Current issue
Displaying 1-37 of 37 articles from this issue
- |<
- <
- 1
- >
- >|
-
2000Volume 57Issue 2 Pages 1-8
Published: 2000
Released on J-STAGE: November 04, 2014
Download PDF (6801K)
Technology and instrument
-
2000Volume 57Issue 2 Pages 20-23
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1830K)
Clinical study
-
2000Volume 57Issue 2 Pages 24-28
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (575K) -
2000Volume 57Issue 2 Pages 30-33
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (837K) -
2000Volume 57Issue 2 Pages 34-39
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (587K) -
2000Volume 57Issue 2 Pages 40-44
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (983K) -
2000Volume 57Issue 2 Pages 45-49
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (413K) -
2000Volume 57Issue 2 Pages 50-51
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (398K) -
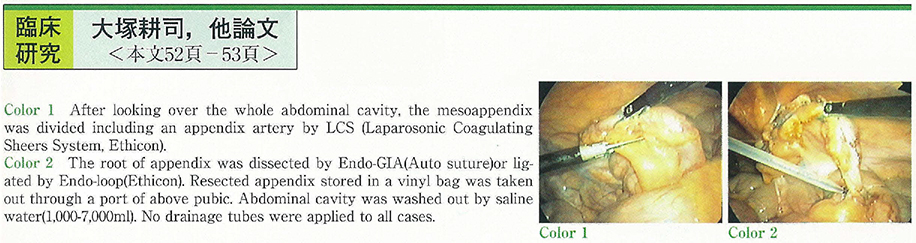
2000Volume 57Issue 2 Pages 52-53
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (258K) -
2000Volume 57Issue 2 Pages 54-55
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1740K) -
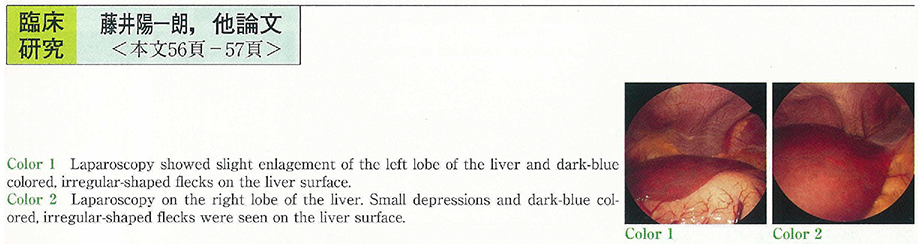
2000Volume 57Issue 2 Pages 56-57
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (523K)
Case report
-
2000Volume 57Issue 2 Pages 58-60
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1354K) -
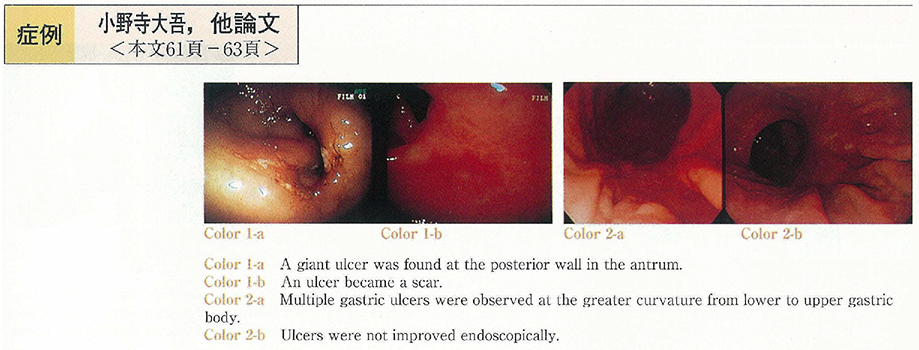
2000Volume 57Issue 2 Pages 61-63
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1098K) -
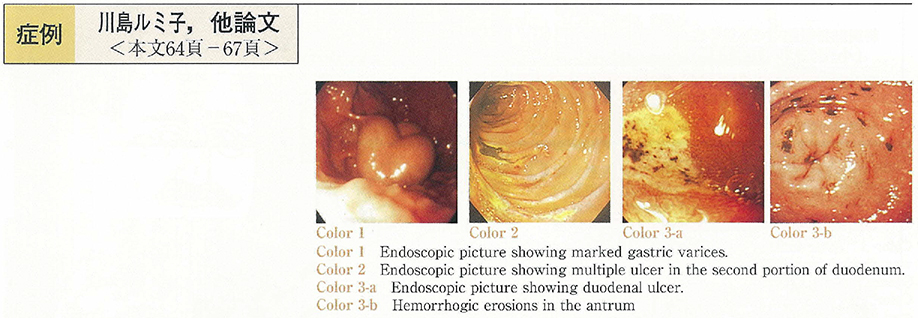
2000Volume 57Issue 2 Pages 64-67
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1233K) -
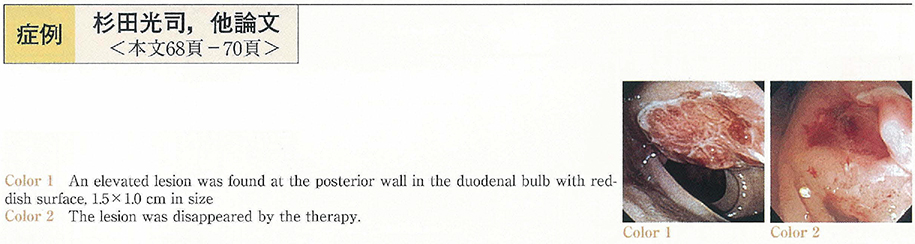
2000Volume 57Issue 2 Pages 68-70
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (944K) -
