84 巻, 1 号
選択された号の論文の78件中1~50を表示しています
掲載論文カラー写真集
-
2014 年84 巻1 号 p. 1-21
発行日: 2014年
公開日: 2014/06/21
PDF形式でダウンロード (23116K)
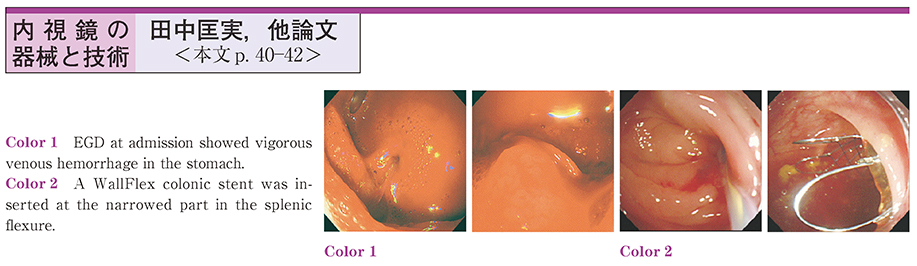
内視鏡の器械と技術
-
2014 年84 巻1 号 p. 40-42
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (808K)
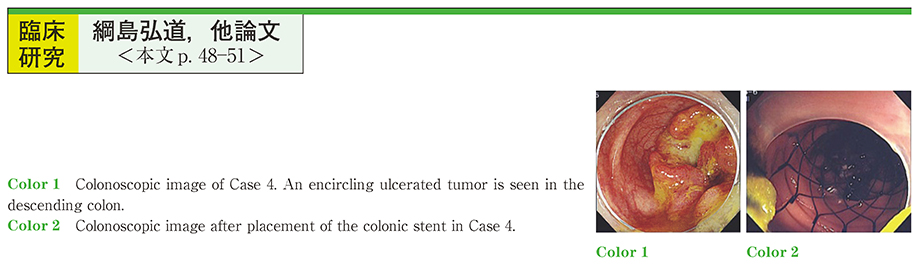
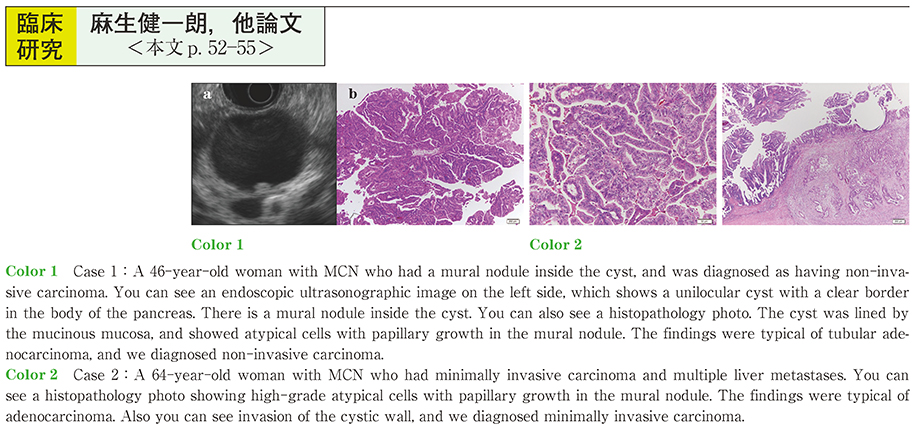
臨床研究
-
2014 年84 巻1 号 p. 43-47
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (491K) -
2014 年84 巻1 号 p. 48-51
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (461K) -
2014 年84 巻1 号 p. 52-55
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (306K) -
2014 年84 巻1 号 p. 56-59
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (273K)
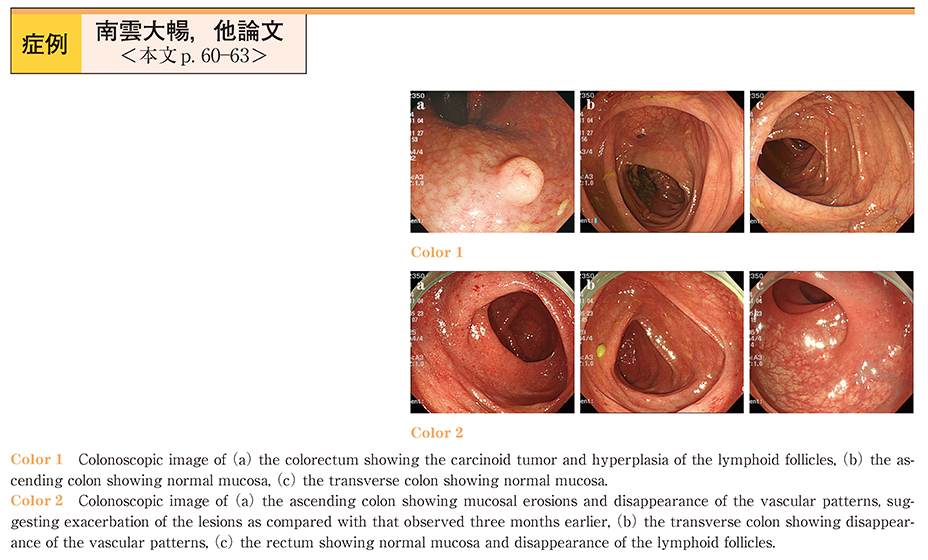
症例
-
2014 年84 巻1 号 p. 60-63
