Volume 55, Issue 2
Displaying 1-32 of 32 articles from this issue
- |<
- <
- 1
- >
- >|
-
1999Volume 55Issue 2 Pages 1-8
Published: 1999
Released on J-STAGE: October 28, 2014
Download PDF (9128K)
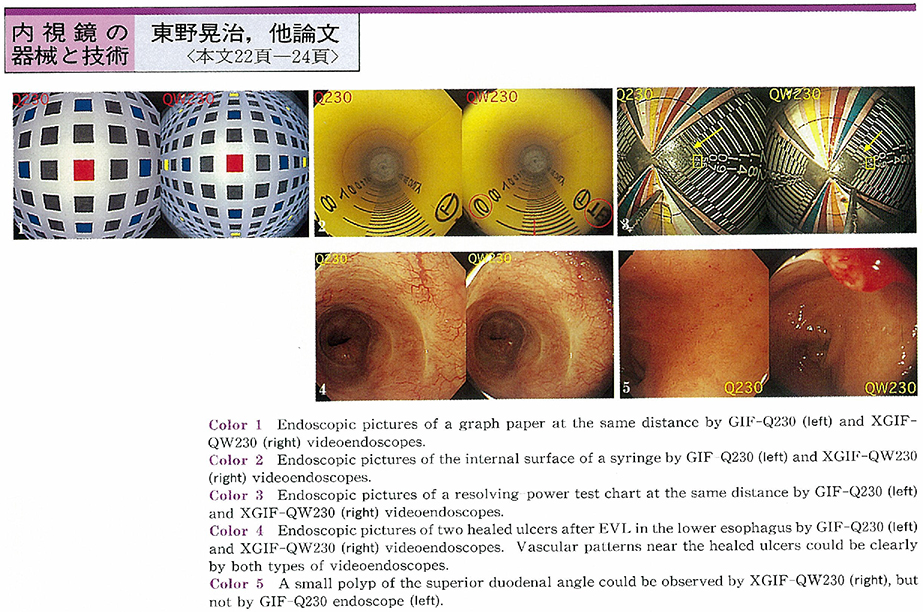
Technology and instrument
-
1999Volume 55Issue 2 Pages 22-24
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (275K)
Clinical study
-
1999Volume 55Issue 2 Pages 25-29
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1296K) -
1999Volume 55Issue 2 Pages 30-33
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1419K) -
1999Volume 55Issue 2 Pages 34-37
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1107K)
Case report
-
1999Volume 55Issue 2 Pages 38-40
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (821K) -
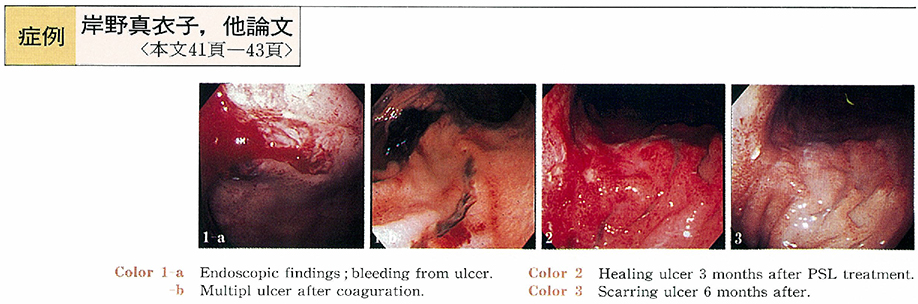