A Case of Juvenile Colitic Cancer, Developing Over a Short Term From The Onset of Ulcerative Colitis2000Volume 57Issue 2 Pages 71-74
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1989K) -
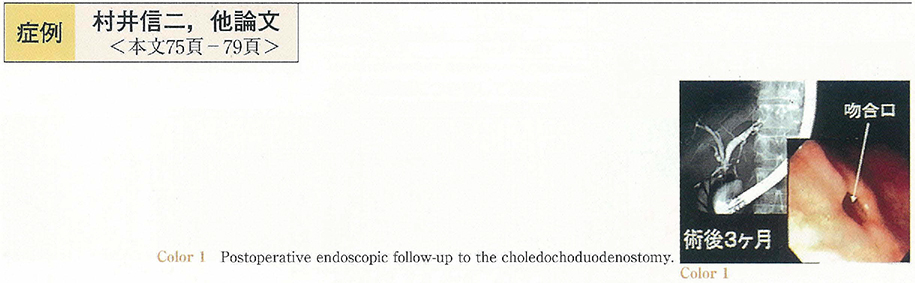
2000Volume 57Issue 2 Pages 75-79
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (2400K) -
2000Volume 57Issue 2 Pages 80-83
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1790K) -
2000Volume 57Issue 2 Pages 84-87
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1610K) -
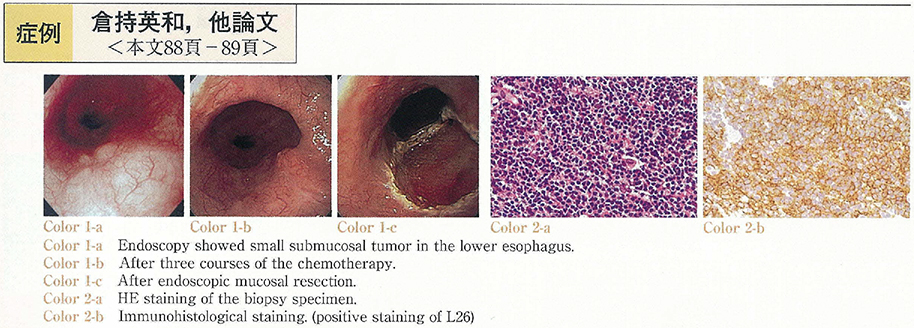
2000Volume 57Issue 2 Pages 88-89
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (877K) -
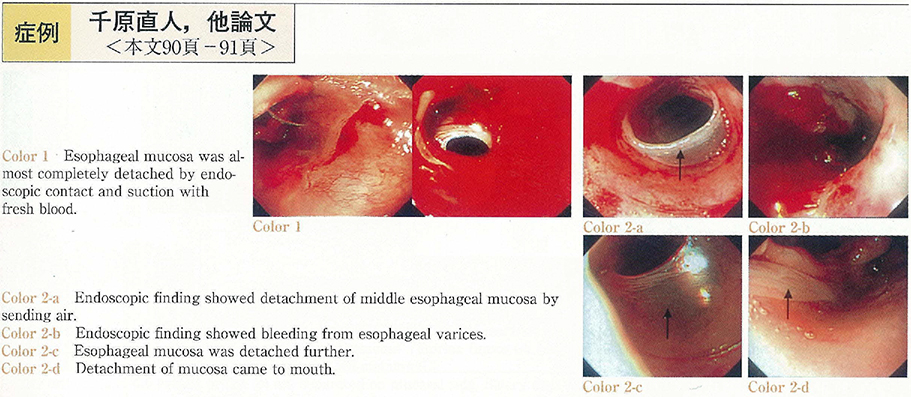
2000Volume 57Issue 2 Pages 90-91
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (851K) -
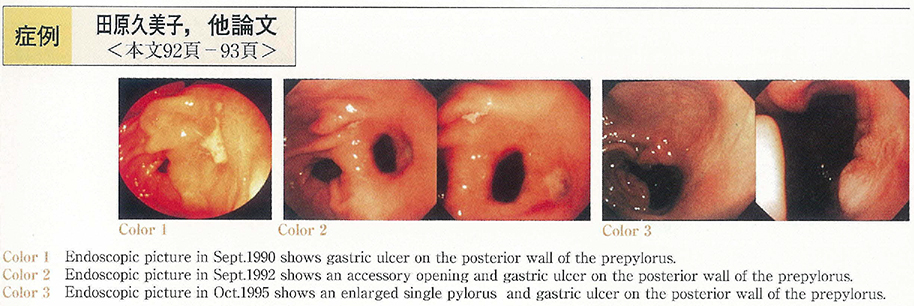
2000Volume 57Issue 2 Pages 92-93
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (242K) -
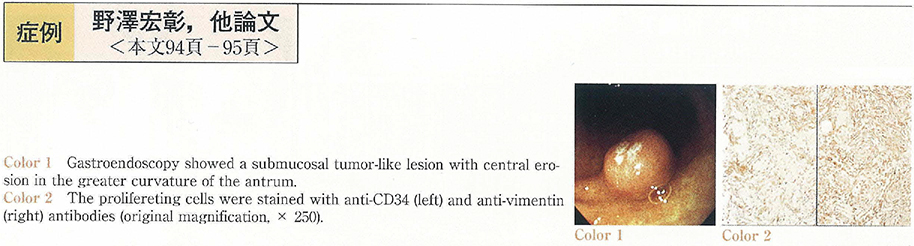