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (1582K)
臨床研究
-
2014 年84 巻1 号 p. 64-65
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (372K)
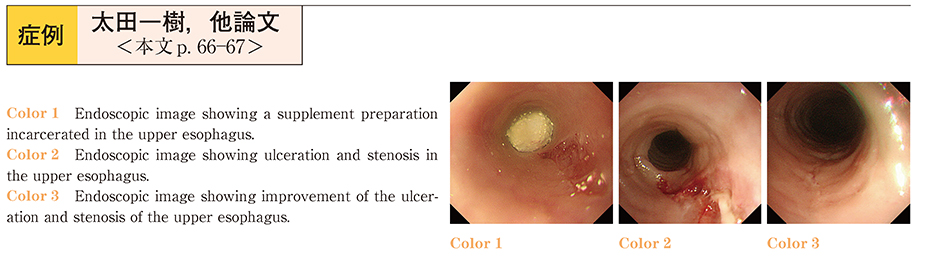
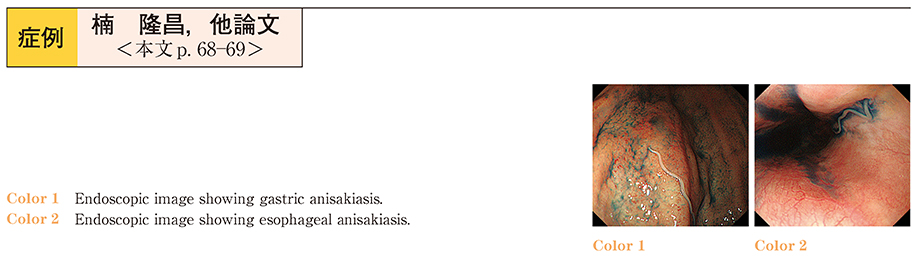
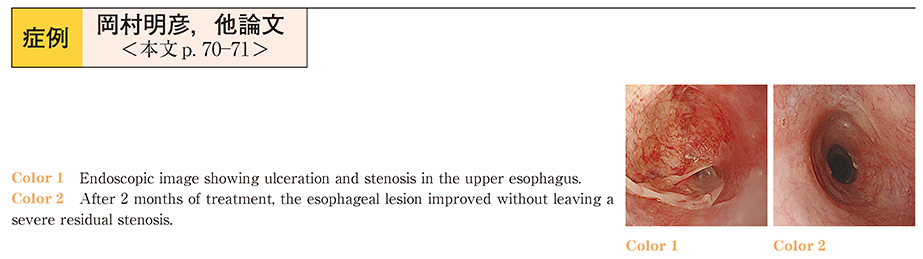
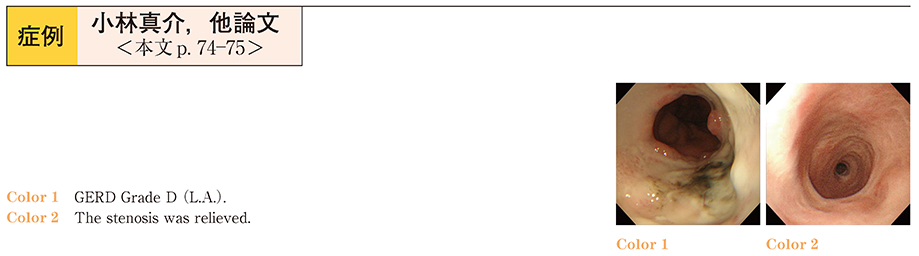
症例
-
2014 年84 巻1 号 p. 66-67
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (283K) -
2014 年84 巻1 号 p. 68-69
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (428K) -
2014 年84 巻1 号 p. 70-71
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (234K) -
2014 年84 巻1 号 p. 72-73
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (434K) -
2014 年84 巻1 号 p. 74-75
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (298K) -
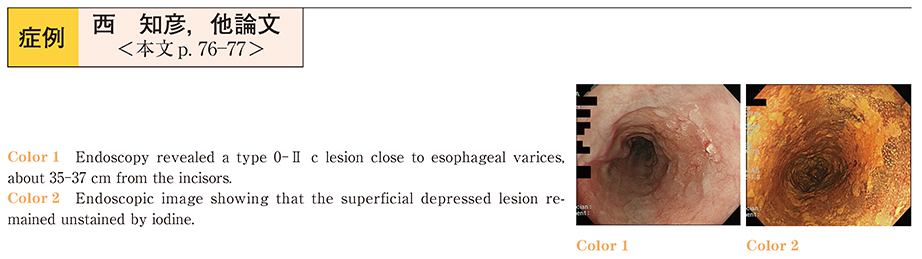