1999Volume 55Issue 2 Pages 41-43
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (536K) -
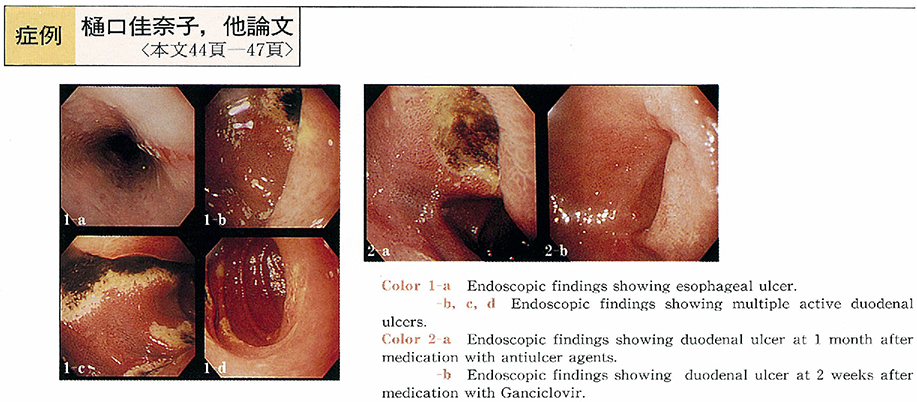
1999Volume 55Issue 2 Pages 44-47
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (416K) -
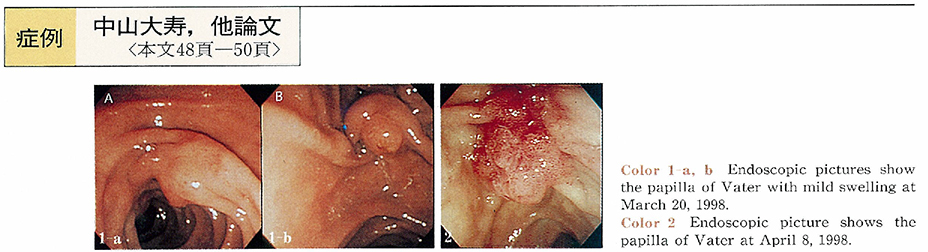
1999Volume 55Issue 2 Pages 48-50
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1046K) -
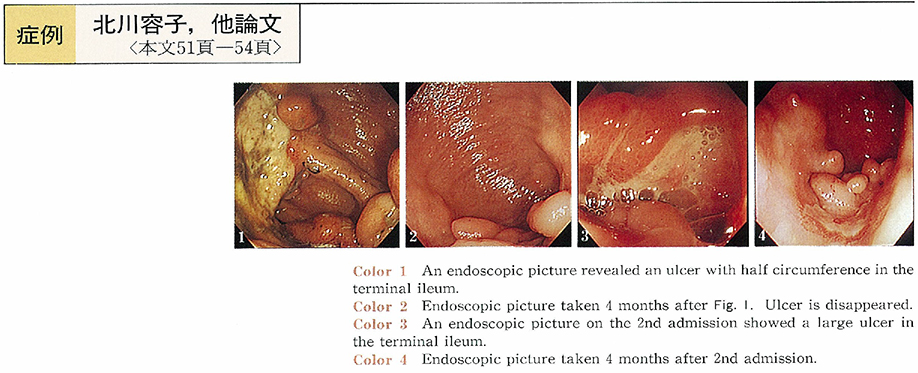
1999Volume 55Issue 2 Pages 51-54
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (534K) -
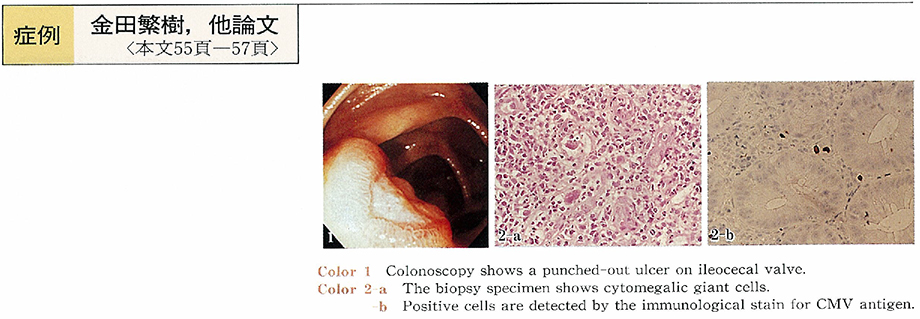
1999Volume 55Issue 2 Pages 55-57
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (356K)
Technology and instrument
-
1999Volume 55Issue 2 Pages 58-59
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (350K) -
1999Volume 55Issue 2 Pages 60-62
