Volume 60, Issue 2
Displaying 1-30 of 30 articles from this issue
- |<
- <
- 1
- >
- >|
-
2002 Volume 60 Issue 2 Pages 1-8
Published: 2002
Released on J-STAGE: May 22, 2014
Download PDF (7661K)
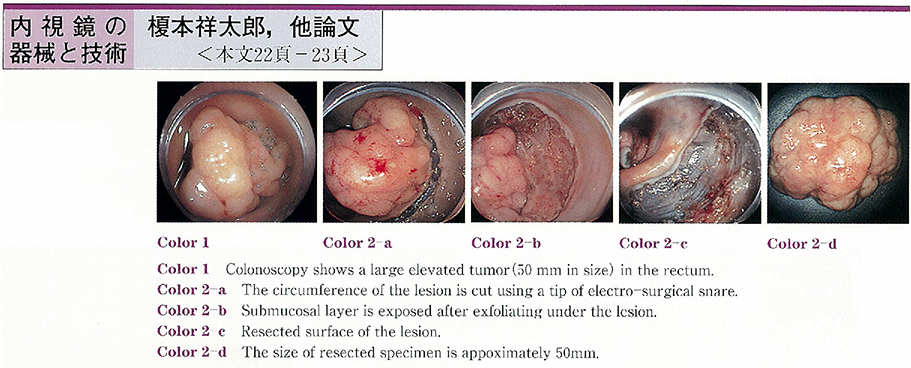
Technology and instrument
-
2002 Volume 60 Issue 2 Pages 22-24
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (1056K) -
2002 Volume 60 Issue 2 Pages 25-27
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (674K)
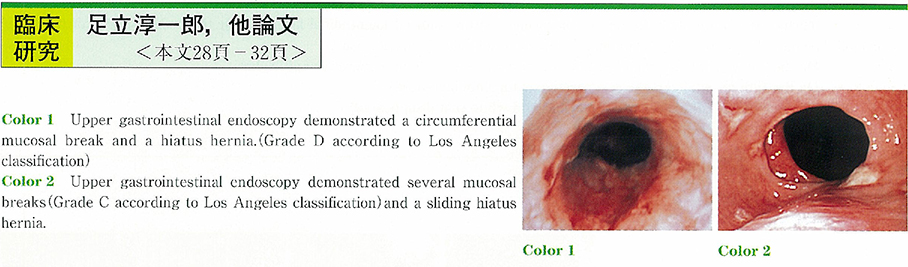
Clinical study
-
2002 Volume 60 Issue 2 Pages 28-32
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (1680K)
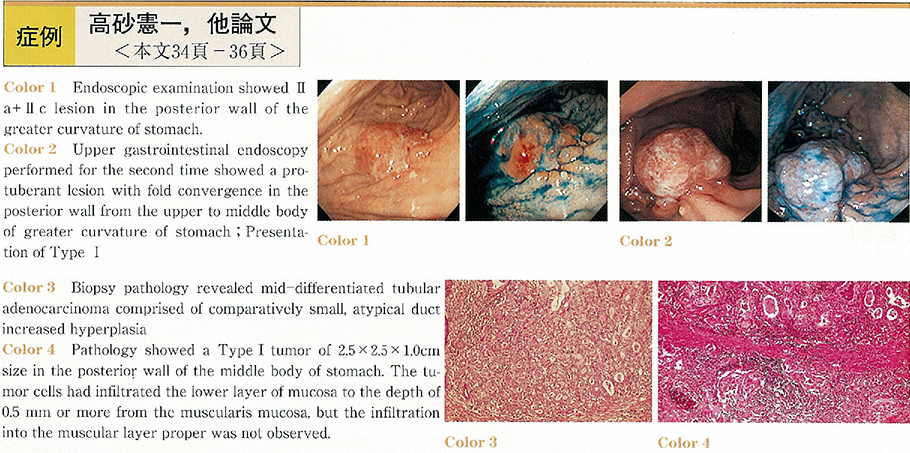
Case report
-
2002 Volume 60 Issue 2 Pages 34-36
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (532K) -