2000Volume 57Issue 2 Pages 94-95
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1146K) -
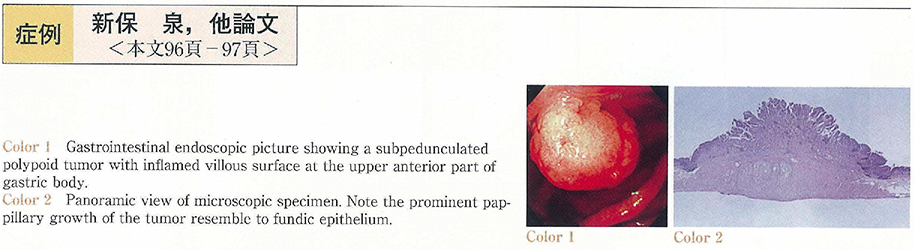
2000Volume 57Issue 2 Pages 96-97
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1108K) -
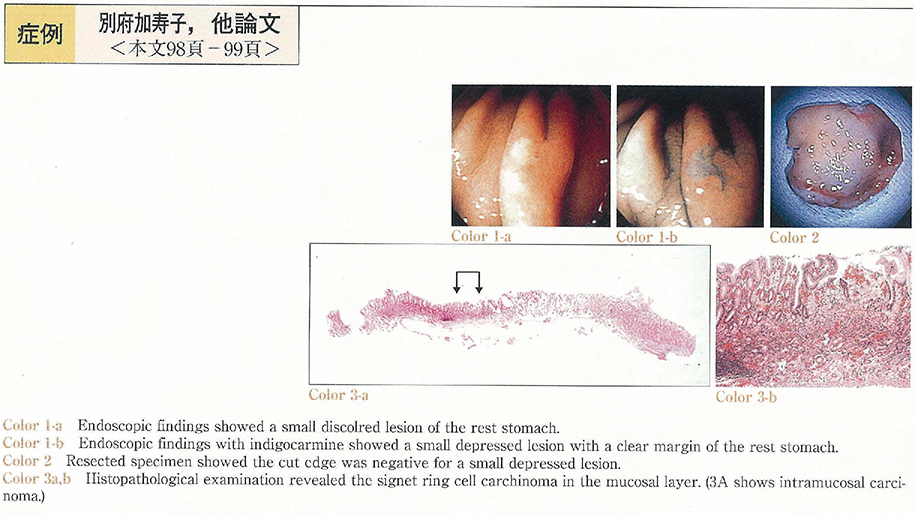
2000Volume 57Issue 2 Pages 98-99
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (501K) -
2000Volume 57Issue 2 Pages 100-101
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (766K) -
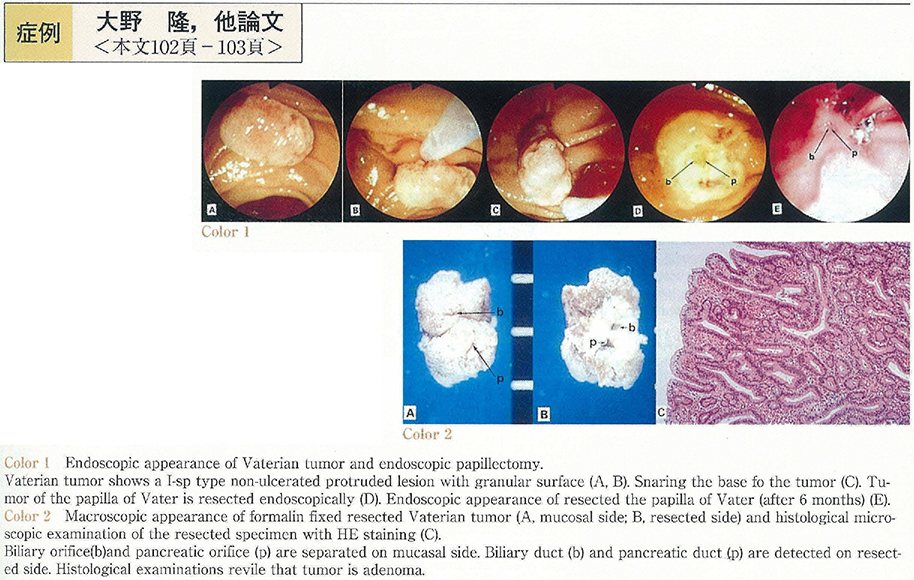
2000Volume 57Issue 2 Pages 102-103
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (528K) -
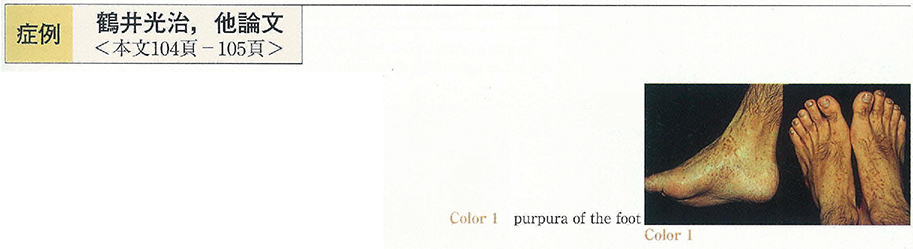
2000Volume 57Issue 2 Pages 104-105
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (571K) -
2000Volume 57Issue 2 Pages 106-107
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (1239K) -
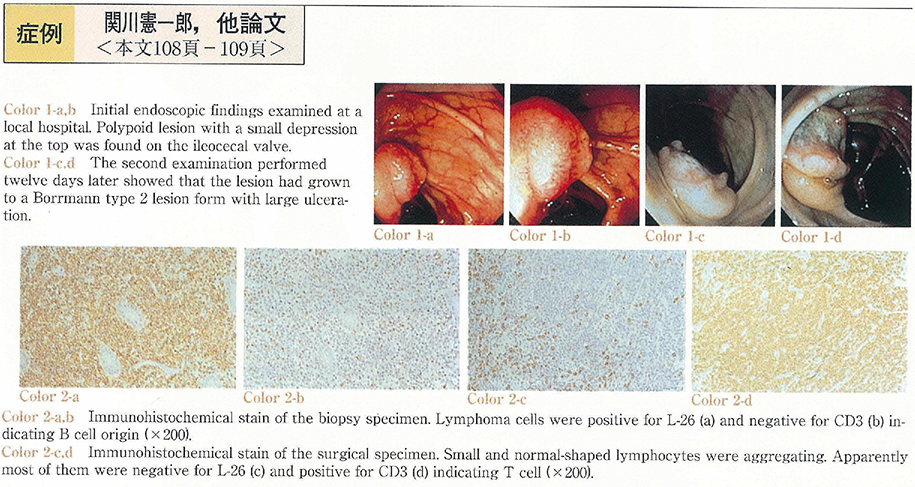
2000Volume 57Issue 2 Pages 108-109