2014 年84 巻1 号 p. 76-77
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (493K) -
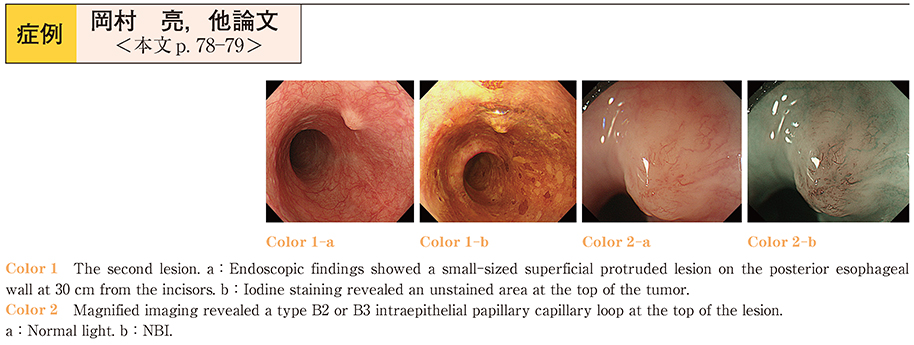
2014 年84 巻1 号 p. 78-79
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (953K) -
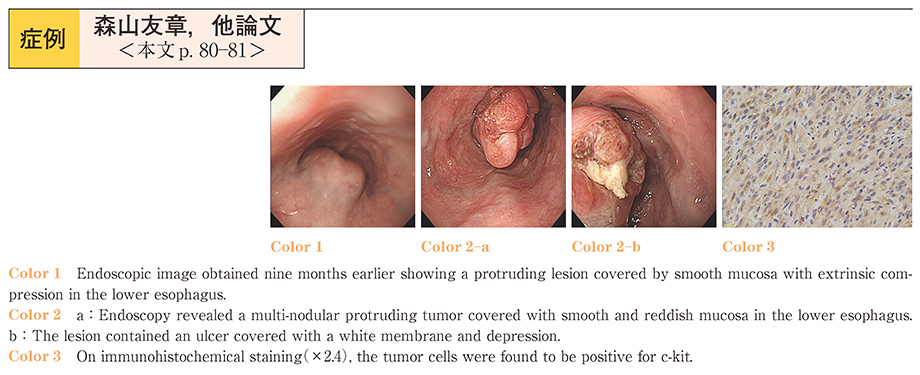
2014 年84 巻1 号 p. 80-81
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (528K) -
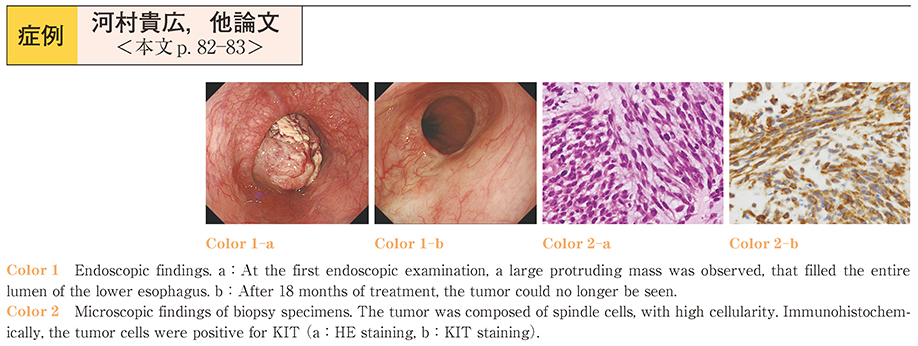
2014 年84 巻1 号 p. 82-83
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (455K) -
2014 年84 巻1 号 p. 84-85
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (232K) -
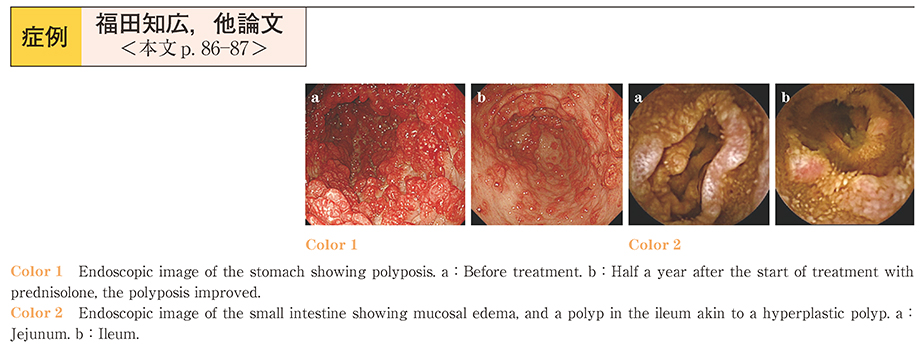
2014 年84 巻1 号 p. 86-87
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (393K) -
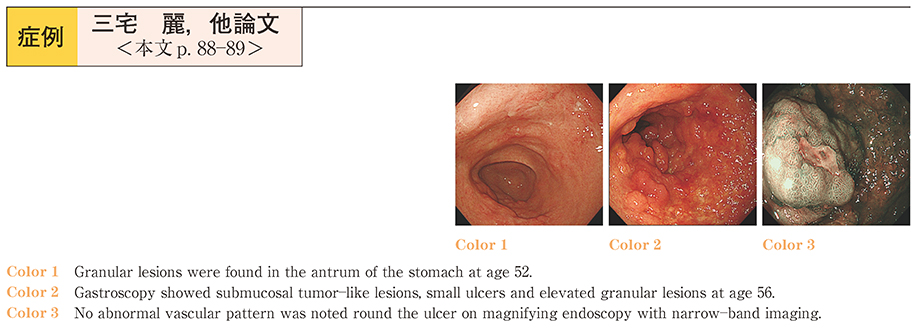
2014 年84 巻1 号 p. 88-89