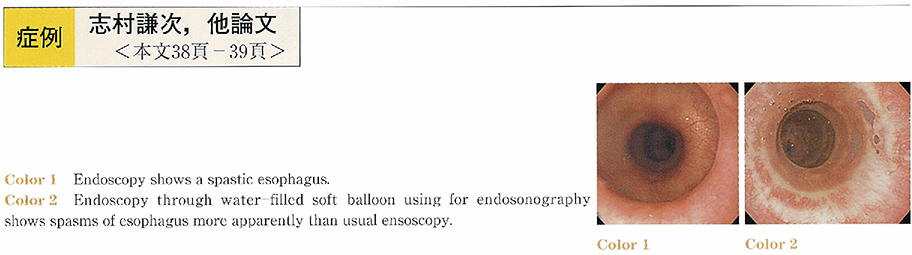
2002 Volume 60 Issue 2 Pages 38-39
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (826K) -
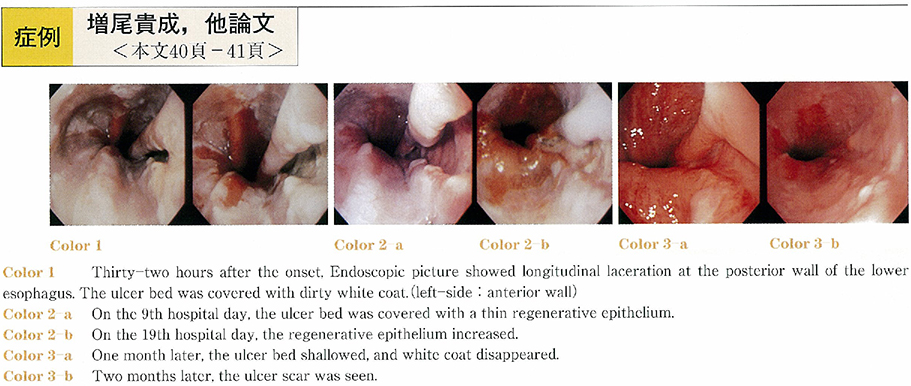
2002 Volume 60 Issue 2 Pages 40-41
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (894K) -
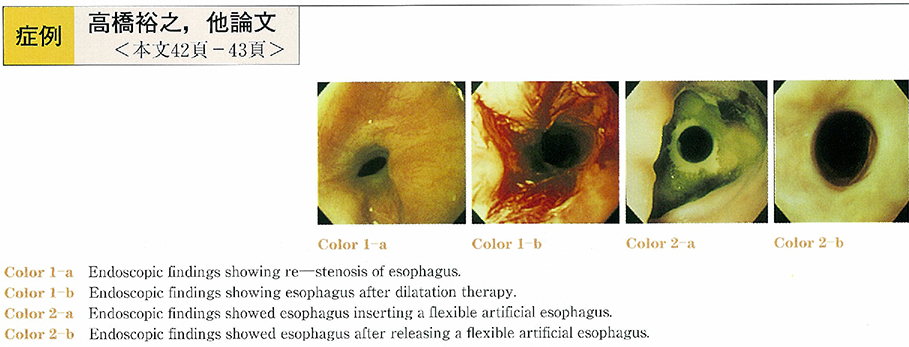
2002 Volume 60 Issue 2 Pages 42-43
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (698K) -
2002 Volume 60 Issue 2 Pages 44-46
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (386K) -
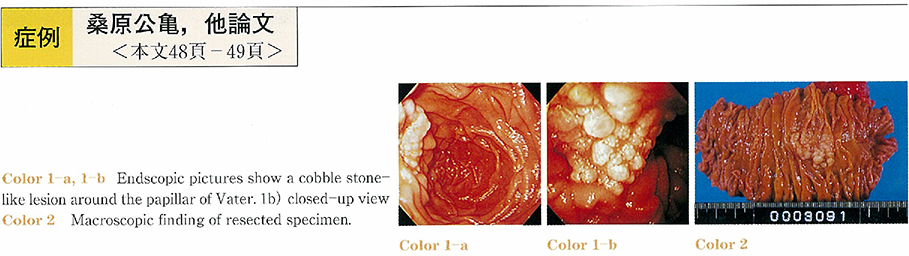
2002 Volume 60 Issue 2 Pages 48-49
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (668K) -
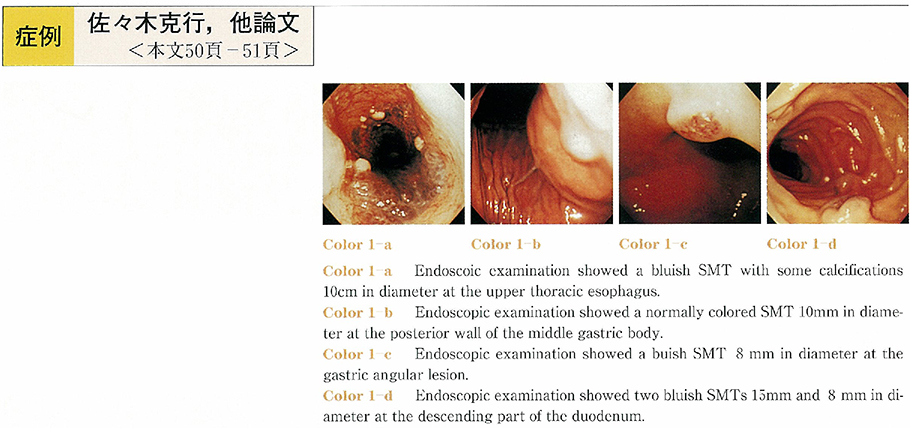
2002 Volume 60 Issue 2 Pages 50-51
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (1215K) -