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (901K) -
2000Volume 57Issue 2 Pages 110-111
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (978K) -
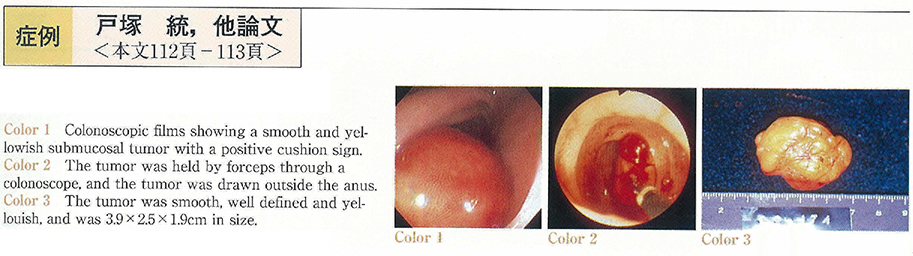
2000Volume 57Issue 2 Pages 112-113
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (898K) -
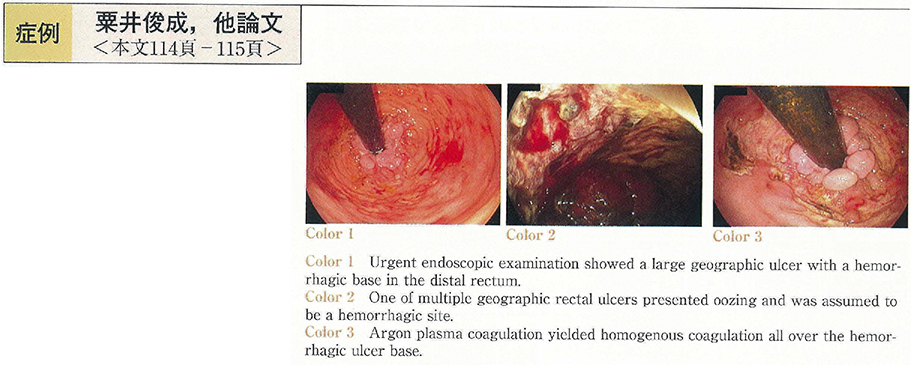
2000Volume 57Issue 2 Pages 114-115
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (238K) -
2000Volume 57Issue 2 Pages 116-117
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (570K) -
2000Volume 57Issue 2 Pages 118-119
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (615K) -
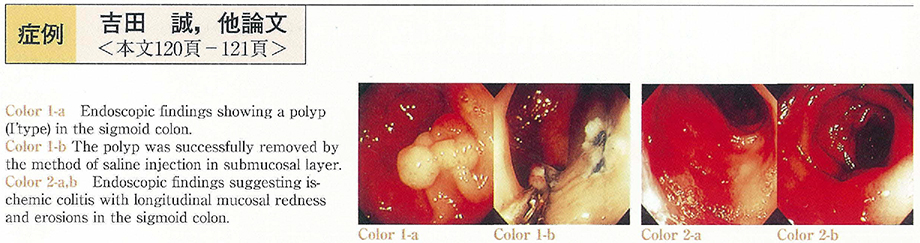
2000Volume 57Issue 2 Pages 120-121
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (358K) -
2000Volume 57Issue 2 Pages 122-123
Published: November 15, 2000
Released on J-STAGE: November 04, 2014
Download PDF (235K)
- |<
- <
- 1
- >
- >|