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (296K) -
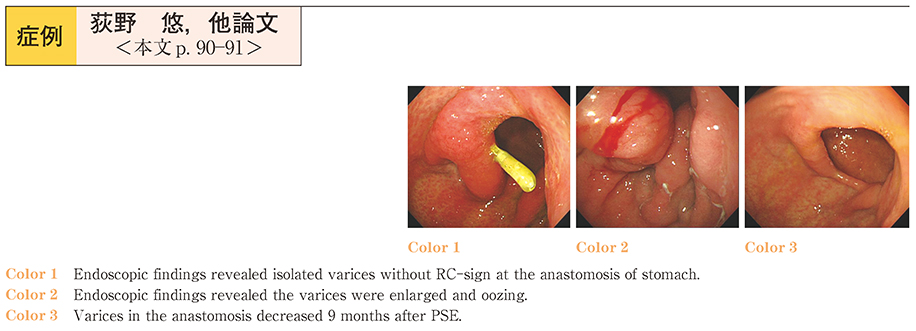
2014 年84 巻1 号 p. 90-91
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (564K) -
2014 年84 巻1 号 p. 92-93
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (587K) -
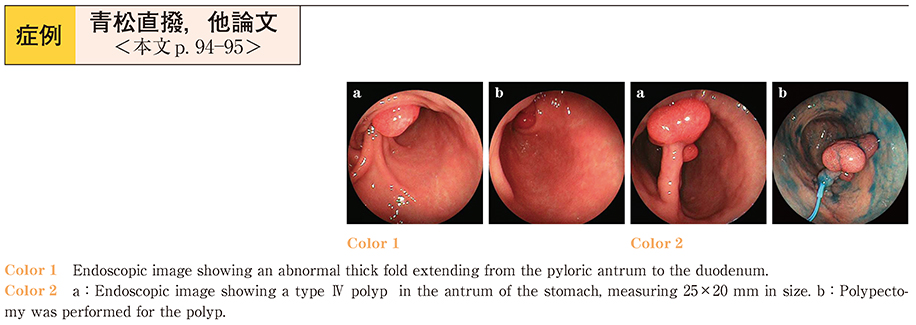
2014 年84 巻1 号 p. 94-95
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (521K) -
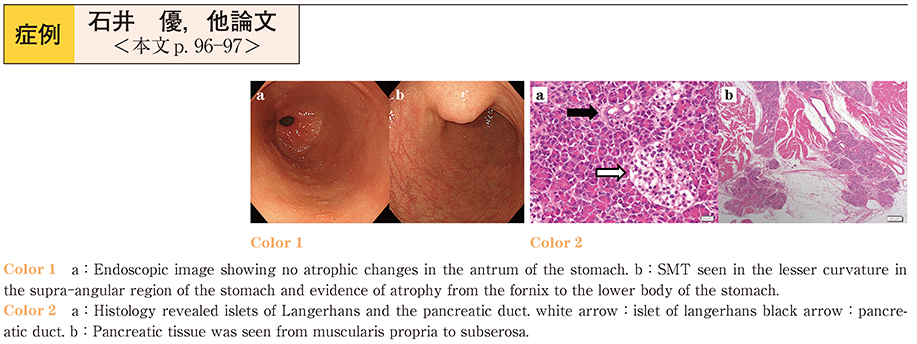
2014 年84 巻1 号 p. 96-97
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (477K) -
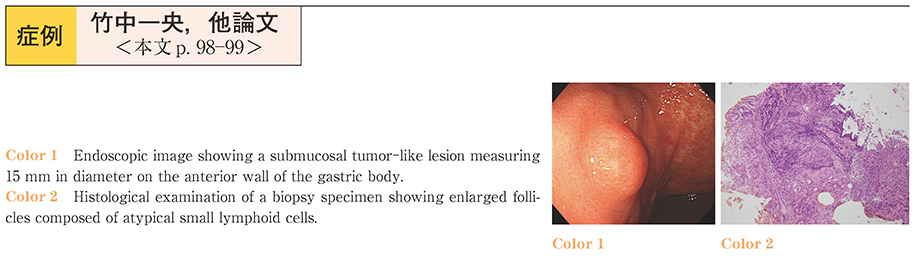
2014 年84 巻1 号 p. 98-99
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (385K) -
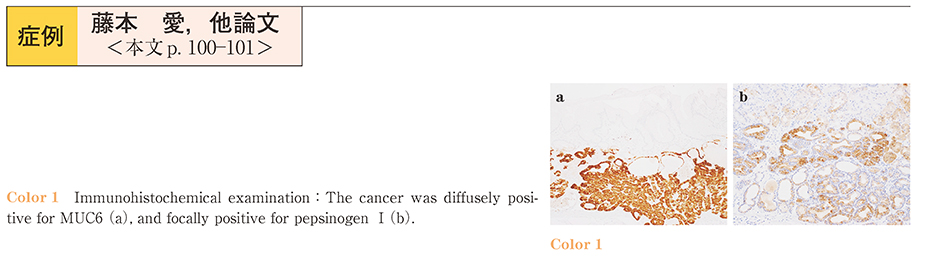
2014 年84 巻1 号 p. 100-101
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (1073K) -
