Volume 92, Issue 1
Displaying 1-50 of 60 articles from this issue
Clinical study
-
2018Volume 92Issue 1 Pages 44-49
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (852K) -
2018Volume 92Issue 1 Pages 50-53
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (724K) -
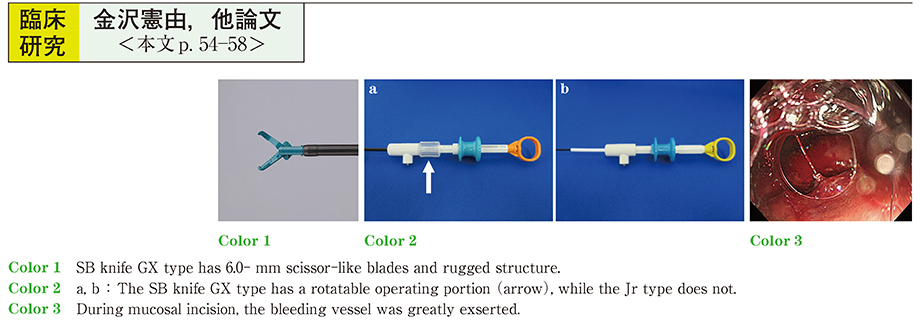
2018Volume 92Issue 1 Pages 54-58
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (813K) -
2018Volume 92Issue 1 Pages 59-63
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (943K) -
2018Volume 92Issue 1 Pages 64-68
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (1127K) -
2018Volume 92Issue 1 Pages 69-73
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (1063K)
Case report
-
2018Volume 92Issue 1 Pages 74-76
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (927K)
Clinical study
-
2018Volume 92Issue 1 Pages 78-79
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (578K) -
2018Volume 92Issue 1 Pages 80-81
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (644K)
Clinical study
-
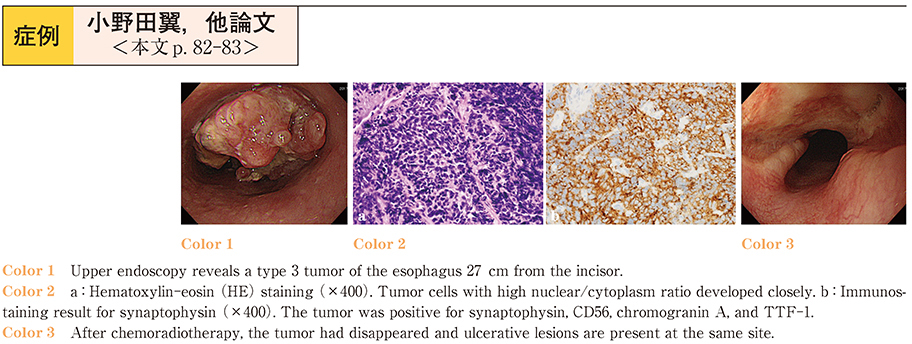
2018Volume 92Issue 1 Pages 82-83
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (775K) -
2018Volume 92Issue 1 Pages 84-85
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (595K) -
2018Volume 92Issue 1 Pages 86-87
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (997K) -
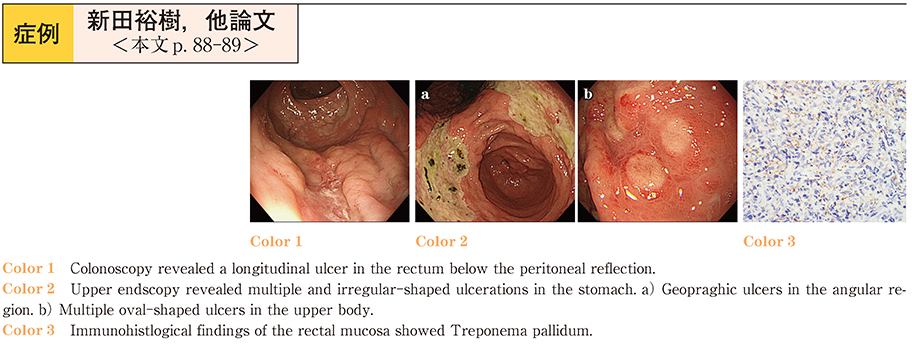
2018Volume 92Issue 1 Pages 88-89
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (739K) -
2018Volume 92Issue 1 Pages 90-91
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (1132K) -
2018Volume 92Issue 1 Pages 92-93
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (869K) -
2018Volume 92Issue 1 Pages 94-95
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (1019K) -
2018Volume 92Issue 1 Pages 96-97
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (1044K) -
2018Volume 92Issue 1 Pages 98-99
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (796K) -
2018Volume 92Issue 1 Pages 100-101
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (632K) -
2018Volume 92Issue 1 Pages 102-103
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (563K) -
2018Volume 92Issue 1 Pages 104-105
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (580K) -
2018Volume 92Issue 1 Pages 106-107
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (963K) -
2018Volume 92Issue 1 Pages 108-109
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (898K) -
2018Volume 92Issue 1 Pages 110-111
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (624K) -
2018Volume 92Issue 1 Pages 112-113
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (789K) -
2018Volume 92Issue 1 Pages 114-115
