巻号一覧

64 巻 (2004)
- 2 号 p. 1-
64 巻, 2 号
選択された号の論文の55件中51~55を表示しています
症例
-
小野里 康博, 飯塚 春尚, 荒川 和久, 新井 弘隆, 阿部 毅彦, 石原 弘, 富沢 直樹, 小川 哲史, 伊藤 秀明2004 年 64 巻 2 号 p. 136-137
発行日: 2004/06/10
公開日: 2014/03/28
ジャーナル フリーA 65 year old man underwent colonoscopy for positive occult blood test. Anapporoximately 30 mm flat elevated granular tumor was detected in the sigmoid colon. Submucosal dissection EMR wasperformed and the tumor was successfully resected en bloc. But colonic perforation was caused by electric hemostasis under submucosal dissection. Endoscopic clip suture was performed immediately and a transanal intraluminal drainage tube was left indwelling for a week after EMR. The colonic perforation improved without peritonitis. The resected specimen was 37×31 mm, and the pathological finding was well-differentiated adenocarcinoma in adenoma without submucosal invasion with negative marigins. Therefore additional surgery was not performed.
Submucosal dissection EMR is useful for lateral spreading tumor but has high risk for colonic perforation. Endscopic clip suture and indwelling transanal intraluminal drainage tube can treat colonic perforation without peritonitis or surgical operation.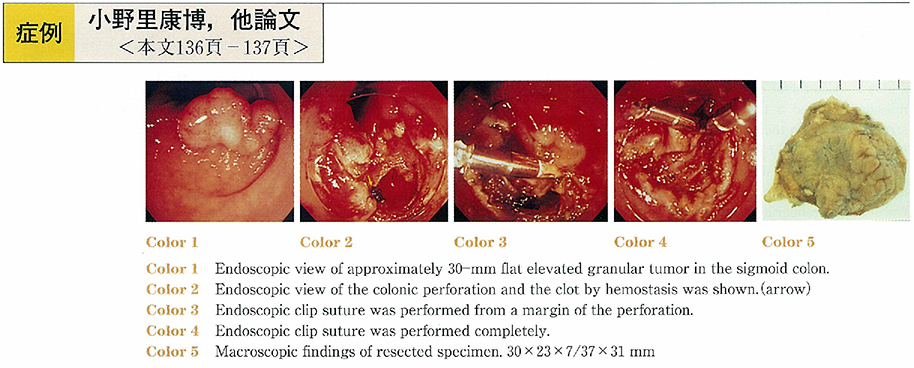 抄録全体を表示PDF形式でダウンロード (565K)
抄録全体を表示PDF形式でダウンロード (565K) -
伊藤 謙, 三村 享彦, 渡辺 利泰, 佐藤 大介, 岡野 直樹, 三浦 富宏, 五十嵐 良典, 飯田 和成, 住野 泰清, 三木 一正2004 年 64 巻 2 号 p. 138-139
発行日: 2004/06/10
公開日: 2014/03/28
ジャーナル フリーCase : An 86-year-old female was presented with flu-like symptoms for a month. A chest X-P revealed pneumonia which was treated with antibiotics. Laboratory examination showed elevated hepatobiliary enzymes, suggesting cholangitis. Endoscopic retrograde cholangiopancreatography (ERCP) revealed no choledocholithiasis, but a huge juxtapapillary duodenal diverticula (JPD) which was compressing the lower common bile duct. We diagnosed Lemmel's syndrome, and performed drainage via ERCP. Despite a needle knife endoscopic sphincterotomy, the patient continued to show elevated hepatobiliary enzymes. Accordingly, we treated her by placing a stent (7 Fr pigtail tail type) across the sphincter of Oddi. The stent was pushed along a guide wire through the cystic duct and then down the common bile duct. The patient did well post-operatively and was discharged. The stent was replaced 2 months later and removed 4 months later. The scintigraphy of the biliary tract revealed excellent drainage. Conclusion : Drainage and stenting via endoscopic retrograde cholangiopancreatography (ERCP) was effective treatment for Lemmel's syndrome 抄録全体を表示PDF形式でダウンロード (674K)
抄録全体を表示PDF形式でダウンロード (674K) -
石井 直樹, 平田 信人, 角岡 真帆, 杉山 政彦, 小田島 慎也, 黒目 学, 亀岡 博, 藪 剛爾, 和田 亮一, 光島 徹2004 年 64 巻 2 号 p. 140-141
発行日: 2004/06/10
公開日: 2014/03/28
ジャーナル フリーA 87-year-old woman was admitted to our hospital with fever and jaundice. Ultrasonography showed the hyperechoic mass in the dilated common bile duct. Computed tomography and MR cholangiography demonstrated dilatation of the bile duct, cystic lesions in the tail of the pancreas, and the communication between common bile duct and dilated branch of pancreatic duct in the head of the pancreas. Endoscopy showed dilatation of the orifice of the major papilla and the minor papilla caused by mucus flow. Endoscopic retrograde cholangiopancreaticography revealed mucus in the dilated common bile duct and the fistula between common bile duct and the dilated branch of pancreatic duct. These findings were characteristic of intraductal papillary tumor with biliopancreatic fistula. Endoscopic sphincterotomy was performed and a plastic stent was placed in the common bile duct. A few days later, fever and jaundice disappeared. Endoscopic therapy was useful for patients with bile duct obstruction and jaundice due to masses of mucus. 抄録全体を表示PDF形式でダウンロード (652K)