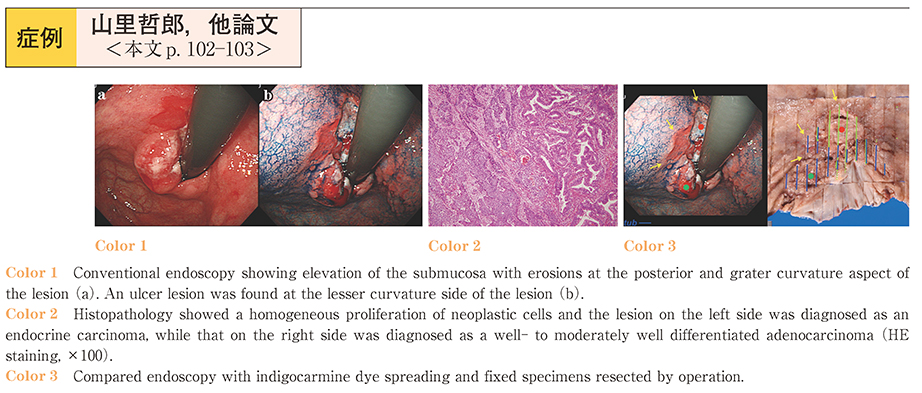
2014 年84 巻1 号 p. 102-103
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (426K) -
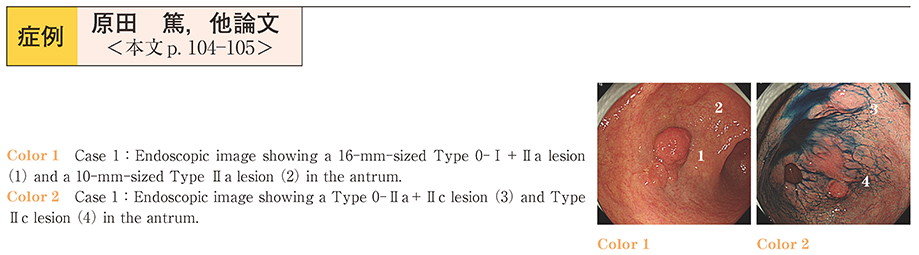
2014 年84 巻1 号 p. 104-105
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (601K) -
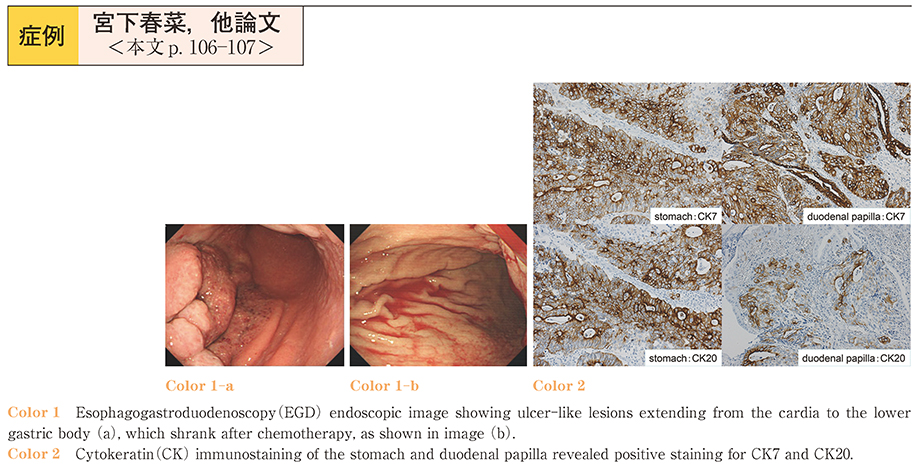
2014 年84 巻1 号 p. 106-107
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (398K) -
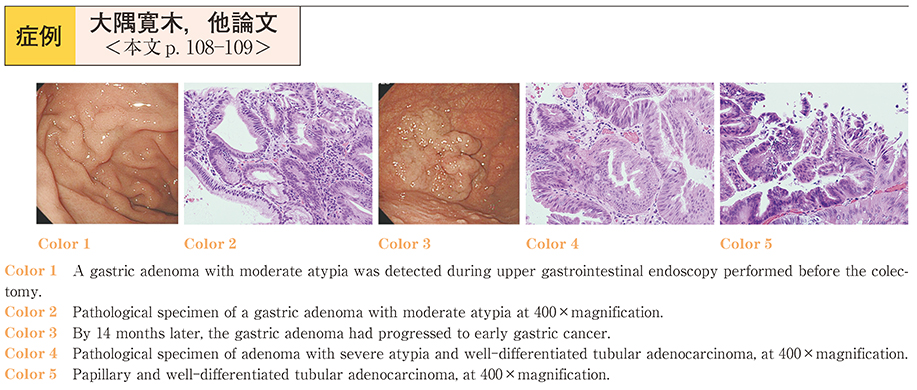
2014 年84 巻1 号 p. 108-109
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (219K) -
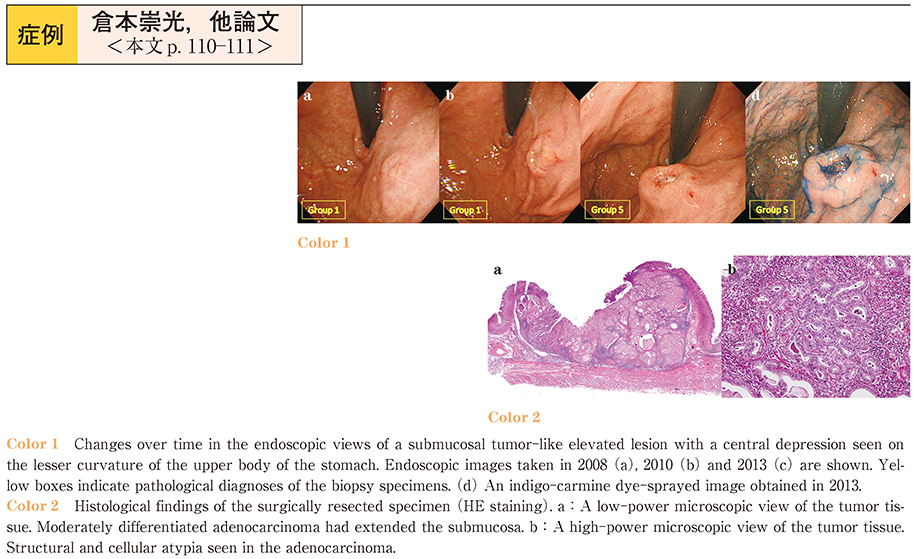
2014 年84 巻1 号 p. 110-111
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (348K) -
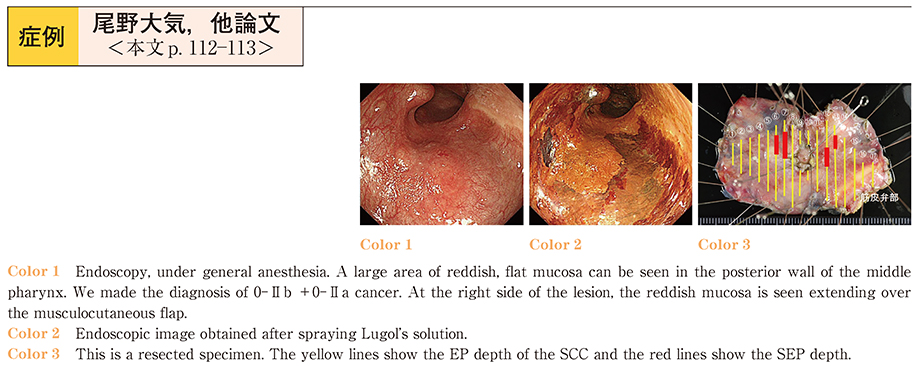
2014 年84 巻1 号 p. 112-113
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (512K) -