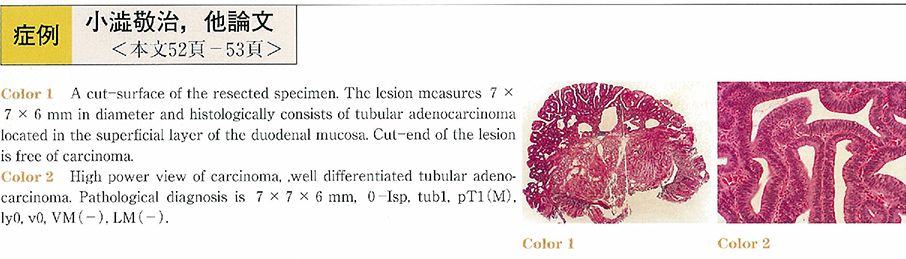
2002 Volume 60 Issue 2 Pages 52-53
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (534K) -
2002 Volume 60 Issue 2 Pages 54-55
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (813K) -
2002 Volume 60 Issue 2 Pages 56-57
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (1102K) -
2002 Volume 60 Issue 2 Pages 58-59
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (659K) -
2002 Volume 60 Issue 2 Pages 60-61
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (713K) -
2002 Volume 60 Issue 2 Pages 62-63
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (535K) -
2002 Volume 60 Issue 2 Pages 64-65
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (877K) -
