83 巻, 1 号
選択された号の論文の79件中51~79を表示しています
症例
-
2013 年 83 巻 1 号 p. 160-161
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (629K) -
2013 年 83 巻 1 号 p. 162-163
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (539K) -
2013 年 83 巻 1 号 p. 164-165
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (411K) -
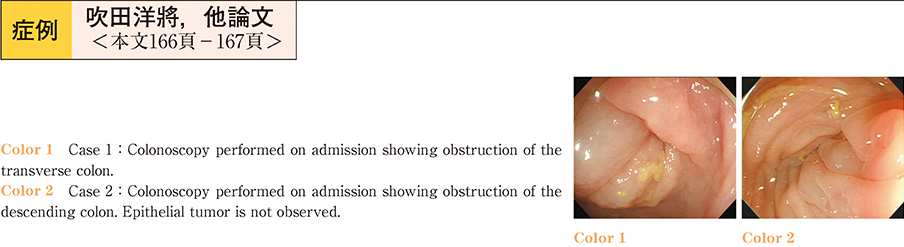
2013 年 83 巻 1 号 p. 166-167
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (945K) -
2013 年 83 巻 1 号 p. 168-169
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (639K) -
2013 年 83 巻 1 号 p. 170-171
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (420K) -
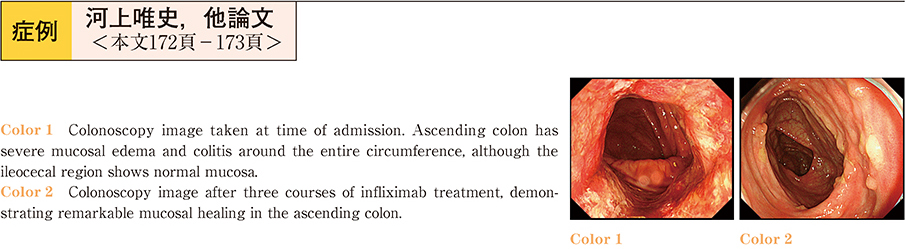
2013 年 83 巻 1 号 p. 172-173
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (741K) -
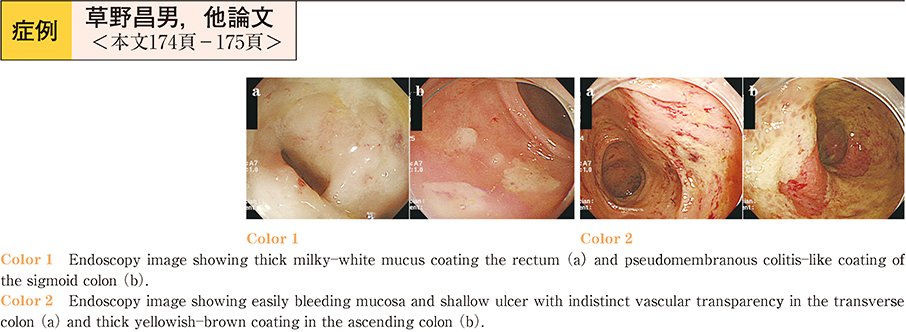
2013 年 83 巻 1 号 p. 174-175
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (530K) -
2013 年 83 巻 1 号 p. 176-177
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (270K) -
2013 年 83 巻 1 号 p. 178-179
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (784K) -
2013 年 83 巻 1 号 p. 180-181
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (493K) -
2013 年 83 巻 1 号 p. 182-183
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (296K) -
2013 年 83 巻 1 号 p. 184-185
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (601K) -
2013 年 83 巻 1 号 p. 186-187
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (570K) -
2013 年 83 巻 1 号 p. 188-189
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (604K) -
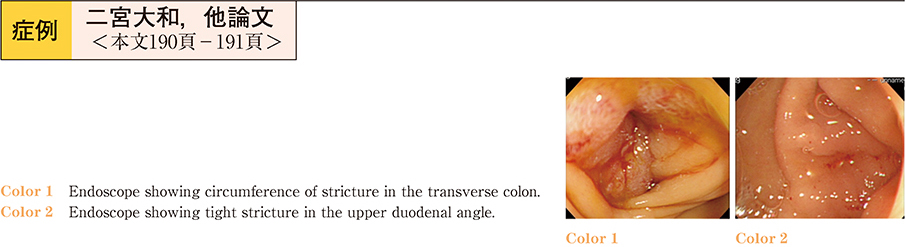
2013 年 83 巻 1 号 p. 190-191
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (499K) -
2013 年 83 巻 1 号 p. 192-193
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (678K) -
2013 年 83 巻 1 号 p. 194-195
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (972K) -
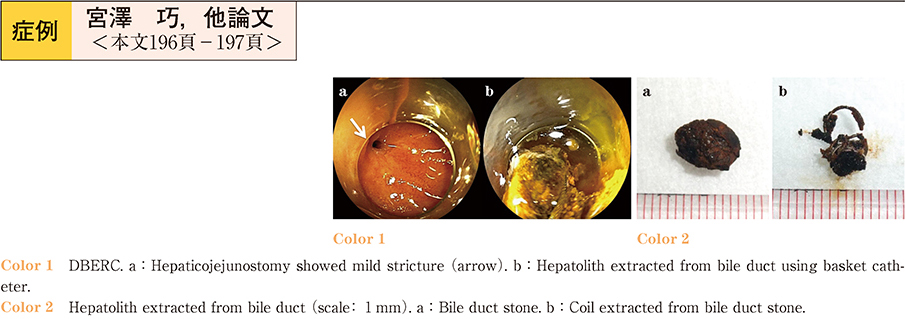
2013 年 83 巻 1 号 p. 196-197
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (390K) -
2013 年 83 巻 1 号 p. 198-199
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (816K) -
2013 年 83 巻 1 号 p. 200-201
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (511K) -
2013 年 83 巻 1 号 p. 202-203
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (764K) -
2013 年 83 巻 1 号 p. 204-205
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (489K) -
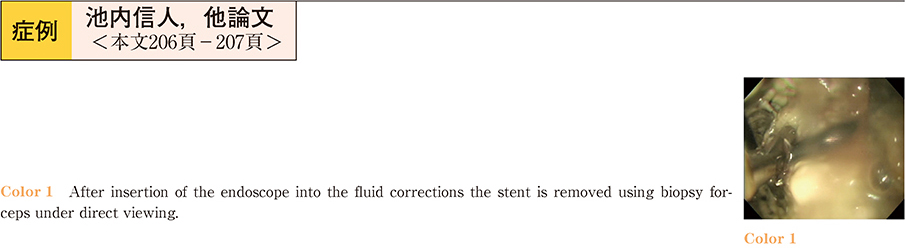
2013 年 83 巻 1 号 p. 206-207
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (449K) -
2013 年 83 巻 1 号 p. 208-209
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (705K) -
2013 年 83 巻 1 号 p. 210-211
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (432K) -
2013 年 83 巻 1 号 p. 212-213
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (616K) -
2013 年 83 巻 1 号 p. 214-215
発行日: 2013/12/14
公開日: 2013/12/21
PDF形式でダウンロード (745K)
お詫びと訂正
-
2013 年 83 巻 1 号 p. 238
発行日: 2013年
公開日: 2013/12/21
PDF形式でダウンロード (195K)