82 巻, 1 号
選択された号の論文の81件中1~50を表示しています
掲載論文カラー写真集
-
2013 年82 巻1 号 p. 1-22
発行日: 2013年
公開日: 2013/07/05
PDF形式でダウンロード (9253K)
内視鏡の器械と技術
-
2013 年82 巻1 号 p. 45-48
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (447K) -
2013 年82 巻1 号 p. 49-52
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (401K) -
2013 年82 巻1 号 p. 53-55
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (348K)
臨床研究
-
2013 年82 巻1 号 p. 56-59
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (263K) -
2013 年82 巻1 号 p. 60-63
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (358K) -
2013 年82 巻1 号 p. 64-67
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (234K) -
2013 年82 巻1 号 p. 68-71
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (330K) -
2013 年82 巻1 号 p. 72-76
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (527K) -
2013 年82 巻1 号 p. 77-81
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (608K) -
2013 年82 巻1 号 p. 82-86
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (682K)
症例
-
2013 年82 巻1 号 p. 87-89
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (293K) -
2013 年82 巻1 号 p. 90-91
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (362K) -
2013 年82 巻1 号 p. 92-93
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (418K) -
2013 年82 巻1 号 p. 94-95
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (261K) -
2013 年82 巻1 号 p. 96-97
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (339K) -
2013 年82 巻1 号 p. 98-99
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (409K) -
2013 年82 巻1 号 p. 100-101
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (398K) -
2013 年82 巻1 号 p. 102-103
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (544K) -
2013 年82 巻1 号 p. 104-105
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (373K) -
2013 年82 巻1 号 p. 106-107
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (267K) -
2013 年82 巻1 号 p. 108-109
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (351K) -
2013 年82 巻1 号 p. 110-111
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (332K) -
2013 年82 巻1 号 p. 112-113
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (416K) -
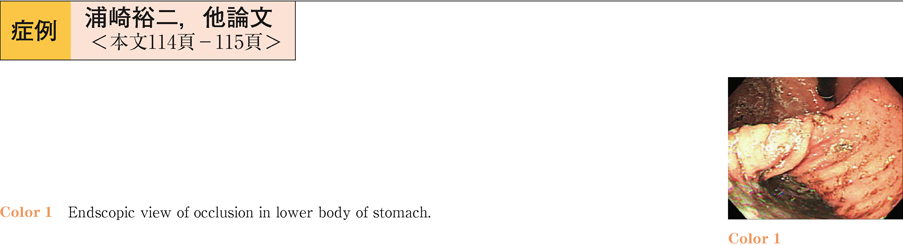
2013 年82 巻1 号 p. 114-115
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (597K) -
2013 年82 巻1 号 p. 116-117
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (419K) -
2013 年82 巻1 号 p. 118-119
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (301K) -
2013 年82 巻1 号 p. 120-121
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (276K) -
2013 年82 巻1 号 p. 122-123
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (386K) -
2013 年82 巻1 号 p. 124-125
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (466K) -
2013 年82 巻1 号 p. 126-127
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (275K) -
2013 年82 巻1 号 p. 128-129
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (480K) -
2013 年82 巻1 号 p. 130-131
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (319K) -
2013 年82 巻1 号 p. 132-133
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (214K) -
2013 年82 巻1 号 p. 134-135
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (498K) -
2013 年82 巻1 号 p. 136-137
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (618K) -
2013 年82 巻1 号 p. 138-139
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (374K) -
2013 年82 巻1 号 p. 140-141
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (452K) -
2013 年82 巻1 号 p. 142-143
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (338K) -
2013 年82 巻1 号 p. 144-145
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (374K) -
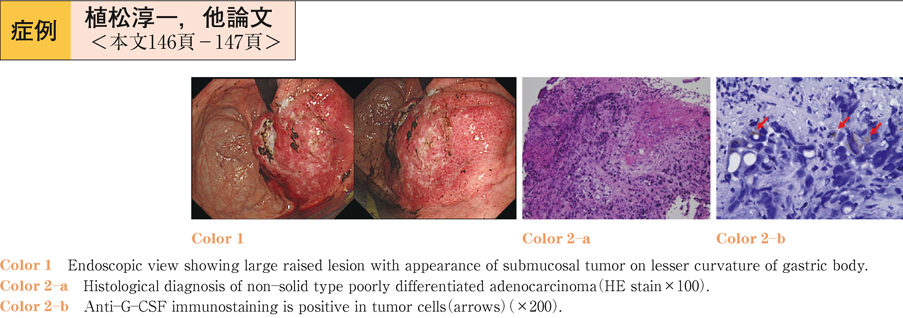
2013 年82 巻1 号 p. 146-147
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (306K) -
2013 年82 巻1 号 p. 148-149
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (249K) -
2013 年82 巻1 号 p. 150-151
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (409K) -
2013 年82 巻1 号 p. 152-153
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (507K) -
2013 年82 巻1 号 p. 154-155
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (358K) -
2013 年82 巻1 号 p. 156-157
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (377K) -
2013 年82 巻1 号 p. 158-159
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (288K) -
2013 年82 巻1 号 p. 160-161
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (300K) -
2013 年82 巻1 号 p. 162-163
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (365K) -
2013 年82 巻1 号 p. 164-165
発行日: 2013/06/14
公開日: 2013/07/05
PDF形式でダウンロード (338K)