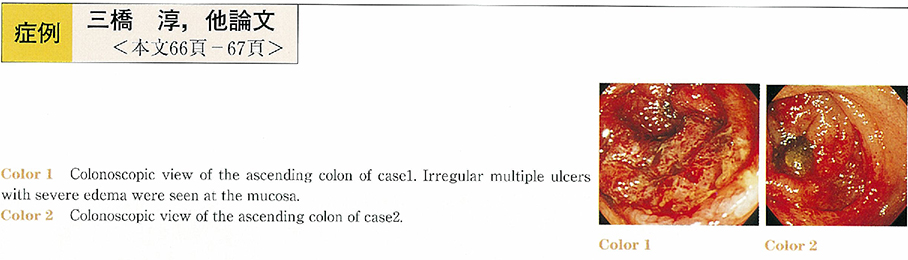
2002 Volume 60 Issue 2 Pages 66-67
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (587K) -
2002 Volume 60 Issue 2 Pages 68-69
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (559K) -
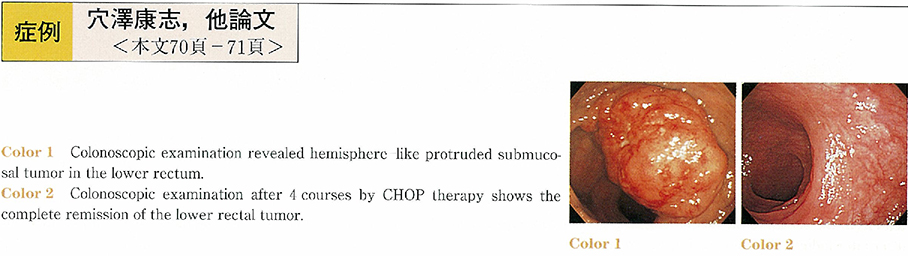
2002 Volume 60 Issue 2 Pages 70-71
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (1021K) -
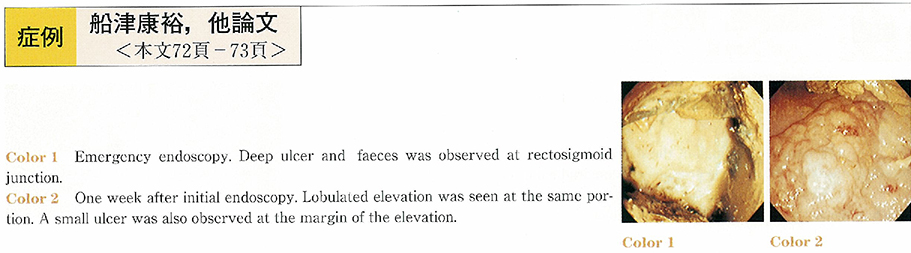
2002 Volume 60 Issue 2 Pages 72-73
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (192K) -
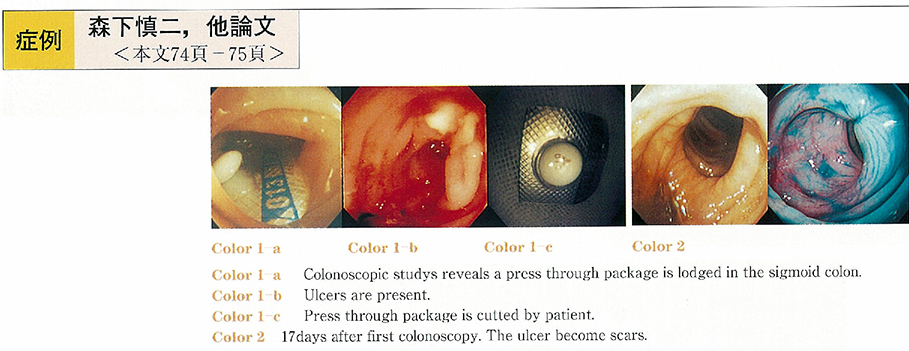
2002 Volume 60 Issue 2 Pages 74-75
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (607K) -
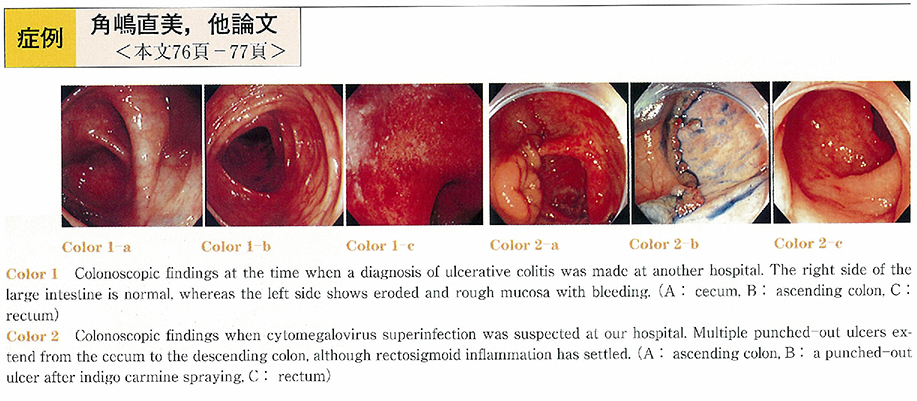
2002 Volume 60 Issue 2 Pages 76-77
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (1238K) -