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1382K)
Clinical study
-
1999Volume 55Issue 2 Pages 64-66
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (338K) -
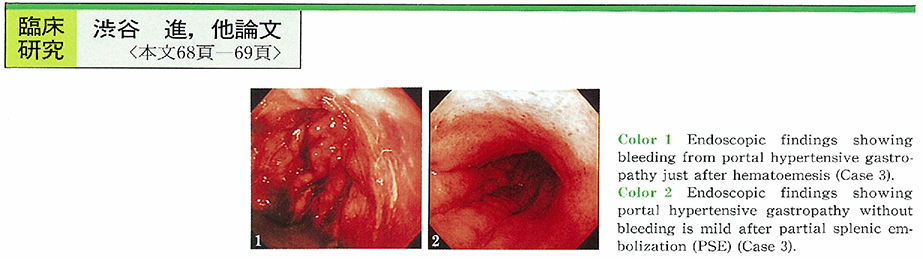
1999Volume 55Issue 2 Pages 68-69
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (432K) -
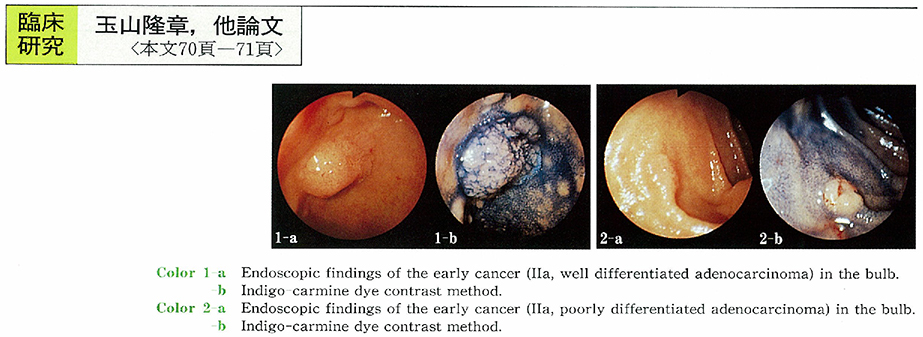
1999Volume 55Issue 2 Pages 70-71
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (229K)
Case report
-
1999Volume 55Issue 2 Pages 72-73
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (258K) -
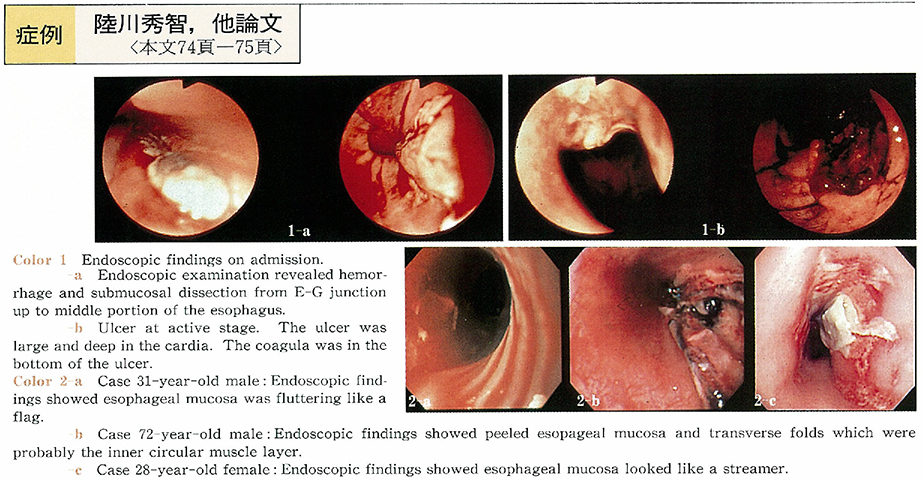
1999Volume 55Issue 2 Pages 74-75
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (445K) -
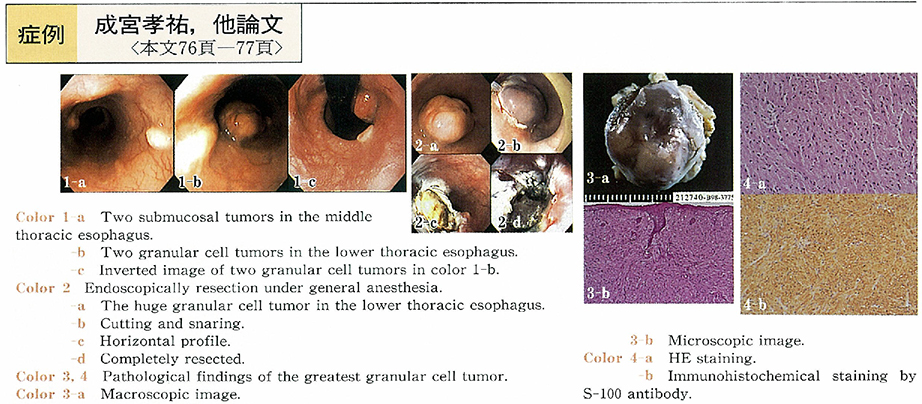
1999Volume 55Issue 2 Pages 76-77
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (514K) -