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (674K) -
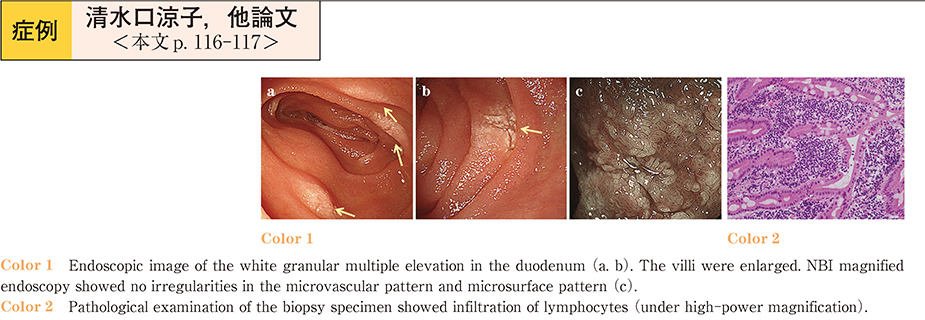
2018Volume 92Issue 1 Pages 116-117
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (642K) -
2018Volume 92Issue 1 Pages 118-119
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (856K) -
2018Volume 92Issue 1 Pages 120-121
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (1009K) -
2018Volume 92Issue 1 Pages 122-123
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (685K) -
2018Volume 92Issue 1 Pages 124-125
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (903K) -
2018Volume 92Issue 1 Pages 126-127
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (918K) -
2018Volume 92Issue 1 Pages 128-129
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (871K) -
A Patient who Underwent Endoscopic Submucosal Dissection for a Submucosal Tumor Arising in the Cecum2018Volume 92Issue 1 Pages 130-131
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (734K) -
2018Volume 92Issue 1 Pages 132-133
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (881K) -
2018Volume 92Issue 1 Pages 134-135
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (796K) -
2018Volume 92Issue 1 Pages 136-137
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (626K) -
2018Volume 92Issue 1 Pages 138-139
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (607K) -
2018Volume 92Issue 1 Pages 140-141
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (569K) -
2018Volume 92Issue 1 Pages 142-143
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (607K) -
2018Volume 92Issue 1 Pages 144-145
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (818K) -
2018Volume 92Issue 1 Pages 146-147
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (934K) -
2018Volume 92Issue 1 Pages 148-149
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (660K) -
A case of bleeding of choledocho-jejuno anastomosis successfully treated by argon plasma coagulation2018Volume 92Issue 1 Pages 150-151
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (887K) -
2018Volume 92Issue 1 Pages 152-153
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (811K) -
2018Volume 92Issue 1 Pages 154-155
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (669K) -
2018Volume 92Issue 1 Pages 156-157
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (926K) -
2018Volume 92Issue 1 Pages 158-159
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (801K) -
2018Volume 92Issue 1 Pages 160-161
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (800K) -
2018Volume 92Issue 1 Pages 162-163
Published: June 15, 2018
Released on J-STAGE: July 19, 2018
Download PDF (681K)