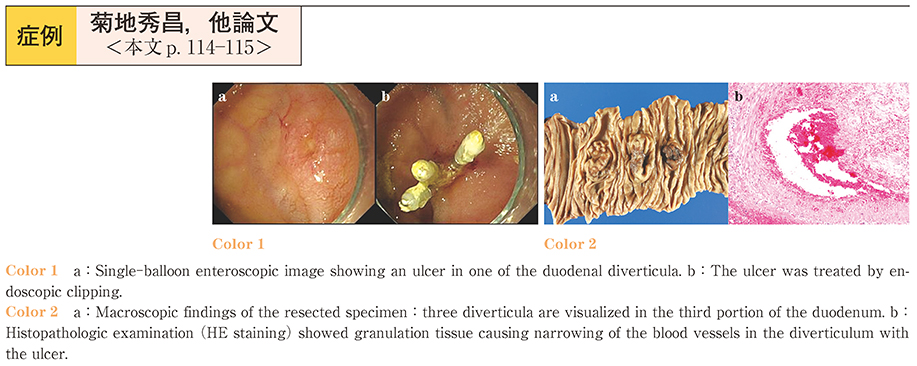
2014 年84 巻1 号 p. 114-115
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (445K) -
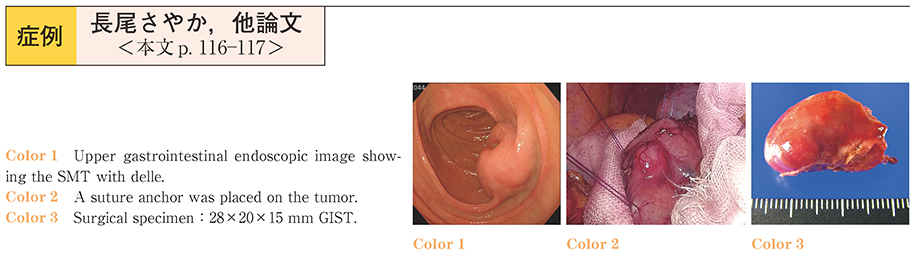
2014 年84 巻1 号 p. 116-117
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (347K) -
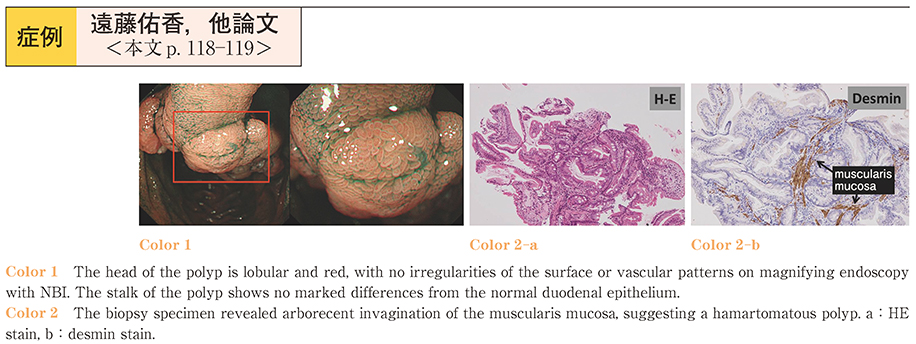
2014 年84 巻1 号 p. 118-119
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (720K) -
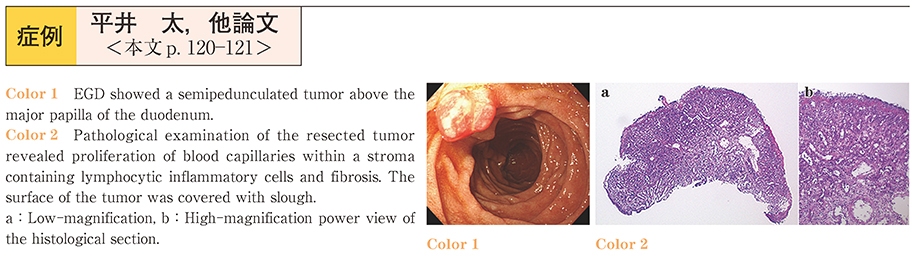
2014 年84 巻1 号 p. 120-121
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (598K) -
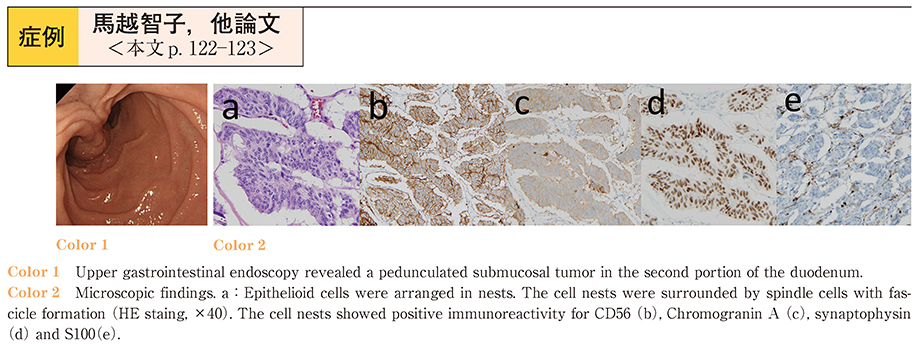
2014 年84 巻1 号 p. 122-123
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (576K) -
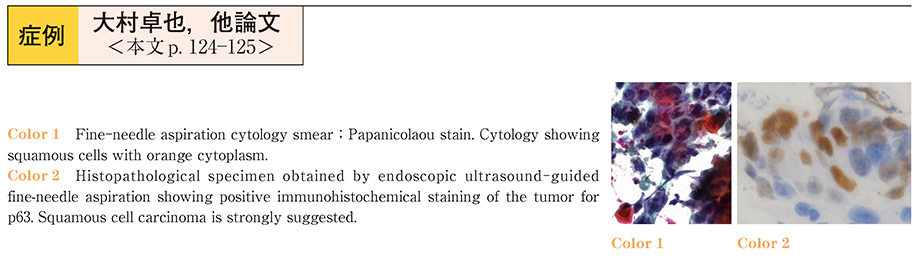
2014 年84 巻1 号 p. 124-125
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (271K) -