抄録全体を表示PDF形式でダウンロード (652K) -
氏家 幸子, 中野 史郎, 奥脇 裕介, 穴澤 康志, 蓮見 桂三, 森野 文敏, 大野 隆, 中安 邦夫, 篠田 政幸, 熊木 伸枝2004 年 64 巻 2 号 p. 142-143
発行日: 2004/06/10
公開日: 2014/03/28
ジャーナル フリーA 67-year-old man came to our hospital with a chief complaint of jaundice and itching. Abdominal ultrasonography and computed tomography showed cystic tumor of the pancreas head and dilatation of the bile and pancreatic ducts. After we diagnosed obstructive jaundice, we performed percutanous transhepatic cholangio-drainage. Magnetic resonance cholangiopancreatography and percutanous transhepatic cholangiography showed fistulous communication with pancreatic duct and common bile duct. We performed percutanous transhepatic cholangioscope, in result we found mucinous ductal ectasia into the through pancreatico-cholangio-fistula. Under the diagnosis of intraductal papillary mucinous tumor (adenoma) , the patient was treated by pancreatico-duodenectomy. Histological examination of the specimen showed invasive carcinoma drived from IPMT, accompanied by invasion into CBD. We reported the case of IPMT with obstructive jaundice due to mucus through pancreatico-cholangio-fistula.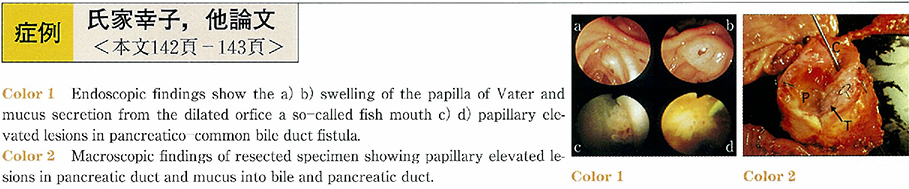 抄録全体を表示PDF形式でダウンロード (487K)
抄録全体を表示PDF形式でダウンロード (487K) -
小野 千尋, 八重樫 寛治, 小野 未来代2004 年 64 巻 2 号 p. 144-145
発行日: 2004/06/10
公開日: 2014/03/28
ジャーナル フリーA 59-year-old male patient had developed obstructive jaundice and was admitted to the Department of Surgery, Soka Municipal Hospital for further diagnosis and treatment. He had the history of being suspected to have diabetes mellitus because of hyperglycemia three years before, but had no history of autoimmune diseases. A physical examination on admission revealed jaundice, but no other abnormal findings. Abdominal CT scan and MRI showed slight swelling of the entire pancreas. Percutaneous transhepatic cholangiography (PTC) showed complete obstruction of the common bile duct in the intrapancreatic portion, with proximal dilatation. Endoscopic retrograde pancreatography (ERP) showed irregular stenosis of the main pancreatic duct in the head and tail of the pancreas. The result of the cytology of the bile juice was Class IIIb. Preoperative diagnosis was common bile duct cancer and pancreaticoduodenectomy was employed. Histological examination of surgical specimen showed severe chronic inflammatory cells infiltration and fibrosis in the pancreas but no cancer cells were observed. Serum IgG4 level four months after operation was as high as 4,400mg/L. The patient was conclusively diagnosed as having autoimmune pancreatitis. It is very important to be well aware of the possibility of the autoimmune panceatitis presenting obstructive jaundice in order to avoid unnecessary operation.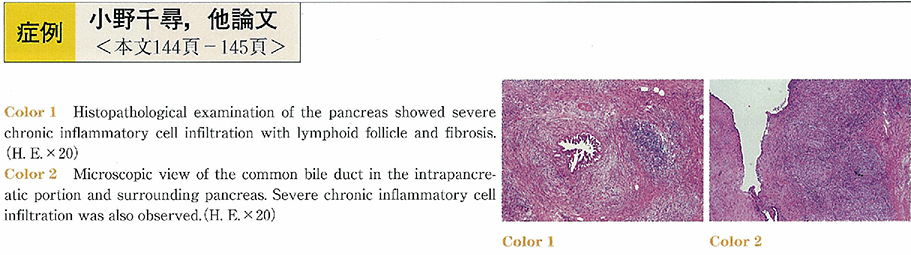 抄録全体を表示PDF形式でダウンロード (913K)
抄録全体を表示PDF形式でダウンロード (913K)