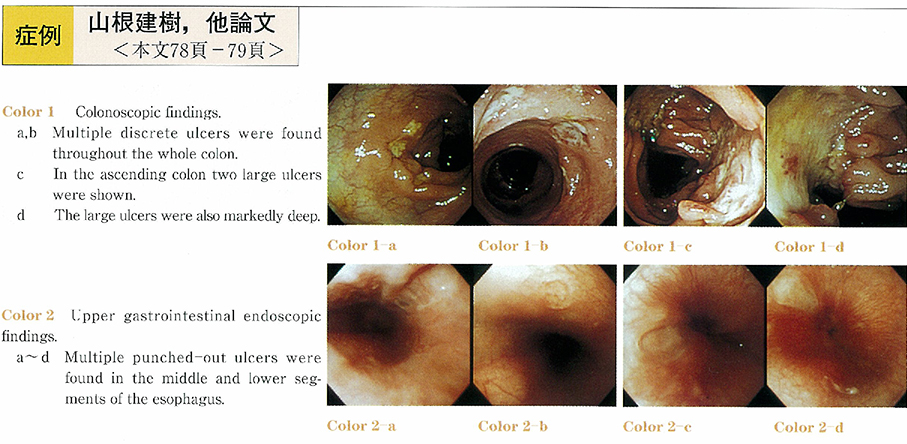
2002 Volume 60 Issue 2 Pages 78-79
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (983K) -
2002 Volume 60 Issue 2 Pages 80-81
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (546K) -
2002 Volume 60 Issue 2 Pages 82-83
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (1212K) -
2002 Volume 60 Issue 2 Pages 84-85
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (1074K) -
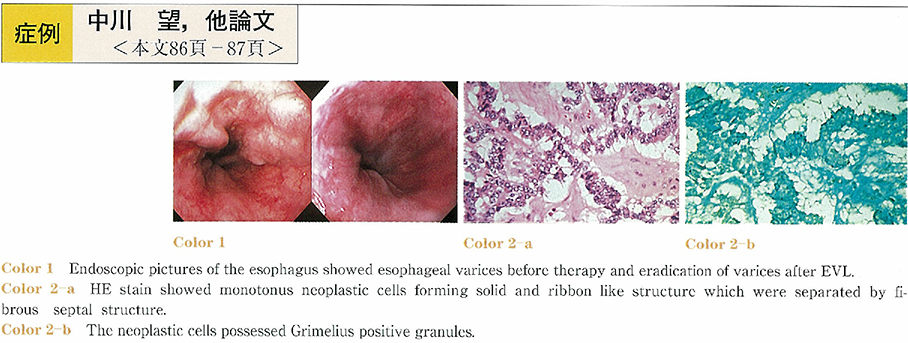
2002 Volume 60 Issue 2 Pages 86-87
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (745K) -
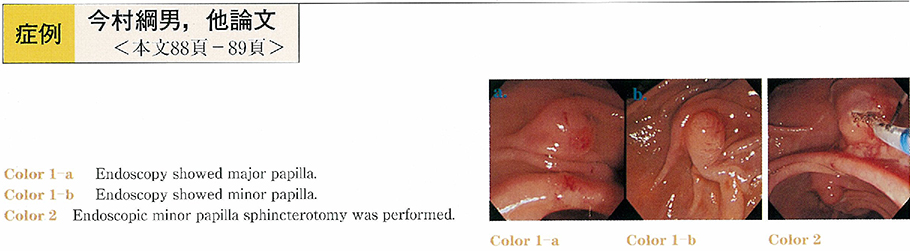
2002 Volume 60 Issue 2 Pages 88-89
Published: June 05, 2002
Released on J-STAGE: May 22, 2014
Download PDF (709K)
- |<
- <
- 1
- >
- >|