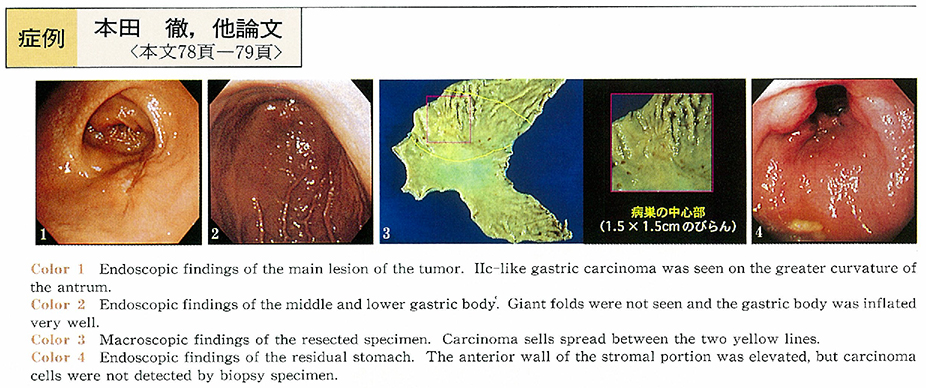
1999Volume 55Issue 2 Pages 78-79
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (1233K) -
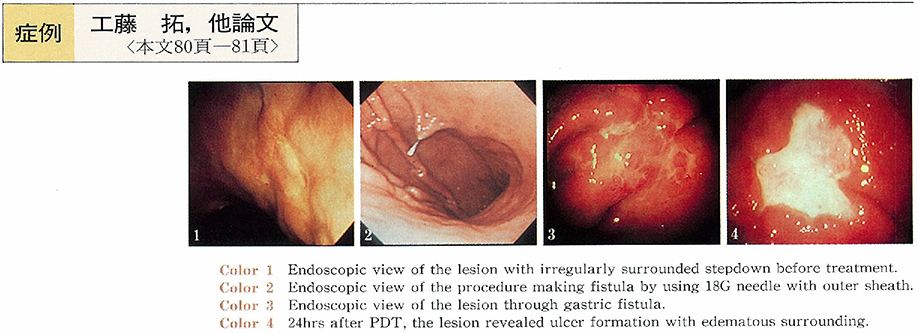
1999Volume 55Issue 2 Pages 80-81
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (566K) -
1999Volume 55Issue 2 Pages 82-83
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (764K) -
1999Volume 55Issue 2 Pages 84-85
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (567K) -
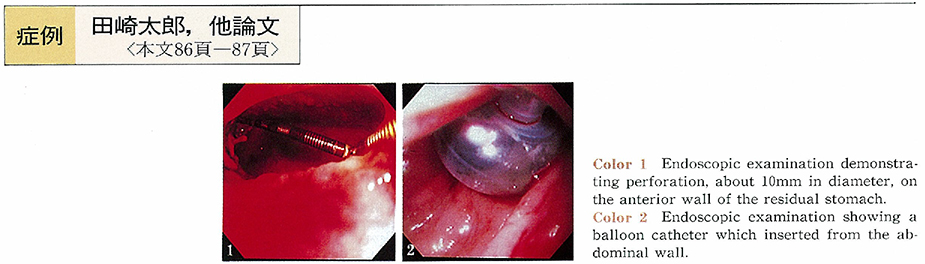
1999Volume 55Issue 2 Pages 86-87
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (702K) -
1999Volume 55Issue 2 Pages 88-89
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (485K) -
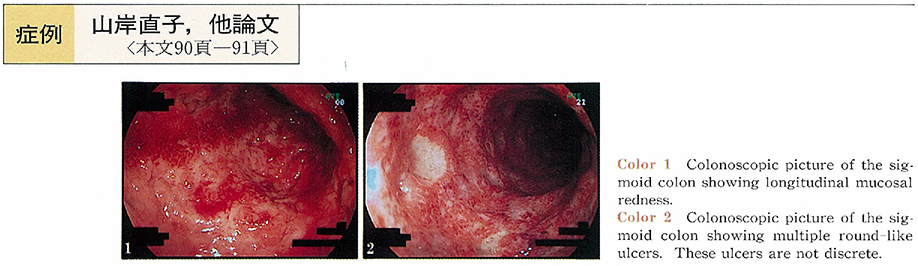
1999Volume 55Issue 2 Pages 90-91