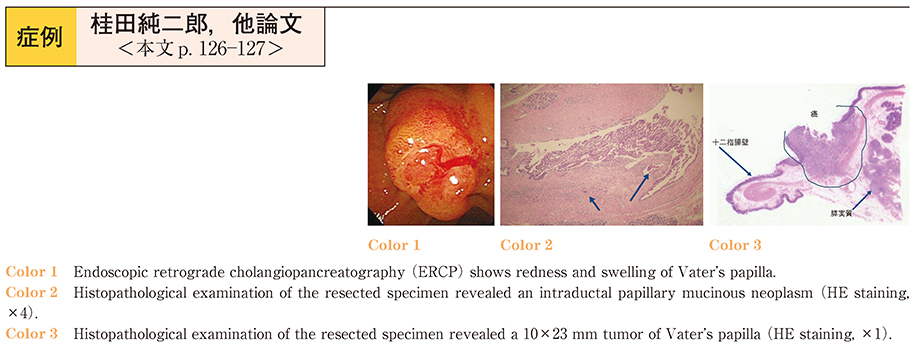
2014 年84 巻1 号 p. 126-127
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (629K) -
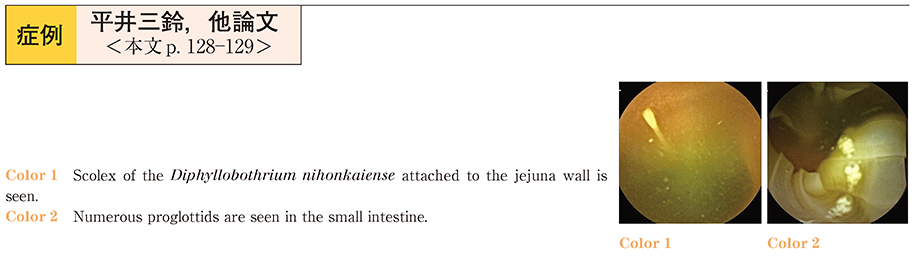
2014 年84 巻1 号 p. 128-129
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (453K) -
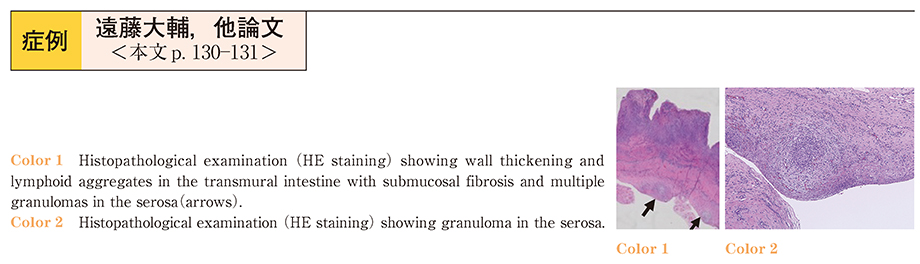
2014 年84 巻1 号 p. 130-131
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (476K) -
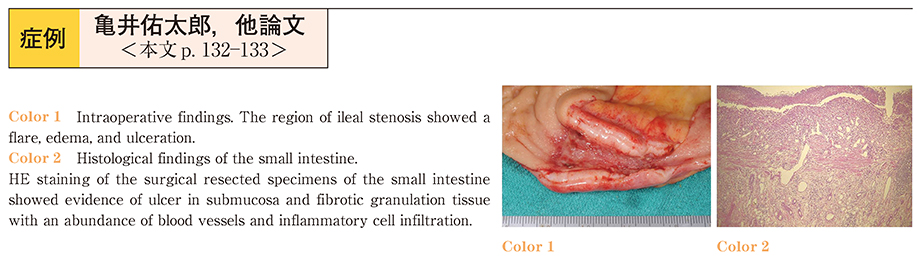
2014 年84 巻1 号 p. 132-133
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (457K) -
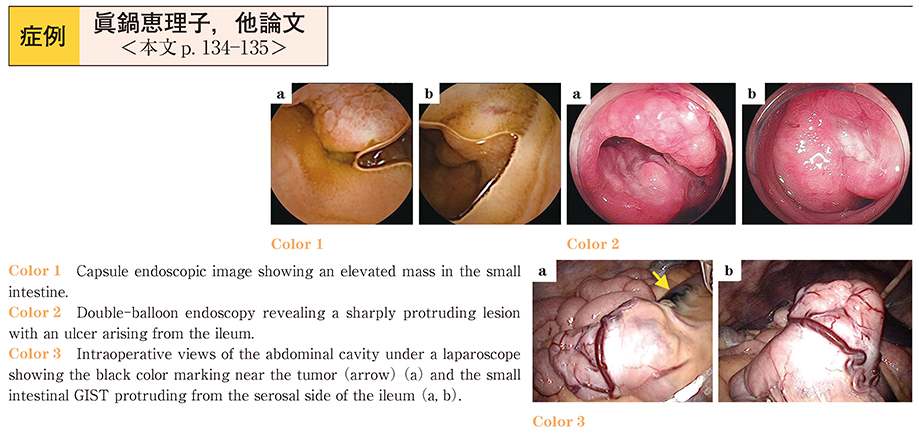
2014 年84 巻1 号 p. 134-135
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (806K) -
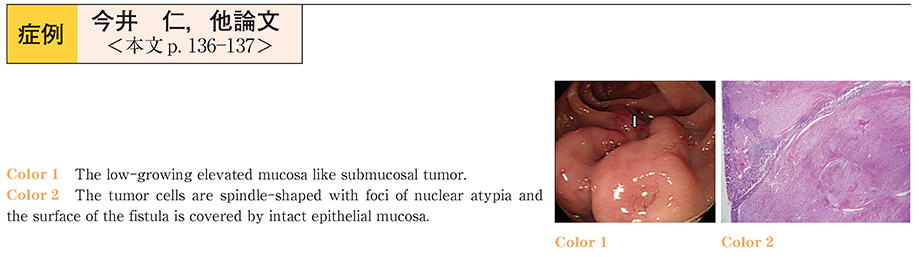
2014 年84 巻1 号 p. 136-137
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (445K) -
