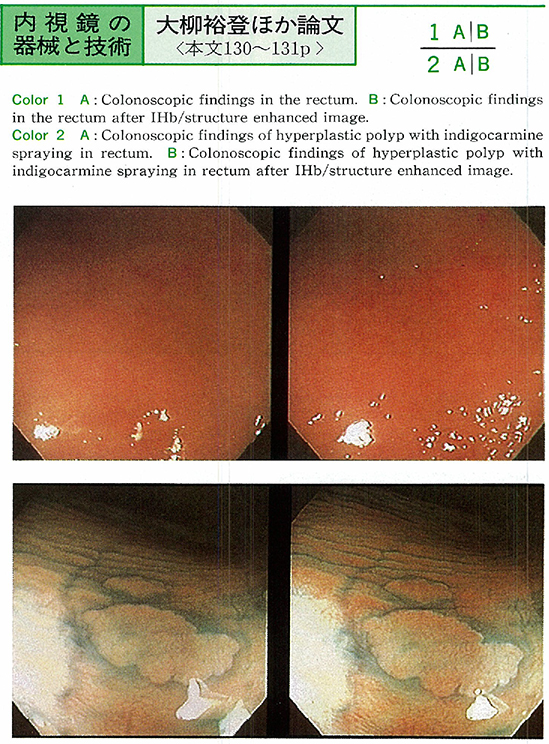
1996Volume 48 Pages 130-131
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (315K) -
1996Volume 48 Pages 132-133
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (565K) -
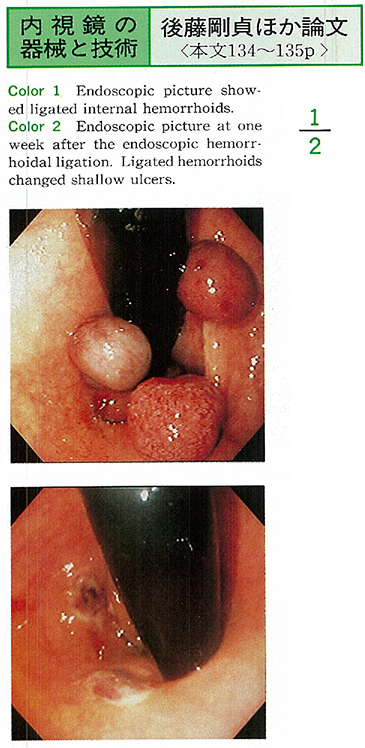
1996Volume 48 Pages 134-135
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (397K)
Clinical study
-
1996Volume 48 Pages 136-137
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (263K) -
1996Volume 48 Pages 138-139
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (329K) -
1996Volume 48 Pages 140-141
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (266K) -
1996Volume 48 Pages 142-143
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (272K) -
1996Volume 48 Pages 144-145
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (271K) -
1996Volume 48 Pages 146-147
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1124K) -
1996Volume 48 Pages 148-149
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (280K) -
1996Volume 48 Pages 150-151
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (298K) -
1996Volume 48 Pages 152-153
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (860K)
Case report
-
1996Volume 48 Pages 154-155
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (676K) -
1996Volume 48 Pages 156-157
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (262K) -
1996Volume 48 Pages 158-159
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (910K) -
1996Volume 48 Pages 160-161
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1062K) -
1996Volume 48 Pages 162-163
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (729K) -
1996Volume 48 Pages 164-165
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (841K) -
1996Volume 48 Pages 166-167
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1347K) -
1996Volume 48 Pages 168-169
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (517K) -
1996Volume 48 Pages 170-171
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (518K) -
1996Volume 48 Pages 172-173
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1334K) -
1996Volume 48 Pages 174-175
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1072K) -
1996Volume 48 Pages 176-177
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1076K) -
1996Volume 48 Pages 178-179
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1065K) -
1996Volume 48 Pages 180-181
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (942K) -
1996Volume 48 Pages 182-183
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (742K) -
1996Volume 48 Pages 184-185
Published: June 07, 1996
Released on J-STAGE: March 20, 2015
Download PDF (1337K)