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (376K) -
1999Volume 55Issue 2 Pages 92-93
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (566K) -
1999Volume 55Issue 2 Pages 94-95
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (535K) -
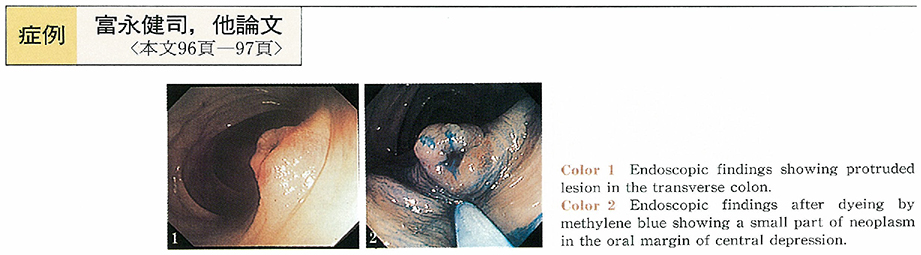
1999Volume 55Issue 2 Pages 96-97
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (679K) -
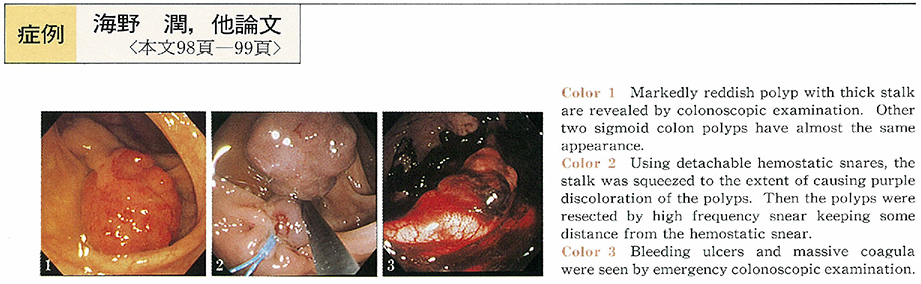
1999Volume 55Issue 2 Pages 98-99
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (664K) -
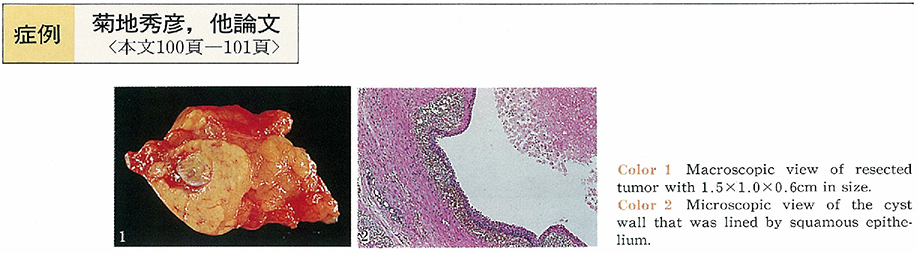
1999Volume 55Issue 2 Pages 100-101
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (582K) -
1999Volume 55Issue 2 Pages 102-103
Published: November 25, 1999
Released on J-STAGE: October 28, 2014
Download PDF (623K)
- |<
- <
- 1
- >
- >|