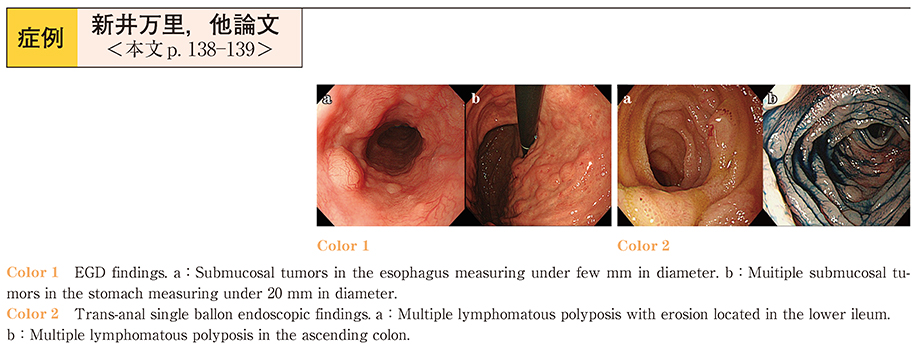
2014 年84 巻1 号 p. 138-139
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (612K) -
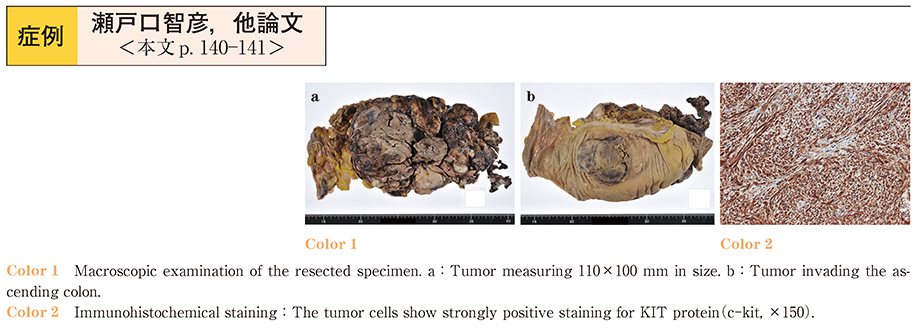
2014 年84 巻1 号 p. 140-141
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (467K) -
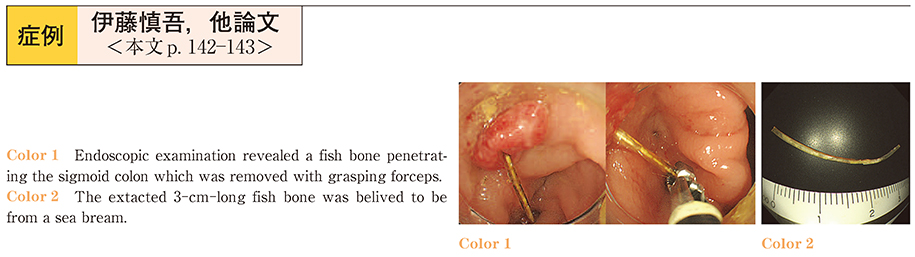
2014 年84 巻1 号 p. 142-143
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (478K) -
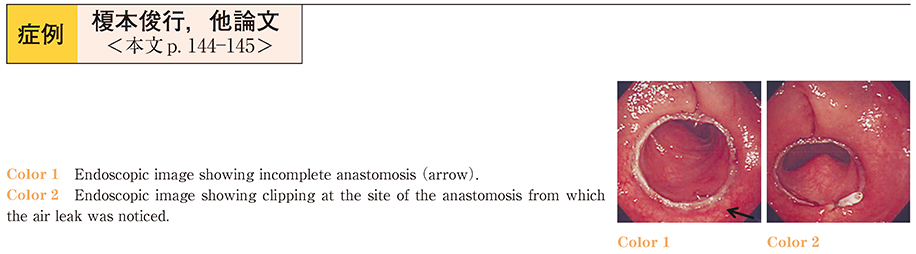
2014 年84 巻1 号 p. 144-145
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (476K) -
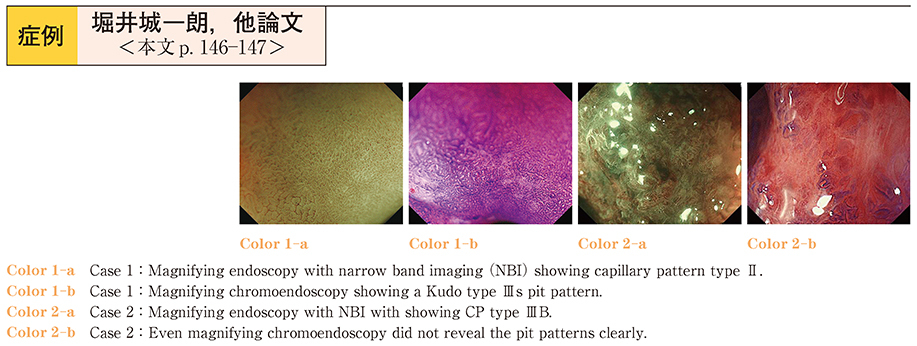
2014 年84 巻1 号 p. 146-147
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (485K) -
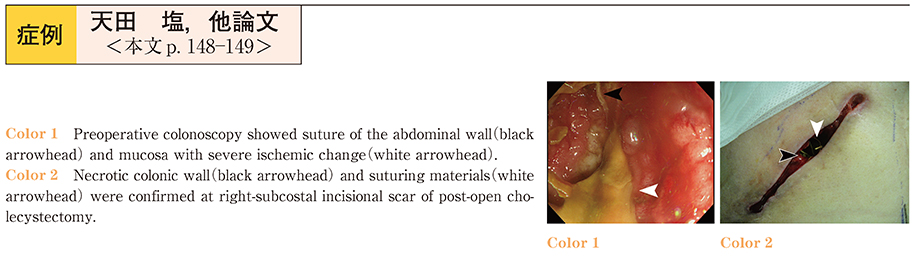
2014 年84 巻1 号 p. 148-149
発行日: 2014/06/14
公開日: 2014/06/21
PDF形式でダウンロード (403K)